




|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Richard A. Lange, MD
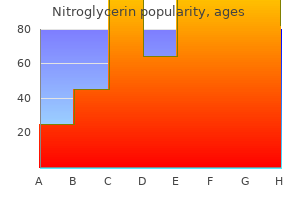
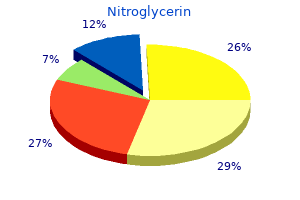
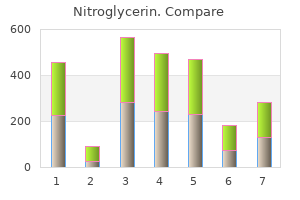
One of the biggest fallacies is that veterinarians are well loved and getting into vet school is the hardest part treatment 0f gout buy discount nitroglycerin 6.5mg. Love and throat punches; Practice managers and bosses: It is your circus and these are your monkeys medications an 627 quality 6.5 mg nitroglycerin. Having to have everything you do fit into this passion mindset is unrealistic and elitist treatment 5th metatarsal shaft fracture generic 2.5mg nitroglycerin. While the overall growth in revenue and visits in 2016 and 2017 was good to see treatment 6 month old cough nitroglycerin 6.5mg visa, there are still some concerning trends medicine 93 generic nitroglycerin 2.5mg free shipping. There have also been a number of studies done in the last few years that provide some insights into what clients want; perhaps one of the most intriguing was released several years ago by Banfield symptoms of breast cancer cheap 2.5 mg nitroglycerin. In the past few years Banfield has harnessed the power of their incredibly large data base and published several reports documenting a decline in pet health. In 2015, they did something a little different; they focused on what pet owners are saying about their pets and their related needs. But instead of doing this via a traditional survey of pet owners, they took to the internet and spent over a year reviewing 2 million plus online conversations posted to blogs, forums and other social communities with the idea that in this kind of environment, pet owners would be more likely to talk about what they really think about their relationship with their veterinarian and their needs related to pet care. What do practice teams need to focus on to build and reinforce the bond with clients? Driving clients crazy mistake #1: Ignoring the cost of veterinary care the cost of owning a pet and the cost of veterinary care are recurring themes in studies of pet owners and one of the most important issues practices need to focus on. Clients are dealing with the increasing costs of veterinary care resulting from the availability of more sophisticated medical options, the extended life span of pets which results in more routine care spending as well as an increased likelihood of the pet developing a serious and/or chronic disease and fee increases well above the rate of inflation. Even clients who are fully committed to providing quality care are pushing back at cost and looking for alternatives. But there are things we can do to make it easier for clients to take care of their pets; these include: · Use a well thought out price-setting process that focuses on value to the consumer · Understand who your customers are, what their financial position is and what they want from their veterinary practice · Better educate pet owners about payment alternatives offered in the practice Driving clients crazy mistake #2: Not giving pet owners the information they want Research has shown that the information that pet owners want and the items the veterinary team want to discuss are often different. What is 417 one thing everyone can do to make sure pet owners get their questions answered? Asking, at multiple times during the visit, is what is important: · What else is going on with Fluffy that you have questions about? In other words, statistical probability of risk, while important to know, is usually not enough to motivate clients to change from the known and familiar course of action. Clients need to know that the recommendation made by the veterinary team will work; that they can do their part. Driving clients crazy mistake #3: Making generic recommendations Pet owners want care recommendations that are personalized to their situation. While many of the recommendations the practice team makes may be the same for most dogs or cats, there are some that should be different based on breed and pet lifestyle considerations. And each of these client requests is very reasonable compared to what they see in other well-run businesses. Practices need to focus on providing to pet owners what pet owners want, not what we want them to want. Driving clients crazy mistake #5: Poor client service Client service is a joke in many businesses these days. They want their experience at the veterinary practice to be easy, relatively quick, be reasonably priced in comparison to the value and not leave them cross and annoyed at the end because of some expectation that went unfulfilled. A very interesting article ("Clueing in Customers"-Berry & Bendapudi-2003) in the Harvard Business Review about the Mayo Clinic reiterates this point. They got there not only by providing great medicine but also by focusing on the client experience, not just the medicine. They recognize that medical care is frightening and complicated and do everything they can to ease the patients concerns. Client service is also about how the pet gets treated and how the pet owner perceives that treatment. Most cats and a surprising number of dogs get very stressed when they visit a veterinary practice. Stressed pets lead to stressed owners and a decline in the 418 number of visits and the care these pets get. Practices need to focus on things that can be done to de-stress the visit both for pets and their owners; some examples include: separate entrances or waiting areas for cat owners and dog owners, a calming environment, "cat only" appointment times, house-calls, a greater use of sedatives before and during the visit and gentle control techniques. Unless you explain it in words of one syllable, the client may not understand or appreciate the efforts. Periodic review of discount programs and ongoing medical record audits are essential to managing both discounts and missed charges. It may be a partial discount or a 100% discount - either way the practice owner, the doctor on the case or a staff member is consciously deciding to reduce the fee for the services that the client received. Random discounts, however, are another story-these are the discounts doctors and team members give for no reasonable purpose. While the bottom line impact on profitability is the same with either discounts or missed charges, it is important to understand what is causing the revenue drain because the corrective action is different for each category. First of all because both discounts and missed charges can have a huge impact on practice profitability. Secondly it takes a disproportionate number of additional appointments to make up for the profits lost through either a discount or a charge that is not entered into a client invoice. And, of course, profits are what allow a practice to invest in new equipment and improved facilities, offer raises and additional benefits to team members, and provide better pet care. This may not seem to be such a large number but it is critical to remember that the total amount of discounts in many practices is often significantly higher because most discounts are not entered as such on the client invoice and thus are not tracked by the software system. In reality, the amount of discounts and missed charges in a typical practice is often much higher than the 2. A medical record audit is the only way to insure a practice finds all discounts not recorded in the invoicing software and all missed charges. To start, pull the medical records for 40 cases per doctor-this should be a mix of initial appointments, rechecks, and hospitalized cases. Compare the services provided to the client as documented in the medical record with what was charged on the invoice. Capture the results of the audit on a chart or a spreadsheet with the following items included: patient name, date and time of appointment, amount of invoice, type of appointment (surgery, hospitalization, outpatient), doctor, date, nurse (if known), receptionist (if known) and information about the discounted or missed charges (procedure performed, correct fee, actual fee charged, amount missed or discounted and whether or not a discount was part of a formal discount program the practice offers). Once the amounts discounted or lost are calculated for this sample, they can be extrapolated to the total practice revenue for an