


|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Abhinav Humar, M.D.
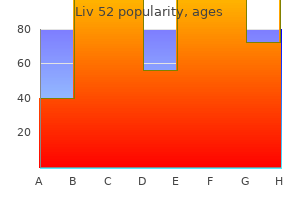
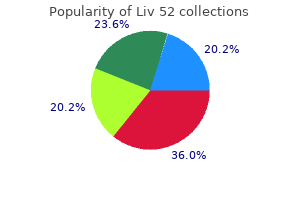
The scope of care treatment ulcerative colitis generic liv 52 100 ml with visa, standardized practices and equipment are specialized for the clinical environment and may differ from those employed during secondary transport symptoms low potassium generic liv 52 100ml mastercard. Prehospital transport typically occurs in the setting of an integrated emergency medical system treatment lichen sclerosis generic 120ml liv 52 otc. Triage decisions regarding the transport destination of a particular patient are important medicine to stop vomiting 100ml liv 52 fast delivery. Available evidence demonstrates improved outcomes for patients triaged to dedicated centers for conditions including trauma medicine 6mp medication buy 100 ml liv 52 visa, acute coronary syndromes and stroke treatment of gout 200ml liv 52 with mastercard. Undertriage, the referral of patients who may benefit from specialized care erroneously to lower acuity centers, may adversely affect outcome. Likewise, over-triage, transferring patients not needing specialized care to dedicated centers, may result in overcrowding and misuse of resources. Controversies remain in several areas of prehospital transport including the benefit of stabilization of patients at the scene via advanced life support ("stay and play") versus rapid transport to an appropriate facility ("scoop and run"). These elements include speed of transport, team composition, team expertise, and appropriate, specific therapeutic interventions. Inter-hospital Transport Interfacility transport is most commonly considered to allow critically ill patients to access a higher level of care or to receive treatment for conditions requiring specific specialty expertise or procedures not available at the referring facility. Considerations for choosing a mode of transport include the urgency of transport, time to mobilize the transport team and vehicles, geographical factors, weather, traffic conditions and cost. In general, ground transport is suitable for many patients and has the advantage of lower cost and is less 43 likely to be affected by inclement weather. Rotary wing transport can be considered for transport distances of 50 to 200 miles and in situations where terrain factors limit ground access. The optimal team composition, team training, skills verification, practice specific algorithms, implementation of crew resource management principles and effect of process improvement initiatives on patient outcome are not well defined. Intrahospital Transport Movement of patients from the intensive care unit to other locations within the hospital is most often performed to obtain diagnostic radiographic studies or for operative procedures. The relative risk of transport should be weighed against the potential benefit derived from the anticipated diagnostic or therapeutic intervention. As discussed previously, a variety of adverse events have been reported during intrahospital transport and this represents an area for potential improvement in patient safety. However, dedicated transport teams may incur increased direct costs to healthcare organizations. Coordination and Communication - Referring physician communicates with accepting physician to confirm acceptance of the patient, availability of required resources and to give detailed report of patient condition. Team Composition - Team composition is variable and often based on patient acuity. Monitoring - Minimum monitoring includes continuous pulse oximetry, electrocardiogram, and regular measurement of blood pressure and respiratory rate. Advanced monitoring including capnography, invasive hemodynamic monitoring and intracranial pressure monitoring can be considered as needed. Equipment - Basic equipment includes airway adjuncts, physiologic monitors, suction, infusion devices and agents for resuscitation and maintenance of vital functions. Consider transport time and potential alterations in airway integrity and gas exchange with transport. An analysis of the reports submitted to the Australian Incident Monitoring Study in Intensive Care. Fanara B, Manzon C, Barbot O, Desmettre T, Capellier G: Recommendations for the intra-hospital transport of critically ill patients. Conclusions Available data suggest that critically ill and injured patients can be transported safely in a variety of transport environments with proper understanding and mitigation of risk. However, the transport environment remains associated with an increased risk for adverse events. Transfer of an unstable patient with urosepsis who is unable to pay for treatment in the emergency department at the referring facility b. Transfer of a patient with an acute coronary syndrome from a regional cardiac center to a nearby community hospital d. Transfer of a trauma patient who has tachycardia and orthostatic hypotension upon arrival to the emergency department of a community hospital 2. Transport ventilators are capable of maintaining the same ventilator parameters as critical care ventilators b. Transport ventilators use special batteries that do not require frequent recharging 46 c. Transport ventilators may prevent harmful hypoventilation or hyperventilation of patients with increased intracranial pressure 3. Patient movement is associated with an increased risk of ventilator associated pneumonia d. Adverse events are rare during intrahospital patient transport 47 Section 6 Cardiopulmonary Resuscitation Key Points: · the 5 criteria defining high