




|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Brian G. Blackburn, MD
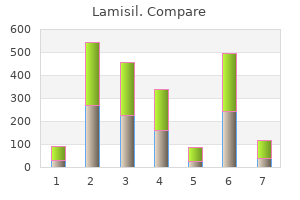
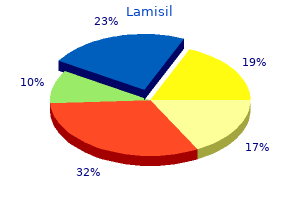
The goal of increasing coverage is an important fungus gnats in plants lamisil 250mg with visa, fundamental aspect of healthcare reform; however antifungal toenail cream order lamisil 250mg with visa, healthcare reform is much broader- and some would say pervasive-than insurance access fungus gnats natural pesticide generic lamisil 250mg with amex. To some degree antifungal thrush quality 250 mg lamisil, the media has focused most of its attention on the insurance aspect to the detriment of other important elements of reform antifungal absorbent powder buy cheap lamisil 250 mg line. This may be because of the complexity of other features or a sense that many of the other reform functions seem esoteric and too focused on addressing the perceived murkiness of the healthcare system fungi definition pronunciation buy lamisil 250 mg lowest price. Throughout this publication, the authors have made reference to healthcare reform, particularly in terms of how it relates to , influences, or even changes fundamental healthcare system functions. This includes healthcare workforce, improved quality of care, healthcare system efficiency (sometimes interpreted exclusively as cost control), and ultimately improved health status and population health. These are all significant issues; however, for the public and mass media, it may be easier to understand having or not having health insurance than it is to understand vague concepts like "value over volume. This will be discussed first with national overtones, and then as it relates to North Dakota. While the initial rollout of the Marketplace in 2014 did not happen without some serious snafus, by 2015 and 2016 most of the blips in the system seem to have been resolved. Nationally, the rate of uninsured has declined by 7 percentage points, from a high of 18% (Quarter 1, 2014) to a low of 11% (Quarter 1, 2016). During the initial rollout in 2014, there were 8 million people enrolled through the Marketplace. Some of the subgroups experiencing the largest reductions in uninsured rates include people earning $36,000 a year or less (30. With the advent of the Marketplace, the percentage of Americans who purchase insurance on their own or through a family member has increased, from 17. According to the Kaiser Foundation, there may be about 3 million to 4 million Americans in the gap. A study published in Health Affairs (2016) estimated that uncompensatedcare costs decreased from 4. There have been greater savings associated with hospitals that had a higher uncompensated-care base before the enactment of the law. Many of the states that have not expanded Medicaid are states that have a higher uncompensated-care level; thus, if they had participated in the program the benefit to those hospitals and states would likely be even higher than noted in the states that did implement Medicaid Expansion. Health Reform in North Dakota In North Dakota, as of March 2016 (most recent data), there were 20,536 North Dakotans who had gained access through the Marketplace for private insurance coverage. Using the middle number 70,000 as a base, with 40,000 newly insured, the percentage of uninsured has declined by about 57% since 2013. There is the lessening of bad debt and charity care, and increased Medicaid reimbursement both in terms of increased volume and increased payment rates. Over the next few years, the ratio moves in increments to a 90:10 level, where the states cover only 10% of the added costs. This compares with general Medicaid where the state may contribute up to 50% of the Medicaid costs. Thus, in North Dakota, hospitals receiving millions of dollars more in Medicaid reimbursement is positive. The reimbursement is at a level that can be used to treat a new patient base that because of limited access to healthcare services has, in many cases, years of untreated conditions. It does cost money to treat these patients to not only address chronic conditions or delayed primary care but to also hopefully improve their individual health status and to focus on prevention. Over time, these new patients-through prevention, care coordination, health coaching, and other methods-become examples of the concept of better care, better health, and lowered cost. Additionally, by reducing uncompensated-care costs, hospitals have the resources to address community needs as part of their community benefit effort. Many people enrolling through the Marketplace are eligible for a federal subsidy to help buy down the cost of their premiums. In North Dakota, about 86% of the Marketplace enrollees received the federal tax credit for 2016. The average subsidy per month was $262 (2016) with the average out-of-pocket cost after the subsidy being $142 per month. If it is determined that someone does not have insurance, they are subject to a penalty. Burwell, upheld the constitutionality or legality of the use of subsidies in every state, including those that use the federal as opposed to state marketplace (the state-versus-federal marketplace had been at the heart of the constitutional question). If the Court had ruled against this, making the tax credit not available in states that used the federal marketplace (like North Dakota), the average increase in premiums in North Dakota would have been 169% in one year because of the absence of a tax credit. With 86% of North Dakota