estimate of the total lost in a month or a year. E $211,000 X 10% = $21,100 the total amount lost is $102,540 or 9% of total revenue. After calculating the total amounts lost, discounts and missed charges should be separated for further analysis. Veterinary practices generally have three kinds of discount programs: employee benefits, marketing programs, and charitable contributions to the community. In addition, they often have a large amount of random, unplanned discounts that doctors or staff give simply because they are uncomfortable with the fee structure or are just nice people. It is critical that the practice periodically review all discounts and make sure they are still accomplishing the intended goal, if there was a particular goal in the first place. Many businesses effectively use discounts to bring in clients for a particular service or during a slow time of the day or year. Common ones include those for senior citizens, multiple pets, breeders, and bundled services. Then take a look at each program individually; for example, if the practice gives a free exam to everyone who purchases a puppy at a local pet store in order to build its client base, is this really working? These clients should be tracked over time to see if they remain with the practice and they brought in enough revenue to warrant the discount. All formal discounts offered by the practice should be reviewed periodically and tracked over time to see if they are effective in bringing in new clients and/or enticing old clients to come in more frequently or buy more services. The questions to be asked when reviewing these discounts are: · Are the benefits competitive with other practices? Whether or not to continue offering these discounts is a question to be considered in a similar fashion to the offering of any other employee benefit. Some practices give charitable discounts to animal welfare organizations or individuals who provide care to stray animals. The amount of charitable contributions given by a practice is at the discretion of the practice owner. The owners are truly the only people in the practice with the right to determine if those discounts are too much. Owners, of course, must understand the financial impact of these discounts when making that decision. The last kind of discount is the random discount; that given for no particular reason. Once the random discounts have been identified, it is important to search for patterns. Once the root cause has been identified, steps can be taken to correct the problem. The policy should very clearly state that employees are expected to charge the fees set by the practice and list the discounts that can be given and who can authorize them as well as any limitations. Practice owners and managers need to share the policy with all team members regularly and make it clear to employees that part of their job is to charge appropriate fees. Review missed charges and discounts given per doctor or other team member on a regular basis. Use this information to identify holes in the system that need to be plugged or individuals who need to be counseled about too many discounts given. Train these employees in the importance of accurate invoices and how to appropriately use the fee schedule. Simplify the fee schedule so there are fewer choices by reducing the number of service categories and the number of individual services. Use the same prices for services that are essentially the same; for example a short in-patient hospital exam and a short medical recheck exam. If one is priced less than the other, it will inevitably be selected more frequently. Review miscellaneous charges and overrides on a frequent basis; these may be used to give away services at a price less than that which should be charged. Educate employees about the importance of profitability and the impact of inappropriate discounts. It is more difficult to justify high fees if the practice in question has fees that are much higher than others in the community or it is not readily apparent what is better about this practice compared to others. Non-owners are also more accepting of the level of fees charged in the practice if the overall practice is run fairly; for example: · Employees are paid well and treated well · Clients are treated well · the value and quality of the services are apparent · Employee pay is tied to performance Owners need to set an example as well. Violating the practices discount policy themselves or talking about the hard times the practice is going through after showing off a brand new expensive car will not gain respect and compliance from employees. As discussed above missed charges are generally a function of a system breakdown rather than an intent to give away a service. They generally occur because of: · Staff shortages-either real shortages or poor scheduling · Lack of systems · Bad systems · Incompetent or non-caring employees Many different kinds of invoicing systems will work well in capturing all fees but each step in the system must have one person specifically accountable for accuracy. Most systems have both manual and electronic steps and everyone, including doctors, must follow the agreed upon rules for medical record documentation and client invoicing. There needs to be a designated person to do a final review and sign-off on each invoice before a client leaves. Some practices designate an employee to review all records within 24-48 hours of the visit and compare actual services performed to those invoiced. Generally, the salary paid to these individuals is more than made up for by the missed charges they identify. When appropriate, clients should be called and told about the mistake and any holes in the system that allowed the missed charge to occur should be reviewed and fixed. Many practices have some systems, policies and rules in place to deter this from happening; however, few have done all they need to do. The goal is to see the right thing occur for "every client, every patient, every record, every time. Secondly (and most importantly), changes need to be made in the practice to improve inventory efficiency and costs. Inventory control is sometimes seen as a boring and tedious task, but it can have a huge impact on your profitability and is actually one of the easier things to do well in a practice. Before discussing why inventory costs might be high, it is important to understand the goals of an effective inventory system. This should be calculated for pharmacy items, food and all inventory combined Most practices use a cash basis of accounting for internal purposes. This means that when the bill is paid, the expense gets recorded in the financial statements. When using a cash basis of accounting, fluctuations in when bills are paid (whether deliberate or accidental) can have a significant impact on analysis. The practice should consider using some of the accrual accounting features available in most accounting software or doing the five or six journal entries necessary to convert cash to accrual every quarter or every year. It is 423 important that the people doing the bookkeeping and the financial analysis have enough real accounting knowledge to understand the implications of cash vs. There must be a balance between the time it takes to price-shop every product and the cost savings. There is also an advantage to working regularly with just 1-2 vendors as long as, on average, their costs are competitive or the practice is getting some other added value that is worth paying more for. The owners and managers in practices should try to carry as few choices as possible in each product category. It may be necessary to have one or more doctor meetings to talk through these choices and reach a consensus that is a balance between carrying a minimal number of products and insuring the practice has the drugs and supplies necessary to provide optimal care. It is often better to write a prescription for products which are rarely used rather than stock them. The vast majority of practices can get almost all products within just a few days of ordering; therefore there is no reason to keep vast quantities on the shelves (unless a genuinely good deal was available. Keeping too much on the shelves as well as product theft and accidental dispensing of product without charging the client are the most common reasons for high costs.