quality chest compressions are: adequate rate (100 120/min), adequate depth (2-2. The patient is brought emergently to cardiac catheterization, but no intervention is done due to lack of a defined culprit lesion. Upon rewarming, the patient opens eyes spontaneously, follows commands in all four extremities, and is able to be extubated. The five criteria defining high quality chest compressions are: adequate rate (100 - 120/min), adequate depth (2 - 2. The importance of minimizing interruptions to chest compressions is another emphasis of the 2015 recommendations. Updated guidelines further define and emphasize the importance of high quality chest compressions. Nielsen N, et al: Targeted temperature management at 33°C versus 36°C after cardiac arrest. Epinephrine 1 mg 52 Section 7 Ethics and Organ Donation Key Points: · the four principles of medical ethics are autonomy, beneficence, nonmaleficence, and justice. A family meeting occurs with physicians, nurses, and a social worker to discuss prognosis and goals of care with his wife and daughters. After being updated regarding his overall clinical picture and poor prognosis, his wife makes the difficult decision to withdraw ventilator support, stating that her husband would never have wanted to be kept alive with a ventilator if there was little chance for meaningful recovery. It is determined that the patient can be clinically diagnosed as having "brain death. Ethical issues occur frequently in the intensive care unit, and decision-making during critical illness or at the end of life may pose some of the most complex 53 ethical challenges encountered in medicine. There are four core principles in medical ethics that provide a framework to guide such decision-making: autonomy, beneficence, non-maleficence, and justice. Autonomy is the concept that the patient has the right to self-determination: to choose or refuse treatments when offered. Beneficence is the tenet that providers should always deliver care which is in the best interest of the patient, while nonmaleficence refers to refraining from care that causes harm to the patient. The principle of justice refers to the fair and equitable allocation of resources amongst patients. The concept of medical futility can be an important yet difficult premise to establish when dealing with patients having progressive disease. In such circumstances, the determination of an appropriate treatment and care plan is multifaceted. In assessing individual patients, the provider will want to make sure that the patient can understand the outlined treatment and comprehend the risks and benefits of accepting or rejecting options. These documents - such as a health care proxy, durable power of attorney for health care, and other advance care directives - may give insight to those individuals and the health care team as to what the patient would or would not have wanted. Advance directives include documents like living wills or instructional directives, which can include desire for or against certain interventions. If the patient is deemed not capable of making his or her own decisions and has not previously designated a particular individual for that role, a surrogate decision maker can be identified to be their "voice. Alternatively, once a surrogate decision maker is appointed, conflict may arise when a treatment plan has been decided. Withdrawal of Life Support Whether or not an advance directive is present, a patient or their surrogate decision maker has the right to change their preferences regarding care treatments as their clinical condition changes. Included in this are decisions to withhold and withdraw specific medical interventions. It is important to keep in mind that withdrawal of support is not withdrawal of care. There are often ethical misconceptions about withdrawing or withholding medical support, which include concerns about patient abandonment, violation of the principle of beneficence, or the use of sedatives hastening death. The Principle of Double Effect states that an act which may ultimately have undesirable side effects is permissible if the intended outcome is in itself good, is not intended to do harm, and outweighs the bad. With few exceptions, the majority of states in the United States do not permit physicianassisted suicide. In the United States, there is no ethical difference between withholding or withdrawing treatment. It may, however, be hard emotionally for families to withdraw life support once it has been initiated. Over the years, there have been several public court cases about withdrawal of life-sustaining support such as Karen Ann Quinlan in the 1970s (involving withdrawal of ventilator support) and more recently Terri Schiavo in 2005 (involving withdrawal of nutritional support). These cases among others have set precedents on current ethical standards in clinical practice. Prior to life sustaining therapy being withdrawn, there are several considerations that should be addressed. The family needs to be informed about what to expect, whether that be irregular 55 breathing if taken off of the ventilator or a slower decline if nutritional support is withdrawn. It should be emphasized that pain relief will be a primary consideration and a plan for narcotics or sedative/anxiolytic agents should be available. In many institutions, there are protocols established to guide withdrawal of life support in the most humane way. Ultimately, the amount of time until death after support is withdrawn is difficult to predict. For example, the time to death after withdrawal of mechanical ventilation usually occurs within 24 