Marketplace subscribers availing themselves of a tax credit, this would have effectively eliminated access to insurance for thousands of North Dakotans. It is important to understand that the subsidy is only available by enrolling through the Marketplace. The subsidy can go as high as 400% of the federal poverty level (for a family of four in 2014, this would mean up to an income of $94,200). There is at least one navigator in each of the eight planning or human service regions of the state (Williston, Minot, Devils Lake, Grand Forks, Fargo, Jamestown, Bismarck, and Dickinson). The Great Plains Tribal navigator program serves American Indians in both North and South Dakota. In North Dakota, there are four navigators associated with the Great Plains effort. One of these is "filling the doughnut hole" found in the expansion of Medicare to include prescription coverage (Medicare Part D. Because of annual adjustments, this doughnut hole was set for 2016 so that the customer is responsible for prescription costs above $3,310 until it reaches the cap of $4,850. Nationally, in 2014 alone (most recent year), 39 million people benefited from this service. The benefit covers cancer screenings, bone-mass measurements, annual physicals, and smoking cessation. For the non-Medicare public, there are also free preventive services covering immunizations, certain cancer screenings, contraception, reproductive counseling, obesity screening, and behavioral assessments for children. One study found that 36% of those who tried to purchase insurance directly were turned down, charged more, or had a specific health problem excluded from their coverage plan. In North Dakota, 276,000 residents had a preexisting condition that is now protected under federal law. A final benefit to note is that health reform requires health insurers to provide consumers with rebates if the amount they spend on health benefits and quality of care is low-as opposed to advertising and marketing. While thousands of North Dakotans and millions of Americans have experienced new opportunities for insurance coverage from the Marketplace or Medicaid Expansion, there are many people who have insurance either through their employer or have to purchase it on their own. They do not qualify for Marketplace subsidies or Medicaid Expansion, and have experienced some "sticker shock" on premium increases in the open market. Nationwide, premiums are expected to increase by 5% to 6% in 2017 for employer-supported plans. Additionally, the rates that insurance companies charge for plans sold through the Marketplace are tipping into double-digit increases. Some employer plans are kept in check by having higher deductibles and co-pays making a trade-off between premiums (costs to the employer and possibly the employee) and out-of-pocket costs for the employee. Some deductibles are as high as $6,500 for an individual plan and $13,000 for a family plan. The rationale for the premium increases has been ascribed to "sticker shock" for the insurance industry. Not everyone who has chronic diseases or other health issues is able to qualify for subsidies. There is a sizable group of Americans who are economically middle class who have health conditions, and they may be bearing the brunt of the changes, including the cost of care, in the system. What is being missed and not adequately explained to the average citizen is how health reform is significantly changing the American healthcare delivery system and how we as a nation-and even as individuals-approach and contemplate health. In a nutshell, under health reform, we are 1) attempting to increase access to healthcare by establishing financial security. Higher-cost services such as inpatient care, readmissions to the hospital, and excess use of the emergency department as a substitute for primary care are scrutinized so as to target appropriate care (better care). In a way, the dual concepts guiding health reform are insurance access and the allocation and management of financial risk (increasing insurance coverage and spreading more financial risk to the provider class). Thus, the Three Aims of better health, better care, and lower or controlled costs are addressed through this focus. This is a simplification of health reform; however, the essence of reform is embodied in that framework. The structural redesign of the American health delivery system brings into the framework of discussions essential elements that have been covered throughout this Biennial Report: financial conditions and constraints, health professional workforce demand and supply, organizational arrangements and systems, health quality metrics and analytics, quality of care and patient safety improvement, and health information technology, such as electronic medical records. Health reform is pervasive, systemic, and complex, encapsulating needs and wants that have meaning for the private and public sectors, and individual and collective levels, and involve the tangible and conceptual. The issue for rural citizens and providers is, do they fit in this new value-based system How can health facilities with limited utilization, workforce shortages, and financial constraints navigate this new delivery system One national rural health and health reform expert commented that "the greatest threat to the sustainability of rural healthcare systems are market forces that will force doctors and patients to choose high-value providers and partners-and rural will be left behind. Essentially, what we are attempting