Tetracosanol (Policosanol). Nitroglycerin.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96177
Upper eyelid: the lateral compartment consists of the lacrimal gland; the central compartment is separated by the medial compartment and the superior oblique muscle medicine you can overdose on purchase 2.5 mg nitroglycerin overnight delivery. N Evaluation G G G G G G the ophthalmologic examination should include visual acuity symptoms quivering lips order nitroglycerin 2.5mg with amex, ocular motility symptoms norovirus purchase 6.5 mg nitroglycerin with amex, and ocular tension by palpation symptoms xanax buy nitroglycerin 6.5 mg without a prescription. Lid distraction test: A "snap test" test for lower lid laxity is performed by outwardly displacing the lower lid and observing for a normal snap (lid settling quickly back in place with less than 10-mm displacement) medicine 8 - love shadow generic nitroglycerin 6.5mg with visa. Lid retraction test: this also tests the laxity of the lower eyelid via inferior displacement; if the puncta moves 3 mm symptoms 6 week pregnancy discount nitroglycerin 2.5mg visa, it indicates a lax canthal tendon and the possible need for a tendon plication to avoid ectropion or scleral show. The brow should be at the orbital rim in males or just above the orbital rim in females and if ptosis is present, a brow repositioning procedure may be needed as well. N Contraindications Contraindications for a cosmetic blepharoplasty include severe heart or lung disease and psychological factors. Blepharoplasty is cautioned in patients with any of the following: G G Bleeding disorder or recent use of anticoagulants Previous facial palsy as it may lead to persistent weakness of the periorbital musculature with inadequate corneal lubrication and recurrent periorbital edema 7. Facial Plastic and Reconstructive Surgery G 663 G Chronic renal disease and diabetes as they may lead to wound-healing problems Thyroid disease including dry eyes syndrome and myxedema; eyelid manifestations may be eliminated by treating hypothyroidism Dry eyes may be worsened by blepharoplasty. G G N Surgical Goals Upper Eyelid Blepharoplasty Goals include addressing fat herniation, skin redundancy, and muscle hypertrophy. Note the asymmetry of the upper eyelids and the position of the superior orbital sulcus: the "tarsal crease" should be 10 mm from lid margin and below the bony margin of the orbital rim. The medial point of incision is 4 mm medial and 4 mm cephalad to the medial canthal tendon taking care to avoid the concavity of the medial orbital rim as this leads to webbing. The lower incision is marked along the tarsal crease 9 to 10 mm from the lid margin. An elliptical-shaped skin specimen is incised followed by blunt dissection with scissors and elevation off the orbicularis muscle. Lower Eyelid Blepharoplasty Goals include a sharp, well-defined canthus, maintenance of a good lower-eyelid position with an absence of scleral show. Surgical incisions are designed to avoid scar contracture in the vertical dimension, lower eyelid retraction, and ectropion. Two possible surgical approaches with either subciliary or transconjunctival approaches are described. Subciliary Approach the transcutaneous subciliary approach employs an external incision just below the eyelashes (high, immediately subciliary, or relatively lower to preserve the pretarsal orbicularis muscle). A skinmuscle flap technique is the preferred method when resection of the orbicularis muscle and skin is indicated the incision is through the skin followed by elevation, and possible fat removal. Fat removal requires the discrete separation of muscle fibers over each fat compartment and incising through the orbital septum. Closure involves lateral and superior elevation with resuspension of the orbicularis muscle. Fat may be removed from the lateral compartment first, followed by the central and then medial compartments. Fat may be infiltrated with 664 Handbook of OtolaryngologyHead and Neck Surgery additional nonepinephrine containing local anesthetic prior to cautery and removal. Advantages of the subciliary approach include a relatively avascular plane with a minimal risk of skin penetration, and additional tightening via skin muscle suspension using sutures from the lateral orbicularis muscle to the lateral orbital region. Limitations of the subciliary approach include a possible increased risk of ectropion. The surgeon may use surgical tape to counter the gravitational effect of postoperative edema, external scar, hematoma, or bruising as a result of orbicularis muscle dissection. Transconjunctival Approach Lower eyelid blepharoplasty is centered on the removal of redundant pseudoherniated fat with incision on the inner aspect of the eyelid. The ideal candidate is 20 to 30 years of age with significant pseudoherniation of fat, minimal skin excess, and minimal orbicularis hypertrophy. This approach is especially helpful to use in patients with tight, inelastic lower eyelids exhibiting scleral show, as this approach transects and releases inferior retractor muscles. The incision is in the lower eyelid conjunctiva with avoidance of disruption of orbicularis muscle. The preseptal approach involves placing the incision high along the inner eyelid conjunctiva with dissection anterior to orbital septum and under the orbicularis muscle. It is important to protect the cornea while dissecting behind the orbicularis muscle. Exposure of the surgical site and globe protection is facilitated with the use of nonconducting retractors. The dissection is continued downward and forward until all the pseudoherniated fat is exposed. Fat is removed to a depth 1 mm below the surface of the orbital rim with gentle pressure placed on the globe to assess for irregularity and asymmetry. Skin may be resected as necessary using the "pinch" technique or may be combined with chemical peel or laser resurfacing to address superficial fine-line rhytides. Transection of lower lid retractors may have the lower lid margin appear elevated for a few weeks. Advantages of the transconjunctival approach include avoidance of external scar, and potentially less risk of ectropion. Limitations include lack of addressing skin excess or hypertrophy of the orbicularis muscle. Lower eyelid blepharoplasty is associated with a higher rate of hematoma formation. It may occur up to a few days postoperatively and is treated with a lateral canthotomy and orbital decompression. Blindness Chronic G G G G G G G Ectropion Lagophthalmos Scleral show Ptosis Epiphora Inadequate excision of skin and fat Dry eyes Further Reading Bosniak S. The lateral skin is tightly adherent to the cartilage, whereas the medial or postauricular skin has loose connective tissue subcutaneously and thus can be easily separated and peeled from the underlying concha and scapha. The lobule has no cartilage and can have several anatomic configurations and positions. The abnormal development that results in deformities of the auricle usually originates from the second branchial arch. These abnormalities usually manifest themselves before the end of the first trimester of pregnancy; the frequency of variants is from 3 to 5% of the Western population. Also, aging makes the auricle appear larger, in part due to elongation of the lobule. N Evaluation of Aesthetic Deformities of the Auricle the helix, scapha/antihelix, posterior conchal wall, and conchal floor make up the four planes of the auricle. The angles between these planes and the auricle or scalp determine the degree of protrusion of the ear. The degree of protrusion or malformation is described as a variant from the normal conchascapha angle. Normal ears have a conchascapha angle of 75105 degrees, with 90 degrees most common. An ear is classified as "protruding" when the conchascapha angle 110 degrees, the