hours but can range from minutes to days or even longer. In some facilities, a palliative care service is involved as emotional and psychological support and aids in the bereavement process. Clergy and social work should also be involved to provide spiritual and long-term support. Efforts should be made to contact anyone who would have an interest in seeing the patient prior to withdrawal of life support. Documentation of the process is also important and a do-notresuscitate order should be completed. This order will detail what is and is not desired by the family in caring for the patient. This can include the decision to withhold vasoactive medications for blood pressure support, intubation with mechanical ventilation, or cardiopulmonary resuscitation, specifically chest compressions or defibrillation. End-of-Life Care and Organ Donation: An evolving area of interest involves the care for potential organ donor patients. Often these patients require aggressive interventions, which may offer no direct benefit to the patients themselves, in order to preserve organs for transplantation. There are currently two accepted classifications of deceased donors: heartbeating organ donation requires determination of death based on irreversible cessation of entire brain function, including the brain stem (donation after brain death), while non-heart-beating organ donation (donation after cardiac death) requires the determination of death based on irreversible cessation of circulatory and respiratory function without antecedent brain death. Families may or may not elect to be present at the time of withdrawal of life support. If the family chooses to be present, life support will usually be withdrawn in an induction room where the family may say goodbye after death. A patient is pronounced dead if after five minutes there is an absence of circulation, along with apnea, unresponsiveness, and asystole on 56 electrocardiograph. Once death is certified, the patient is moved to the operating room where organ procurement takes place. No organs can be procured until a physician who is not involved with the transplantation service has certified death. Often the goal of organ preservation requires aggressive interventions such as mechanical ventilation, hemodynamic support, and medication administration, which may not offer any direct benefits to the dying patient. The patient and their family may view such interventions as a sharp contrast to their cultural and religious beliefs. Unfortunately, care providers may unintentionally cause pain and suffering to their patients and their families. The ultimate safeguard in protecting the patient and care providers from this potential conflict is informed consent. An ethically valid informed-consent process should consist of a balanced discussion of the available options and counseling to help patients and their families reach the choice that is best for them. It is recommended that the conversation regarding organ donation and end-of-life care be approached early in the treatment course and with a team of care providers. Step one recommends ongoing resuscitation and life support to preserve organs until procurement staff can determine the medical suitability of potential donors. Step two of the Uniform Anatomical Gift Act states that consent is required before organs may be removed. Although legally appropriate to proceed with organ procurement in the setting of first-person consent, it is strongly advised that the family be closely involved in the discussion to mitigate any potential conflicts. If appropriate consent is obtained, critical care professionals should begin to transition the goals of care. Any potential organ donor has the right to comfort measures and all attempts should be made to provide this support, whether or not they may become donors. Additionally, support should be provided to the families of potential organ donors, including pastoral care, social work, and palliative care staff. A multidisciplinary approach to the end-of-life care for potential organ donors often provides the best care for all parties involved. As medicine evolves, the opportunities for potential organ transplantation continue to increase. Organ donation can be a wonderful gift allowing those at the end of their life to extend the lives of others and can offer families the closure that something positive has come from their loss.
A subconjunctival injection of gentamicin and dexamethasone is given postoperatively medicine definition cheap liv 52 200 ml with mastercard. The pupil is kept dilated with short acting mydriatic and topical steroidantibiotic drops are applied several times each day for 2-3 weeks medicine expiration generic liv 52 200ml with mastercard. Posterior capsular opacification-This is almost universal if the posterior capsule is retained symptoms xanax overdose buy liv 52 120 ml mastercard. The incidence is reduced when posterior capsulorhexis is combined with vitrectomy treatment jaundice buy discount liv 52 200 ml line. Proliferation of lens epithelium is common but may not be visually significant if visual axis is not involved treatment 2 go liv 52 200ml cheap. Lensectomy In this operation symptoms 1 week before period buy generic liv 52 120ml online, the lens including anterior and posterior capsule along with anterior vitreous are removed with the help of vitreous cutter, infusion and suction device. Indication · All cataracts occuring in childhood both congenital or acquired are easily treated by this procedure. A well constructed sclera tunnel may not require suturing, but placement of one horizontal