angle of the ear to scalp 40 degrees, or the helical rim protrudes 3 cm. N Surgical Techniques Treatment of abnormally shaped ears commonly addresses two concerns: the lack of development of the antihelical fold and the deep concha cavum, respectively. The Mustarde-type approach utilizes permanent sutures to recreate the antihelical fold. The second approach utilizes scoring incisions, abrading, or filing the cartilage to alter its shape thus reestablishing a fold. A combination of the techniques may be utilized particularly if the scapha is resistant to reshaping via the suture placement. One is the Furnas-type approach of suturing posterior conchal cartilage to the mastoid periosteum. The other techniques involve excisions of conchal cartilage usually performed through the postauricular incision. The excisions can be elliptical or crescent-shaped with reapproximation of the cartilage or they can be disk shaped when combined with the conchal setback techniques. The goal is to reduce the height of the posterior conchal wall, thus reducing the prominence of the ear. Facial Plastic and Reconstructive Surgery 667 In the majority of patients, the permanent suture technique is utilized with or without scapha weakening. Deep conchal bowls are reduced by elliptical posterior cartilage excisions of 3 to 5 mm and usually followed by a conchal setback procedure. The procedure is done under general anesthesia in children and local anesthesia with sedation in adults. The incision is placed above the postauricular sulcus in an intermediate location between the mastoid and postauricular skin and the edge of the auricle. When reducing the conchal bowl, perform this first by excision of 3 to 5 mm and reapproximating the edges with 5-0 clear Prolene. The edges are undermined to avoid bunching of the skin, but not so extensively as to create conditions for hematoma formation. The creation of the antihelical fold is done by folding the auricle and noting the location for suture placement necessary to create the fold. The locations are then marked externally and internally prior to suture placement. The sutures are placed (usually two or three) in horizontal mattress fashion and are tied after all are placed. The knots are triply placed so that the suture can be "cinched" into its ideal position. After completing the conchal bowl and antihelical fold portions of the procedure, excess skin may be trimmed and additional maneuvers to reposition the lobule by postauricular skin excision are completed if deemed necessary. A cotton ball impregnated with mineral oil or topical ointment is then sutured fixated to the conchal bowl by placing 30 nylon on a long Keith needle to secure the bolster. The patient is discharged with a pain medication and a broad spectrum prophylactic antibiotic. N Complications Complications of otoplasty are rare, but include the possibility of hematoma formation, incision dehiscence, and a permanent suture dehiscence that would require a secondary procedure to replace the suture. If this should develop after 6 months, the suture can be removed without a significant change to the auricular contour; thus it is usually not necessary to replace an extruded suture at this point of the recovery. Wound infection is uncommon, but should be treated aggressively to avoid the long-term complication associated with chondritis. Although not commonly recognized as a complication, under- or overcorrection of the auricular deformity may occur. This should be managed individually to promote patient and family satisfaction with the surgical outcome with consideration of the risk-benefit ratio of further intervention. N Outcome and Follow-Up After discharging the patient, a postoperative visit is scheduled 48 hours after the procedure to evaluate the surgical site specifically for a conchal bowl hematoma. The appropriate use of the cotton bolster combined with conservative elevation of the overlying skin of the conchal bowl should make this complication rare. It is common at this point to see significant swelling as well as some bruising of the auricle. Open or closed approaches can be utilized, depending on the exposure required and preference. Rhinoplasty is surgery to reshape the nose, the most prominent and central facial feature. Common requests include making a nose smaller, reducing the bridge of the nose, narrowing the nose, making changes to the nasal tip, lifting a droopy nose, revising a previous rhinoplasty, and others. In addition to cosmetic concerns, deformities may contribute to problems with nasal function, such as an obstruction from valve collapse, requiring repair. The great majority of patients benefit emotionally and psychologically from rhinoplasty. Facial Plastic and Reconstructive Surgery 669 N Anatomy Although the anatomy of the nose has been fundamentally understood for many years, only relatively recently has there been an increased understanding of the long-term effects of surgical changes upon the function and appearance of the nose. A detailed understanding of nasal anatomy is critical for successful rhinoplasty. The accurate assessment of the anatomic variations presented by a patient allows the surgeon to develop a rational and realistic surgical plan. Furthermore, recognizing variant or aberrant anatomy is critical to preventing functional compromise or untoward aesthetic results. It is critical to consider the soft tissue and skin of the nose, which is thickest usually at the nasal tip, thinnest at the rhinion, and thick also at the nasion. The main underlying structures are the paired nasal bones, the upper lateral cartilages, the lower lateral (alar) cartilages, which include a medial crus and a lateral crus, and the nasal septum. Nasal Analysis It is critically important that the rhinoplasty surgeon develop skills of facial and nasal analysis. Our perception of beauty helps define what makes an ideal shape for a female or male nose, so there is also always a bit of an artistic element to this concept. Although the "aesthetic ideal" cannot be completely boiled down to simple lines and numbers alone, guidelines. Examples include the nasolabial angle (ideally 90105 degrees) and the nasofrontal angle (ideally 115120 degrees), and others. Preoperative photographic documentation is important, in frontal, right and left oblique, right and left lateral and basal views. Again, good communication regarding surgical goals is key, bearing in mind these contraindications to rhinoplasty: G G G G Continued intranasal cocaine use Psychiatric or mental instability Unrealistic patient expectations History of too many previous rhinoplasties N Incisions and Approaches Incisions are methods of gaining access to the bony and cartilaginous structures of the nose, and include transcartilaginous, intercartilaginous, marginal, and transcolumellar incisions. Approaches provide surgical exposure of the nasal structures including the nasal tip and include cartilage-splitting (transcartilaginous incision), retrograde (intercartilaginous incision with retrograde dissection), delivery approach (intercartilaginous marginal incisions), and external (transcolumellar and marginal incisions). An operative algorithm may provide a helpful starting point in selecting the incisions, approaches, and techniques used in nasal surgery. As the anatomic deformity becomes more abnormal, a graduated, stepwise approach is taken. However, other factors, such as the need for spreader grafts, complex nasal deviation, surgeon preference, and other factors may also appropriately affect the ultimate selection of approach. The endonasal approaches may be generally preferred for patients requiring conservative profile reduction, conservative tip modification, selected revision rhinoplasty patients, and other situations in which conservative changes are being undertaken.