suture (with 10-0 nylon) ensures wound stability and reduces postoperative astigmatism. Spectales-They are useful for older children with bilateral aphakia but not for unilateral aphakia. Contact lenses-These are superior optical solution for both bilateral and unilateral aphakia iii. Etiopathogenesis · Heredity play an important role and it may appear at an earlier age in successive generations. Formation of aberrant lens fibres-These are produced when the germinal epithelium of lens loses its ability to form normal fibres as happens in posterior subcapsular cataract. Abnormal product of metabolism, drugs or metals can be deposited in storage diseases (Fabry), metabolic diseases (Wilson) and toxic reactions (siderosis). The Lens 213 Classification Morphologically, the senile cataract occurs in two forms: 1. It is common to find cortical and nuclear senile cataracts co-existing together in one eye. In general, the relative frequency of cunieform cataract is 70%, nuclear 25% and cupuliform cataract is 5% approximately. Any physical or chemical factor which disturbs the intra and extracellular equilibrium of water and electrolytes causes opacification of lens. Hydration-It occurs due to osmotic changes and changes in the semipermeability of lens capsule. Denaturation and coagulation of proteins-It leads to the formation of dense, irreversible lenticular opacity. Frequent changes of glasses occur due to rapid change in the refractive index of lens. Monocular diplopia or polyopia-It is common in cortical spoke - like (cuneiform) opacities along with clear water clefts. Coloured halos around light are seen due to presence of irregular refractive index in different parts of the lens. Cupuliform cataract Clinical Stages In senile cortical cataract presenile changes are the rule. Grey appearance of pupil-It is due to increase in the refractive index of the cortex and due to increased reflection and scattering of light. Lens striae-The wedge-shaped or spokes-like opacities (Cuneiform opacities) appear in the periphery of the lens with clear areas in between. Progressive hydration causes swelling of the lens, making the anterior chamber shallow. Immature cataract-When there is clear lens substance between the pupillary margin and the opacity, the iris throws a semilunar shadow on the deeper lens opacity. The iris shadow is absent as iris is separated by only lens capsule from the opaque lens. Nucleus-It is small, brownish and sinks by gravity in the bag of liquefied cortex (Morgagnian cataract). Later on Hypermature morgagnian cataract fluid cortex may get absorbed due to leakage resulting in the formation of membranous cataract with a very small nucleus. Iridodonesis-There is tremulousness of iris as its support is lost due to shrinkage of lens. Phacolytic glaucoma may occur due to leakage of lens protein which is ingested by the phagocytes. These large Hypermature cataract phagocytes obstruct the angle of anterior chamber. Phacoanaphylactic uveities-Lens protein may leak into the anterior chamber which act as antigens causing antigen antibody reaction leading to uveitis. There is dense aggregation of opacities just beneath the capsule usually in the posterior cortex. There is marked impairment of vision due to the opacity being near the nodal point of the eye. There is loss of ability to see objects in bright sunlight or being blinded by light when driving at night. Etiology There is slow sclerosis of the nucleus due to long-term effect of the ultraviolet irradiation. Black cataract (Cataracta brunescens)-The nucleus becomes diffusely cloudy and dark. It may become brown, dusky red or black occasionally due to deposition of melanin pigment derived from amino acids in the lens. Mature cataract-The sclerosis extends upto the capsule and the entire lens functions as a nucleus. There is change in refractive index of the nucleus which causes index myopia, resulting in improvement of near vision. Colour shift-The blue end of the spectrum is absorbed more by the cataractous lens. Ophthalmoscopic examination-The details of the fundus cannot be seen due to hazy media. Etiology There is disturbance to the nutrition of the lens due to the inflammatory or degenerative diseases of the other parts of the eye. Symptom There is markedly impaired vision due to presence of opacity near the nodal point in the posterior cortex. Posterior segment diseases · It causes characteristic posterior cortical cataract. Ophthalmoscopic examination-Vaguely defined, dark area is seen in the posterior cortex against red background. True diabetic cataract is a rare condition occurring typically in young persons due to acute diabetes. When blood sugar levels are elevated beyond 200 mg per ml, excess glucose is converted to sorbitol. Clouds of small discrete opacities appear in the cortex, separated from the capsule by a clear zone. It causes bilateral cataract typical (oil drop cataract) due to inborn inability to metabolize galactose. Chlorpromazine, Busulphan, Amiodarone, Gold and Allopurinol are the other drugs associated with cataract. Irradiation-Irradiation by X-ray, -rays and neutrons results in formation of posterior cortical cataract near posterior pole. Ultrasonic radiation-Lens opacities are formed due to heat and concussion produced by ultrasonic radiation. It is the excessive awareness of light, such as direct sunlight or headlights of an oncoming motor vehicle. Commonly occurs with posterior subcapsular cataract due to excessive irregular scattering of light. They can be easily differentiated from muscae volitantes in the vitreous which are mobile. Coloured