Clonidine is now being used in dogs for certain behavioral conditions including phobias and separation anxiety medicine reviews cheap nitroglycerin 6.5mg with amex. Overdose of guanfacine and clonidine can result in clinical signs including depression symptoms right after conception order 2.5mg nitroglycerin with amex, sedation medicinebg order nitroglycerin 2.5 mg on-line, ataxia treatment 5th metatarsal stress fracture purchase nitroglycerin 2.5mg online, vomiting 3 medications that affect urinary elimination order nitroglycerin 6.5 mg amex, bradycardia medications that raise blood sugar cheap 2.5 mg nitroglycerin otc, hypotension, and potentially seizures and tremors. Signs can develop at low doses, and these drugs have a narrow margin of safety in pets. Asymptomatic patients may be induced to vomit and then given one dose of activated charcoal. Atipamezole will need to be re-dosed frequently as it typically lasts only 2-3 hours, while the effects of clonidine and guanfacine can have a duration of 24 hours or longer. Vital signs, especially heart rate and blood pressure, should be monitored frequently. At low doses, signs of anorexia, sedation or agitation have been reported with potential for hypertension, tachycardia, and possibly tremors at higher doses. Cats and pets with liver disease are thought to be more sensitive to the effects of this drug. With recent ingestion, induce emesis and then give one dose of activated charcoal. Treatment is symptomatic and supportive if signs develop with anti-emetics for nausea/vomiting, sedation for agitation, beta blockers if persistent tachycardia develops, and methocarbamol for tremors. These drugs may come as either an immediate release or extended release formulation. Larger overdoses may cause tremors, seizures, nystagmus, dysphoria, vocalization, aggressive behavior, ataxia, and, bradycardia. As the degree of overdose increases, so does the risk for the development of serotonin syndrome, a toxidrome characterized by central nervous, autonomic, and neurobehavioral signs including agitation, vocalization, vomiting, diarrhea, muscle rigidity, increased reflexes, tremors, hyperthermia, hypertension, and transient blindness. Appropriate decontamination with early emesis and activated charcoal is recommended if aspiration risk is low. Cyproheptadine, a serotonin antagonist, is useful in reducing the severity of signs, especially vocalization and dysphoria and is dosed at 1. Tricyclic antidepressants Tricyclic antidepressants are another class of antidepressants used in human medicine as well as veterinary medicine for separation anxiety, other behavior conditions, excessive grooming or feather plucking, urinary conditions, pruritus, and neuropathic pain. Common tricyclic antidepressants include amitriptyline, clomipramine (Clomicalm), nortriptyline, and doxepin. These drugs have a narrow margin of safety, and anticholinergic effects can develop with overdose. Signs of toxicity may include constipation, urine retention, mydriasis, sedation vs agitation, disorientation, ataxia, arrhythmias, tachycardia, hypertension, vomiting, serotonin signs, and seizures. Close monitoring of vital signs, especially cardiovascular monitoring, is warranted Many tricyclic antidepressants are fat soluble, so treatment with intravenous lipids may be helpful in cases of severe toxicity. Benzodiazepines and non-benzodiazepine sleep aids Benzodiazepines are commonly used as anxiolytics, anticonvulsants, muscle relaxants and sedatives/hypnotics. Common benzodiazepines used in veterinary medicine include alprazolam (Xanax), diazepam (Valium), lorazepam (Ativan), midazolam (Versed), and zolazepam found in combination with tiletamine as the dissociative agent (Telazol). Other benzodiazepines used in human medicine include clonazepam (Klonopin), oxazepam (Serax), and temazepam (Restoril). Common Non-benzodiazepine hypnotics include zolpidem (Ambien), eszopiclone (Lunesta), and zaleplon (Sonata). Chronic oral use of diazepam in cats, however, can result in hepatic failure and should be avoided. If necessary, the reversal agent or antidote, flumazenil, can be used but is rarely needed as these drugs are typically well tolerated. In symptomatic animals, monitor the body temperature and blood pressure and provide thermoregulation. In cases of paradoxical stimulatory signs, additional benzodiazepines should not be administered as they will exacerbate the clinical signs. Lithium Lithium carbonate and lithium citrate are used to treat bipolar disorder and as an adjunct to other antidepressants in humans, and its mechanism of action is not well understood. It has recently been tried as a treatment of anemia and neutropenia in dogs with bone marrow suppression, though with questionable efficacy. Lithium is a cation that competes with sodium, potassium, calcium, and magnesium at cellular sites, so animals with renal disease, dehydration, and sodium depletion can be more sensitive to this drug. Acute overdoses of this drug are typically well tolerated with only mild vomiting, anorexia, and lethargy expected. Chronic overdose, which occurs rarely in pets, can be more serious, and signs may include lethargy, muscle rigidity, tremors, seizures, hypotension, arrhythmias, and bradycardia. Treatment is otherwise symptomatic and supportive with antiemetics for vomiting, anticonvulsants for seizures, and methocarbamol for tremors and muscle rigidity. Lamotrigine Lamotrigine (Lamictal) is a phenyltriazine anticonvulsant that is also used to treat bipolar disorder in humans. Overdose of this drug can result in vomiting, lethargy vs hyperactivity, ataxia, weakness, tremors, seizures, hypokalemia, and acidosis. This drug is rapidly absorbed with onset of action in most cases within 4 hours, and signs can last 24-48 hours. Treatment of acute ingestions consists of appropriate decontamination and supportive care. Intravenous fluid may aid elimination and is also used for hydration and perfusion. Antiemetics are used as needed for vomiting, and diazepam and/or phenobarbital if seizure activity develops. Very depressed or comatose patients may need monitoring of respirations and blood gas, and some dogs require ventilatory support. Antipsychotics Antipsychotic drugs are used in human medicine to treat bipolar disorder, schizophrenia, and other psychiatric and neurologic conditions in humans. Common drugs in this class include olanzapine (Zyprexa), risperidone (Risperdal), aripiprazole (Abilify), and ziprasidone (Geodon). Signs of toxicity with these drugs include agitation or lethargy, hyperesthesia, vomiting, diarrhea, hypotension, tachycardia, ataxia, vocalization and aggression, serotonin syndrome, and arrhythmias. Animal studies of risperidone have shown that induction of emesis with apomorphine can be inhibited by this drug and may not be productive. It is also important to note that the "discmelt" version of Abilify contains xylitol. These drugs are quickly absorbed with rapid onset of signs, and signs typically last approximately 24 hours in dogs. Treatment of acute ingestions consists of appropriate decontamination with emesis only in asymptomatic patients and activated charcoal only if low risk of aspiration. Treatment is supportive with close monitoring of vital signs and blood pressure in symptomatic pets. Sedation is warranted in agitated pets, and if serotonin syndrome develops, cyproheptadine 1. Tremors can be treated with methocarbamol and seizures with standard anticonvulsants. Fulminant hepatic failure associated with oral administration of diazepam in 11 cats. Management of attention-deficit disorder and attention-deficit disorder drug intoxication in dogs and cats. Retrospective evaluation of toxicosis from selective serotonin reuptake inhibitor antidepressants: 313 dogs (2005-2010). Consider the proper patient assessment as described above to determine if the benefits of decontamination outweigh the risk and whether the exposure will harm the patient. If decontamination is deemed to be warranted, selecting the appropriate method will help ensure successful management of the patient. Types of decontamination include: Ocular If an animal has been exposed to a chemical that is considered an irritant or corrosive to the eye, ocular decontamination is warranted. The pH will indicate if it is acidic or alkaline and there are often key words on the bottle such as caution or danger. As ocular decontamination should be started as soon as possible, owners should be encouraged to flush the eye at home with tap water or saline. If the product is an irritant the eyes should be irrigated for 10-15 minutes at home and monitored for signs of irritation including redness, lacrimation, pawing or rubbing at the eye, squinting or edema. Corrosive products should also have an additional 15-20 minutes of irrigation performed by a veterinarian followed by a fluorescein stain, topical antibiotic ointment or drops and use of an Elizabethan collar. Dermal Dermal decontamination is indicated for exposure to corrosives or irritants, glues or adhesives, gasoline/hydrocarbons and systemically absorbed toxins. This will help prevent oral exposure by self-grooming, remove unwanted substances, minimize paresthesia and reduce the risk of burns. Irritant products generally have a caution statement on the label and result in mild redness and irritation. Rinsing product off or bathing with a degreasing dish soap is generally effective treatment. Corrosive products are alkaline or acidic in nature and generally have a danger statement on the label. Rinsing product for 15 minutes and bathing with a degreasing dish soap 2-3 times will help to remove product. The affected fur can be clipped if the animal is bothered to help avoid self-mutilation. Otherwise, if the affected area is not problematic, no therapy is generally necessary, and the product should wear off with time. They may cause defatting of the skin resulting in cracking, secondary infections and chemical irritant contact dermatitis. Systemically absorbed toxins do not generally cause dermal damage, however, result in systemic signs. Bathing 2-3 times in a degreasing dish soap will help to minimize absorption depending on the timing since exposure. Inhalation Toxins that may require respiratory decontamination include concentrates or corrosives, including bleach and ammonia mixtures, as well as smoke inhalation and carbon monoxide. A simple yet important aspect of inhalation decontamination is to remove the animal from the source of exposure. Oxygen therapy is often required for smoke inhalation, carbon monoxide, and cyanide toxicity. Birds are very sensitive to inhalants, and fragrances, Teflon, and regular respiratory irritants may cause significant concern. The animal should be removed from the source, be given humidified oxygen, and offered heat support and fluids. Gastrointestinal Emesis Emesis is by far the most common method of gastrointestinal decontamination. Approximately 49% (range of 9-75%) of stomach contents are recovered less than 30 minutes after ingestion. These ranges often make emesis success or failure difficult to assess, particularly when the ingestion is suspected but not known or when the number of items 346 ingested is unknown as is often the case when an animal chews up a bottle of medication or eats a handful of raisins. If emesis is unproductive, it does not guarantee that the ingestion did not happen as emesis does not fully empty the stomach of its contents. In many cases, there is a window of opportunity of only 1-2 hours for a positive return on emesis. However, there are certain toxins that can have successful emesis for up to 6 hours post ingestion. These include grapes, raisins, chocolate, xylitol containing gum, bezoars, massive ingestions and drugs that decrease gastric emptying (opioids, salicylates, anticholinergics and tricyclic antidepressants). Inducing emesis in dogs is performed by using apomorphine or 3% hydrogen peroxide. Hydrogen peroxide is a gastric irritant and exceeding recommended amounts may result in gastritis with gastric bleeding. Inducing emesis in cats is best performed by using an a-2 adrenergic receptor agonist drug such as xylazine at 0. Cats are more sensitive to developing hemorrhagic gastritis with hydrogen peroxide and is often not effective, therefore, not recommended. Salt toxicity, gastric irritation, nerve damage or aspiration may occur when other methods are used. Emesis should not be induced in symptomatic animals, those that have already vomited to bile/clear, or those with a history of aspiration pneumonia or at risk for such due to laryngeal paralysis or megaesophagus. Caution should be taken if inducing emesis in brachycephalic breeds, young animals (less than 3 months of age), geriatric pets (greater than 10-12 years of age), animals with a history of heart disease, seizures, recent surgery or those that have a non-toxic ingestion. Species that do not vomit include rabbits, ruminants (sheep, cattle, llama, goat), horses, birds and several rodents including chinchillas, rats and gerbils. Gastric lavage Gastric lavage may or may not be more effective at removing gastric contents. Often the more forceful contractions of the gastric muscles during emesis are more effective at removing contents than passive flow from lavage. This is a viable option for those species that do not vomit, symptomatic patients with a large ingestion, a large amount of stomach contents or where emesis was unsuccessful. It also may be helpful with potentially fatal ingestions including calcium channel blockers, beta blockers, baclofen, and metaldehyde. Safe performance of gastric lavage requires sedation, intubation, and endotracheal insufflation. The animal should be in right lateral recumbency with the head tilted down at an approximately 20-degree angle. The stomach tube should be measured to the last rib, passed in to the stomach, and flushed with 5-10ml/kg warm water. The stomach should be agitated and then aspirated or allow for gravity to drain stomach contents. Once adequate removal of stomach contents is achieved, activated charcoal can be given. Caution should be used, however, as it is not uncommon for regurgitation to occur and the risk of aspiration is high.