halos are seen due to hydration of the lens which results in irregularity in the refractive index of different parts of the lens. Posterior cortical cataract-Visual loss is out of proportion to the size of opacity as it is close to the nodal point. Nuclear sclerosis-There is progressive myopia so the presbyopic person gets "second sight" or "improvement" in vision without the glasses. Mature cataract-The vision is grossly reduced to counting fingers at few cm or hand movement or perception of light with good projection of rays. Plane mirror examination at a distance of 22 cm (distant direct ophthalmoscopy)-The exact position of the opacity is determined by parallactic displacement. Direct ophthalmoscopy-The surgeon looks through a self-luminous ophthalmoscope and directs the light upon the pupil. Cataract-Acquired, congenital, after cataract Glaucoma-Open angle glaucoma, chronic congestive glaucoma Refractive errors-Myopia, hypermetropia, astigmatism Uveitis and its complications-Chronic iridocyclitis, secondary glaucoma, complicated cataract, choroiditis, etc. Phacoanaphylactic uveitis-In hypermature cataract lens proteins may leak into anterior chamber. These may act as antigens and induce antigen-antibody reaction leading to uveitis. Lens-induced glaucoma-It may occur due to an intumescent lens (phacomorphic glaucoma) or due to leakage of proteins into the anterior chamber from an hypermature cataract (phacolytic glaucoma). Subluxation and dislocation of lens may occur due to degeneration of zonules in hypermature stage. Examination of the eye is done carefully specially in cases of complicated cataract. Systemic examination is done for diabetes, hypertension, ischaemic heart disease and gross focal sepsis. When fundus cannot be seen, the following tests are done to find out the condition of posterior segment, I. Light is thrown from various directions and the patient points the correct direction. Two point discrimination test-Patient looks through an opaque disc perforated in the centre with two pinholes close together. Entoptic view of the retina-The eyes are closed and globe is firmly massaged through the lower lid with a bare lighted bulb of a torch. Ultrasonic investigation by B-scan-Retinal detachment and vitreous pathology may be detected. Laser interference fringes-Postoperative visual acuity is assessed by focusing light beams from two sources (helium-neon) which overlap equally posterior to the plane of the lens. Photo stress test-The eye is exposed to bright light for 15 seconds and recovery time is noted. A visual acuity of 6/12 or 6/18 with accommodation is considered better than 6/6 without accommodation. Phacolytic glaucoma-It results due to leakage of lens protein (hypermature cataract). Phacomorphic glaucoma-The swollen lens pushes the iris forwards (intumescent stage). Retinal diseases like diabetic retinopathy or retinal detachment, treatment of which cannot be done in presence of cataract. Surgical Treatment the technique of cataract extraction has changed drastically in recent years due to the introduction of operating microscope and intraocular lens implant. However, the modern trend is in favour of extracapsular lens extraction along with intraocular lens implantation. This reduces the incidence of vitreous loss to the minimum with superior visual results. In elderly persons the nucleus is hard and it can be removed by the following methods: 1. The choice of a particular surgical technique depends upon the following factors: 224 Basic Ophthalmology 1. Prophylactic antibiotics-Local and systemic broad-spectrum antibiotics should be started at least one day prior to surgery. The pupil is dilated with a combination of medications which include topical cycloplegics which paralyze the sphincter pupillae (cyclopentolate, tropicamide or homatropine drops), mydriatics which stimulate the dilator pupillae (phenylephrine) and nonsteroidal anti-inflammatory agents (diclofenac or ketorolac). The latter inhibit prostaglandin release from the iris on mechanical stimulation during surgery and prevent intraoperative miosis. Anaesthesia and akinesia-Most of the cataract surgery is done under local anaesthesia except in children and uncooperative patients. Topical anaesthesia with paracaine or 2% lignocaine jelly supplemented with intracameral injection of preservative free lignocaine, if required, provides only anaesthesia and is being increasingly used for phacoemulsification surgery. The facial nerve is paralysed so that the patient is unable to squeeze the eyelids during operation due to orbicularis oculi muscle paralysis. Van Lints method-Local anaesthetic is injected near the outer canthus of the eye. Ciliary block by retrobulbar injection 1-2 cc of anaesthetic is injected into the neighbourhood of ciliary ganglion behind the eyeball. It causes anaesthesia of deeper structures like iris and lowers the intraocular pressure. It is associated with risk of causing retrobulbar haemorrhage and bulbar penetration. The patient looks up straight at the ceiling and 5 ml of local anaesthetic is injected from the lateral part of the lower lid. The anaesthetic infiltrates into the retrobulbar space by the application of superpinkie ball (30 mm Hg pressure) for 15-20 minutes. Complications of anaesthesia include: · Retrobulbar or peribulbar haemorrhage · Accidental globe perforation · Accidental injection into optic nerve sheath with intracranial spread · Anaphylactic shock · Vasovagal reflex resulting in collapse and death. Ocular hypotony-In most cases hypotony is achieved by the application of superpinkie ball or manual pressure.