Physical exam may also suggest diagnosis: pleural friction rub raises possibility of pulmonary embolism or some other pleural-based lesion (lung abscess medicine nelly generic nitroglycerin 2.5mg on-line, coccidioidomycosis cavity treatment 9mm kidney stones cheap 2.5 mg nitroglycerin mastercard, vasculitis); diastolic rumbling murmur suggests mitral stenosis; localized wheeze suggests bronchogenic carcinoma medicine 750 dollars discount 6.5 mg nitroglycerin visa. Rigid bronchoscopy helpful when bleeding is massive or from proximal airway lesion and when endotracheal intubation is contemplated medications you can take while breastfeeding order 6.5 mg nitroglycerin overnight delivery. In massive hemoptysis medications like lyrica safe nitroglycerin 2.5mg, highest priority is to maintain gas exchange medications such as seasonale are designed to purchase nitroglycerin 6.5 mg otc, and this may require intubation with doublelumen endotracheal tubes. Pts with severely compromised pulmonary function may be candidates for bronchial artery catherization and embolization. Peripheral Cyanosis Occurs with normal arterial O2 saturation with increased extraction of O2 from capillary blood caused by decreased localized blood flow. Peripheral cyanosis most intense in nailbeds and may resolve with gentle warming of extremities. Clubbing may be hereditary, idiopathic, or acquired and is associated with a variety of disorders. Repeat while pt inhales 100% O2; if saturation fails to increase to 95%, intravascular shunting of blood bypassing the lungs is likely. Edema fluid is a plasma transudate that accumulates when movement of fluid from vascular to interstitial space is favored. Since detectable generalized edema in the adult reflects a gain of 3 L, renal retention of salt and water is necessary for edema to occur. Allergic reactions ("angioedema") and superior vena caval obstruction are causes of localized facial edema. Ascites (fluid in peritoneal cavity) and hydrothorax (in pleural space) may also present as isolated localized edema, due to inflammation or neoplasm. Bilateral lower extremity swelling, more pronounced after standing for several hours, and pulmonary edema are usually cardiac in origin. Periorbital edema noted on awakening often results from renal disease and impaired Na excretion. In cirrhosis, arteriovenous shunts lower effective renal perfusion, resulting in Na retention. Ascites accumulates when increased intrahepatic vascular resistance produces portal hypertension. Reduced serum albumin and increased abdominal pressure also promote lower extremity edema. In nephrotic syndrome, massive renal loss of albumin lowers plasma oncotic pressure, promoting fluid transudation into interstitium; lowering of effective blood volume stimulates renal Na retention. Supportive stockings and elevation of edematous lower extremities will help mobilize interstitial fluid. If severe hyponatremia (132 mmol/L) is present, water intake should also be reduced (1500 mL/d). Distal ("potassium sparing") diuretics or metolazone may be added to loop diuretics for enhanced effect. Note that intestinal edema may impair absorption of oral diuretics and reduce effectiveness. Overdiuresis may result in hyponatremia, hypokalemia, and alkalosis, which may worsen hepatic encephalopathy (Chap. Regurgitation refers to the gentle expulsion of gastric contents in the absence of nausea and abdominal diaphragmatic muscular contraction. Rumination refers to the regurgitation, rechewing, and reswallowing of food from the stomach. Increased intrathoracic pressure results in further movement of the material to the mouth. Vomiting is controlled by two brainstem areas, the vomiting center and chemoreceptor trigger zone. Activation of the chemoreceptor trigger zone results in impulses to the vomiting center, which controls the physical act of vomiting. For example, vomiting that occurs predominantly in the morning is often seen in pregnancy, uremia, and alcoholic gastritis; feculent emesis implies distal intestinal obstruction or gastrocolic fistula; projectile vomiting suggests increased intracranial pressure; vomiting during or shortly after a meal may be due to psychogenic causes or peptic ulcer disease. The effectiveness of antiemetic medications depends on etiology of symptoms, pt responsiveness, and side effects. Antihistamines such as dimenhydrinate and promethazine hydrochloride are effective for nausea due to inner ear dysfunction. Anticholinergics such as scopolamine are effective for nausea associated with motion sickness. Haloperidol and phenothiazine derivatives such as prochlorperazine are often effective in controlling mild nausea and vomiting, but sedation, hypotension, and parkinsonian symptoms are common side effects. Selective dopamine antagonists such as metoclopramide may be superior to the phenothiazines in treating severe nausea and vomiting and are particularly useful in treatment of gastroparesis. Intravenous metoclopramide may be effective as prophylaxis against nausea when given prior to chemotherapy. Ondansetron and palosetron, serotonin receptor blockers, and glucocorticoids are used for treating nausea and vomiting associated with cancer chemotherapy. Aprepitant, a neurokinin receptor blocker, is effective at controlling nausea from highly emetic drugs like cisplatin. Functional dyspepsia is defined as 3 months of dyspepsia without an organic cause. Functional dyspepsia is the cause of symptoms in 60% of pts with dyspeptic symptoms. In most cases, the esophagus is not damaged, but 5% of pts develop esophageal ulcers and some form strictures. Extraesophageal manifestations include asthma, laryngitis, chronic cough, aspiration pneumonitis, chronic bronchitis, sleep apnea, dental caries, halitosis, and hiccups. Clinical trials suggest that proton pump inhibitors (omeprazole) are more effective than histamine receptor blockers (ranitidine) in patients with or without esophageal erosions. Surgical techniques (Nissan fundoplication, Belsey procedure) can be used in the rare pts who are refractory to medical management. The routine medical history should always include inquiry about changes in weight. Rapid fluctuations of weight over days suggest loss or gain of fluid, whereas long-term changes usually involve loss of tissue mass. In older persons the most common causes of weight loss are depression, cancer, and benign gastrointestinal disease. In the absence of documentation, changes in belt notch size or the fit of clothing may help to determine loss of weight. The history should include questions about fever, pain, shortness of breath or cough, palpitations, and evidence of neurologic disease. Travel history, use of cigarettes, alcohol, and all medications should be reviewed, and pts should be questioned about previous illness or surgery as well as diseases in family members. Signs of depression, evidence of dementia, and social factors, including