Speech-Language Pathology Medical Review Guidelines 17 Audiologic Rehabilitation or Auditory Rehabilitation (See also Hearing Disorder) Audiologic rehabilitation assessment is provided to evaluate the impact of a hearing loss on communication functioning (strengths and weaknesses) symptoms 7dpiui order liv 52 100 ml overnight delivery, including the identification of speechlanguage-communication impairments treatment varicose veins best liv 52 120 ml. Treatment Treatment is provided to improve the communication abilities of an individual with a hearing loss treatment zap generic 120 ml liv 52 with mastercard. Treatment focuses on comprehension and production of language in oral symptoms 7 weeks pregnant cheap liv 52 100ml without a prescription, signed symptoms to diagnosis buy generic liv 52 120ml on line, or written modalities; speech and voice production; auditory training; speech reading; multimodal medicine pouch buy discount liv 52 100ml line. The brain identifies sounds by analyzing their distinguishing physical characteristics (frequency, intensity, and temporal features). Both audiologists and speech-language pathologists play a role in (central) auditory processing evaluation and treatment. Treatment Two general treatment approaches have been used for (central) auditory processing problems. Speech-Language Pathology Medical Review Guidelines 18 Cognitive-Communication Treatment (Cognitive Deficits, Cognitive Rehabilitation; See also Cognitive-Communication Disorder) Intervention services are provided to individuals with cognitive-communication disorders, including problems in the ability to perceive, attend to , organize, and remember information; to reason and to solve problems; and to exert executive or self-regulatory control over cognitive, language, and social skills functioning. Treatment Assessment identifies the specific deficits along with preserved abilities and areas of relative strength in order to maximize functional independence and safety, and to address the deficits that diminish the efficiency and effectiveness of communication. Intervention may focus on developing compensatory memory strategies, formal problem-solving strategies and their application to functional activities, and improving attention at various levels of complexity. Treatment may focus on improving the processing of varied types of information, including verbal, non-verbal, and social cues. Fluency Treatment (Stuttering, Cluttering; See also Stuttering and Cluttering Disorder) Fluency assessment is provided to evaluate aspects of speech fluency (strengths and weaknesses), including identification of impairments. Elicitation and use of prognostic information and information that optimizes treatment planning may be addressed. Speech-Language Pathology Medical Review Guidelines 19 Treatment Fluency intervention is provided to improve aspects of speech fluency and concomitant features of fluency disorders in ways that optimize activity/participation. This may include: reducing the severity, duration, and abnormality of stuttering-like dysfluencies in multiple communication contexts reducing avoidance behaviors removing or reducing barriers that create, exacerbate, or maintain stuttering behaviors. Some individuals with fluency disorders participate in intensive residential treatment programs. More often, individual treatment sessions are offered by hospital and community outpatient clinics and private practitioners. Language Treatment (Receptive, Expressive, Pragmatics or Social Communication, Reading, Writing; See also Language Disorder) Individuals receive intervention services for language impairment when their ability to communicate effectively and to participate in social, educational, or vocational activities is impaired because of a spoken and/or written disorder. Treatment Language intervention for language impairment addresses knowledge and use of language for listening, speaking, reading, writing, thinking, reasoning, and social communication, including: phonology and print symbols (orthography) for recognizing and producing intelligible spoken and written words syntactic structures and semantic relationships for understanding and formulating complex spoken and written sentences discourse structures for comprehending and organizing spoken and written texts pragmatic conventions (verbal and nonverbal) for communicating appropriately in varied situations. Speech-Language Pathology Medical Review Guidelines 20 Myofunctional Treatment (Tongue Thrust; See also Myofunctional Disorder) Myofunctional disorder is a disorder of tongue and lip posture and movement. Speech misarticulations can cooccur with this condition in some patients and treatment would include correction of speech sound errors. Treatment Depending on assessment results, intervention addresses the following: alteration of lingual and labial resting postures muscle retraining exercises modification of handling and swallowing of solids, liquids, and saliva speech sound production errors, if present. Neurological Motor-Speech Treatment Neurological motor speech assessment looks at the structure and function of the oral motor mechanism for non-speech and speech activities including assessment of muscle tone, muscle strength, motor steadiness and speech, range, and accuracy of motor movements. Treatment Depending on assessment results, intervention addresses the following: 1. Including direct behavioral treatment techniques, use of prosthetics, or appropriate referral for medical-surgical or pharmacologic management. Social Communication Treatment (See also Language Treatment, Social Communication Disorder) Social communication treatment is provided to individuals who have difficulty with social interactions and whose ability to communicate effectively and to participate in social, educational, or vocational activities is impaired. Body language, facial expression, emotional understanding, speech style, social reasoning, and making inferences are examples of elements of social communication. Standardized assessment, parent reports, and observation may all be used to evaluate social communication skills. Treatment may focus on a prompting strategy used to teach individuals to use a variety of language during social interactions, or use of social skills groups to teach ways of interacting appropriately with typically developing peers through instruction, role-playing, and feedback. Stories to explain social situations to individuals and to help them learn socially appropriate behaviors and responses may also be used in treatment. For more