financial issues that might affect food intake, should be considered. Physical examination should begin with weight determination and documentation of vital signs. The skin should be examined for pallor, jaundice, turgor, surgical scars, and stigmata of systemic disease. Evaluation for oral thrush, dental disease, thyroid gland enlargement, and adenopathy and for respiratory, cardiac, or abdominal abnormalities should be performed. All men should have a rectal examination, including the prostate; all women should have a pelvic examination; and both should have testing of the stool for occult blood. Neurologic examination should include mental status assessment and screening for depression. Initial laboratory evaluation is shown in Table 49-2, with appropriate treatment based on the underlying cause of the weight loss. If an etiology of weight loss is not found, careful clinical follow-up, rather than persistent undirected testing, is reasonable. Globus pharyngeus is the sensation of a lump lodged in the throat, but swallowing is unaffected. The motor function abnormalities that cause dysphagia may be related to defects in initiating the swallowing reflex. Approach to the Patient History can provide a presumptive diagnosis in about 80% of pts. Difficulty with both solids and liquids may occur late in the course of mechanical dysphagia but is an early sign of motor dysphagia. Weight loss out of proportion to the degree of dysphagia may be a sign of underlying malignancy. Hoarseness may be related to involvement of the larynx in the primary disease process. Physical exam may reveal signs of skeletal muscle, neurologic, or oropharyngeal diseases. Dysphagia is nearly always a symptom of organic disease rather than a functional complaint. If oropharyngeal dysphagia is suspected, videofluoroscopy of swallowing may be diagnostic. Mechanical dysphagia can be evaluated by barium swallow and esophagogastroscopy with endoscopic biopsy. Barium swallow and esophageal motility studies can show the presence of motor dysphagia. Causes include: for solids only, carcinoma, aberrant vessel, congenital or acquired web (Plummer-Vinson syndrome in iron deficiency), cervical osteophyte; for solids and liquids, cricopharyngeal bar. Causes include: gastroesophageal reflux disease, esophageal motility disorders, peptic ulcer disease, gallstones, psychiatric disease (anxiety, panic attacks, depression). Evaluation Consider a trial of antireflux therapy (omeprazole); if no response, 24-h ambulatory luminal pH monitoring; if negative, esophageal manometry may show motor disorder. Barium swallow shows dilated esophagus with distal beaklike narrowing and air-fluid level. Causes include: primary (idiopathic) or secondary due to gastroesophageal reflux disease, emotional stress, diabetes, alcoholism, neuropathy, radiation therapy, ischemia, or collagen vascular disease. Condition may resolve over time or evolve into diffuse spasm; associated with increased frequency of depression, anxiety, and somatization. Evaluation Barium swallow shows corkscrew esophagus, pseudodiverticula, and diffuse spasm. Manometry shows spasm with multiple simultaneous esophageal contractions of high amplitude and long duration. If heart disease has been ruled out, edrophonium, ergonovine, or bethanecol can be used to provoke spasm. Rare pts require surgical intervention; longitudinal myotomy of esophageal circular muscle. Oral valganciclovir (900 mg bid) is an effective alternative to parenteral treatment. Diagnosis is made on endoscopy by identifying yellowwhite plaques or nodules on friable red mucosa. Predisposing factors include recumbency after swallowing pills with small sips of water, anatomic factors impinging on the esophagus and slowing transit. Consider obstruction, perforation, or rupture of hollow viscus; dissection or rupture of major blood vessels (esp. Brief History and Physical Examination Historic features of importance include age; time of onset of the pain; activity of the pt when the pain began; location and character of the pain; radiation to other sites; presence of nausea, vomiting, or anorexia; temporal changes; changes in bowel habits; and menstrual history. Abdominal paracentesis (or peritoneal lavage in cases of trauma) can detect evidence of bleeding or peritonitis. Abdominal ultrasound (when available) reveals evidence of abscess, cholecystitis, biliary or ureteral obstruction, or hematoma and is used to determine aortic diameter. Diagnostic Strategies the initial decision point is based on whether the pt is hemodynamically stable. If not, one must suspect a vascular catastrophe such as a leaking abdominal aortic aneurysm. Such pts receive limited resuscitation and move immediately to surgical exploration. If the pt is hemodynamically stable, the next decision point is whether the abdomen is rigid. If the abdomen is not rigid, the causes may be grouped based on whether the pain is poorly localized or well localized. In the presence of poorly localized pain, one should assess whether an aortic aneurysm is possible. Pain localized to the epigastrium may be of cardiac origin, esophageal inflammation or perforation, gastritis, peptic ulcer disease, biliary colic or cholecystitis, and pancreatitis. Pain localized to the right upper quadrant includes those same entities plus pyelonephritis or nephrolithiasis, hepatic abscess, subdiaphragmatic absess, pulmonary embolus, or pneumonia or be of musculoskeletal origin. Additional considerations with left upper quadrant localization are infarcted or ruptured spleen, splenomegaly, and gastric or peptic ulcer. Left lower quadrant pain may be due to diverticulitis, perforated neoplasm, and other entities previously mentioned. Traditionally, narcotic analgesics were withheld pending establishment of diagnosis and therapeutic plan, since masking of diagnostic signs may delay needed intervention. Intestinal water absorption passively follows active transport of Na, Cl, glucose, and bile salts. Proximal small intestine: iron, calcium, folate, fats (after hydrolysis of triglycerides to fatty acids by pancreatic lipase and colipase), proteins (after hydrolysis by pancreatic and intestinal peptidases), carbohydrates (after hydrolysis by amylases and disaccharidases); triglycerides absorbed as micelles after solubilization by bile salts; amino acids and dipeptides absorbed via specific carriers; sugars absorbed by active transport. Propulsion is controlled by neural, myogenic, and hormonal mechanisms; mediated by migrating motor complex, an organized wave of neuromuscular activity that originates in the distal stomach during fasting and migrates slowly down the small intestine. Defecation is effected by relaxation of internal anal sphincter in response to rectal distention, with voluntary control by contraction of external anal sphincter.
Generic 6.5 mg nitroglycerin amex. 9 Signs That PROVE You're A Psychic Medium.
References