information on social communication disorders, treatment, and the role of the speech-language pathologist, go to Speech Sound Disorders Treatment (Articulation Disorder Treatment, Phonological Process Disorder Treatment) Speech sound disorders treatment focuses on correct speech sound production. Speech sound impairments may arise from problems with articulation (making sounds) and phonological processes (sound patterns). Treatment Articulation disorders treatment may involve demonstrating how to produce a sound correctly, learning to recognize which sounds are correct and incorrect, and practicing sounds in different Speech-Language Pathology Medical Review Guidelines 22 words. Phonological process disorders treatment may involve teaching the rules of speech to individuals to help them say words correctly. Depending on assessment results and age of the patient, intervention addresses the following: selection of intervention targets based on the results of an assessment of articulation and phonology improvement of speech sound discrimination and production general facilitation of newly acquired articulation and/or phonological abilities to a variety of speaking, listening, and literacy-learning contexts increased phonological awareness of sounds and sound sequences in words and relating them to print orthography (when age-appropriate). Swallowing Treatment (See also Dysphagia, Swallowing Disorder) Swallowing treatment is provided to prevent nutrition and hydration problems and pulmonary complications of aspiration and to improve functional feeding/swallowing skills. The speechlanguage pathologist performs clinical and instrumental assessments and analyzes and integrates the diagnostic information to determine candidacy for intervention as well as appropriate compensations and rehabilitative therapy techniques. A swallowing evaluation assesses oral, pharyngeal, and related upper digestive structures and functions to determine swallowing functioning and oropharyngeal/respiratory coordination (strengths and weaknesses), including identification of impairments and assessment of the ability to eat safely and to sustain adequate nutrition and hydration. Swallowing and feeding disorders occur with multiple medical diagnoses across the age spectrum from premature infants to geriatric adults. Treatment Intervention may address the following: No oral presentation of food or liquids. Oral presentation of foods or liquids that may be of specified volume and/or consistency. Techniques to improve oral, pharyngeal, and laryngeal coordination, control, speed, and strength. Facilitate coordinated movements of the oral/pharyngeal mechanism and respiratory system. Techniques for modifying behavioral and sensory issues that interfere with feeding and swallowing. Structural assessment of face, jaw, lips, tongue, teeth, hard and soft palate, oral pharynx, and oral mucosa. Functional assessment of physiologic functioning of the muscles and structures used in swallowing, including observations of symmetry, sensation, strength, tone, range and rate of motion, and coordination or timing of movement. Note: Direct observations of the pharynx (other than the oral pharynx) and larynx are not possible without instrumentation. Functional assessment of actual swallowing ability, including observation of sucking, mastication, oral containment and manipulation of the bolus; impression of the briskness of swallow initiation; impression of the extent of laryngeal elevation during the swallow; and signs of aspiration such as coughing or wet-gurgly voice quality after the swallow. Impression of adequacy of airway protection and coordination of respiration and swallowing. Assessment of saliva management including frequency and adequacy of spontaneous swallowing and ability to swallow voluntarily. Structural assessment, including observation of face, jaw, lips, tongue, teeth, hard palate, soft palate, larynx, pharynx, and oral mucosa. Functional assessment of physiologic functioning of all the muscles and structures used in swallowing, including observations and measures of symmetry, sensation, strength, tone, range and rate of motion, and coordination or timing of movement. Also, observation of head-neck control, posture, developmental reflexes, and involuntary movements. Functional assessment of actual swallowing ability, including observation of sucking, mastication, oral containment and manipulation of the bolus; briskness of swallow Speech-Language Pathology Medical Review Guidelines 24 initiation; lingual, velopharyngeal, laryngeal, and pharyngeal movement during swallowing; coordination and effectiveness of these movements. Assessment of adequacy of airway protection; assessment of coordination of respiration and swallowing. Assessment of the effect of intubation on oropharyngeal swallowing (feeding tube, tracheostomy) and the effect of mechanical ventilation on swallowing. Assessment of the effect of changes in bolus size, consistency, or rate or method of delivery on the swallow. For pediatric patients, instrumental diagnostic procedures that are age-appropriate with regard to positioning, presentation. The final analysis and interpretation of an instrumental assessment should include a definitive diagnosis; identification of the swallowing phase(s) affected; and a recommended treatment plan, including compensatory swallowing techniques and/or postures and food and/or fluid texture modification. An instrumental assessment is not indicated if findings from the clinical evaluation fail to support a suspicion of dysphagia, or when findings from the clinical evaluation suggest dysphagia but include either of the following: (1) the patient is unable to cooperate or participate in an instrumental evaluation or (2) the instrumental examination would not change the clinical management of the patient. The effects of compensatory maneuvers and diet modification on aspiration prevention and/or bolus transport during swallowing can be studied radiographically to determine a safe diet and to maximize efficiency of the swallow. Detailed information regarding swallowing function and related functions of structures within the upper aerodigestive tract are obtained. The sensory evaluation is completed by delivering pulses of air at sequential pressures to elicit the laryngeal adductor reflex. Individuals of all ages are treated on the basis of swallowing function assessment. At the conclusion of the assessment, the presence, severity, and pattern of dysphagia should be determined, and recommendations made with collaboration among the therapist, physician, and patient/family. Voice and/or Resonance Treatment (See also Voice and/or Resonance Disorder) Voice treatment is provided for individuals with voice disorders, alaryngeal speech, and/or laryngeal disorder affecting respiration. Intervention is conducted to achieve improved voice production, coordination of respiration and laryngeal valving, and/or acquisition of alaryngeal speech sufficient to allow for functional oral communication. Resonance and nasal airflow assessment is provided to evaluate oral, nasal, and velopharyngeal function for speech production (strengths and weaknesses), including identification of impairments, associated activity, and participation limitations. Intervention is conducted to achieve improved resonance Speech-Language Pathology Medical Review Guidelines 26 and nasal airflow and improved articulation sufficient to allow for functional oral communication. Treatment Research data and expert clinical experience support the use of voice therapy in the management of patients with acute and chronic voice disorders (for details on voice treatment, see Voice and/or Resonance Disorder). Intervention focuses on proper use of respiratory, phonatory, and resonatory processes to achieve improved voice production and coordination of respiration and laryngeal valving, with appropriate treatment to enhance these behaviors. Treatment is also provided for individuals with resonance or nasal airflow disorders, velopharyngeal incompetence, or articulation disorders caused by velopharyngeal incompetence and related disorders such as cleft lip/palate. Additionally, treatment includes patient-directed selection of preferred alaryngeal speech communication means, including development of one or more of the following alaryngeal alternatives: esophageal speech, artificial larynx speech, or tracheoesophageal prosthesis speech. Intensive Voice Treatment Model For patients with voice and airway disorders, speech-language pathologists traditionally provide weekly or biweekly treatment. However, different protocols used in intensive voice treatment programs may produce better results for patients who cannot adhere to that schedule or for whom traditional treatment has proven unsuccessful. For example, in the voice and swallowing clinics at the University of Wisconsin-Madison, Division of OtolaryngologyHead and Neck Surgery, an intensive voice treatment approach has been successful. For more information on this intensive treatment model, see Voice Boot Camp at leader. Aerodynamic testing assesses average airflow, peak airflow, vocal efficiency, and subglottal pressure. Acoustic tests include pitch, loudness, jitter, shimmer, signal-to-noise ratio, and spectral analysis. Instrumental techniques ensure the validity of signal processing, analysis routines, and elimination of task or signal artifacts. Videostroboscopic laryngoscopy incorporates a stroboscope, laryngeal fiberscope, and a videoscope to produce a permanent image of the motion of the vocal folds. Videostroboscopy is a diagnostic procedure for examination of the vocal cords when pathology is suspected (based on persistent symptoms or other findings with suspected pathology such as carcinoma, vocal cord paralysis, or polyps) despite negative or unsatisfactory/inadequate mirror-image and endoscopic examinations. If a cleft palate/craniofacial team is involved, for example, team members will have access to: a nasometer that analyzes acoustic energy emitted through the oral cavity and nasal cavity during the production of speech aerodynamic assessment, measuring oral pressure and oral airflow during speech, and estimating the size of the velopharyngeal gap/orifice nasopharyngoscopy (a procedure using a flexible fiberoptic nasopharyngealscope) to visualize the velopharyngeal mechanism and its function by viewing the nasal surface of the velum and the velopharyngeal port during connected speech videofluoroscopy and lateral cephalographs to assess velopharyngeal closure during speech and phonation, respectively. Speech-Language Pathology Medical Review Guidelines 28 Prosthetics Intervention services are conducted to help individuals to understand, use, adjust, and restore their customized prosthetic/adaptive device. Prosthetic/adaptive device interventions include fitting, orientation, modification, and repair. Tracheostomy speaking valves such as the Passy-Muir valve are considered voice prosthetics that enable the wearer to produce speech. With potential for a tracheostomy tube to be in place for an extended period of time, these children may be at risk for long-term disruption to normal speech development. As such, speaking valves that restore more normal phonation are often key tools in the effort to restore speech and promote more typical language development in this population. Tracheotomized patients, both adults and children, use tracheostomy speaking valves. Laryngeal implants are devices used to restore voice when the larynx is damaged or paralyzed, precluding speech production. They are implanted into a vocal fold or laryngeal vestibule to allow for precise, easily adjustable control of vocal cord medicalization to approximate a natural voice. For patients with respiratory insufficiency, the speech-language pathologist can teach phrasing to promote energy conservation. Submaximal tongue strengthening exercises and diaphragmatic exercises also can be taught to help improve articulation and voice projection. Patients should be monitored, and as their speech declines, the speech-language pathologist may introduce augmentative communication devices, such as writing implements, communication boards, or computer-assistive technology. For those with severe bulbar and limb involvement, eye gaze and blink generally are preserved. Therefore, the speech-language pathologist can take advantage of these preserved functions by introducing blink controlled voice synthesizers, communication boards, and computer assistive devices that utilize eye gaze techniques (Shannon & Bockenek, 2009). Aphasia Aphasia is a language disorder that results from damage to portions of the brain that are responsible for language. All aspects of language (speaking, writing, reading, and Speech-Language Pathology Medical Review Guidelines 33 understanding) may be affected to some degree. Aphasia may co-occur with speech disorders such as dysarthria or apraxia of speech. The nature and severity of aphasia will vary from individual-to-individual as will the treatment plan and approaches used.
Buy liv 52 200ml otc. Ayushman Bhava : Dengue Fever | डेंगू बुखार.
Diseases