to do is gradually adjust our payment structure from one that relies on and reinforces paying for more services on a fee-for-service basis. So, what are some of the significant changes in pursuit of better care, better health, and lowered costs Burwell announced in January 2015 some ambitious goals to shift Medicare payments into a value-based framework. The secretary announced in March 2016 that the goals for that year were already met, well ahead of the end of the year. One is the Hospital Readmissions Reduction Program, where hospitals that have excess readmissions are penalized. Hospitals are given an incentive on a pay-for-performance method wherein a portion of reimbursement is influenced by how well the hospital performs on a set of measures compared with other hospitals or how much they improve their performance on each measure compared with their baseline performance period. All three of these initiatives are indicative of the drive to correlate quality with payment and to emphasize value or outcomes. In other words, payment follows the patient as one payment allocation is made to be shared by all the providers for an episode of care. This contrasts to the traditional approach, where each provider receives a separate payment directly from the payer. The theory is that a bundled payment may be more efficient and is awarded based on value or outcome as opposed to each provider receiving a payment for specific services. Some healthcare experts have cautioned that one of the unintended implications is that the bundled payment structure may change relationships with post-acute-care providers. Unless the patient specifically says they want to go back to their home provider, the post-acute care does not have to take place in the originating community. Experts feel this will lead to changes in some facility-to-facility relationships. The American Academy of Pediatrics pioneered the idea in 1967 to create a new medical approach that strove to include patients and families in the treatment process by emphasizing primary healthcare that was accessible, family-centered, coordinated, comprehensive, continuous, compassionate, and culturally effective. It emphasizes the role of primary care, and sometimes is called the primary care medical home model. In the early 2000s, family medicine also adopted the language of patient centeredness in a report titled, the Future of Family Medicine: A Collaborative Project of the Family Medicine Community, which called for everyone to have a personal medical home. Mental or behavioral health and other specialty services can be woven into the application of the model. It can also incorporate per-member, per-month medical home payments and allows for risk adjustment. The Geisinger Health Plan program (associated with the Geisinger Medical Center, a large rural-based system in Pennsylvania) was found to have reduced hospital admissions by 18% and readmissions by 36% per year. The Group Health Cooperative of Puget Sound was found to have reduced emergency department visits by 29%. The Milbank Memorial Fund and the Patient-Centered Primary Care Collaborative issued a report on the model in 2014. The study showed that there have been some improvements in cost, utilization, population health, prevention, and patient satisfaction, but there is still a gap in evidence with regard to physician satisfaction. A study published in the Journal of the American Medical Association was less promising. It can be physicians only, hospitals only, physicians and hospitals, or other health providers. The Shared Savings and the Pioneer models were announced in 2011, and while they each concentrate on improving care and quality for Medicare beneficiaries along with reducing healthcare costs, they do differ in their construction. The Pioneer Model accepts risk for at least 15,000 beneficiaries (with 5,000 in rural areas). The Next Generation model requires even more risk allocation to the providers, above what is found in the Pioneer Model (up to 100% of the risk). This also means that the Next Generation model provides for more opportunity to share in cost savings (bonuses for better care coordination and care management). The networks entering this model tend to be experienced, having been either part of a Pioneer or a Shared Savings model. Next Generation also employs prospective rather than retrospective benchmarks and will test beneficiary incentives.
In addition antifungal shampoo for dogs buy lamisil 250 mg cheap, through state funding fungi quiz biology generic lamisil 250mg fast delivery, there were "earmarked" funds for oil-impacted counties that covered additional costs associated with staff anti bacterial fungal shampoo for dogs lamisil 250mg without a prescription, equipment fungus gnats removal generic lamisil 250 mg fast delivery, coverage antifungal eye drops lamisil 250 mg for sale, and training fungus gnats wood discount lamisil 250 mg free shipping. The 2015 Legislature also approved what is called a Medicaid rebase in which the payments for ambulance transfers (from one hospital to another) were adjusted. This had been at 53% and was increased to 64% for a significant increase of 11 percentage points. There is an understanding that the state government does not wish to be the employer of community-based emergency services personnel. There is an increasing recognition that, in addition to improving actual provider skill levels, there is a corresponding need to improve the ability of rural units in the areas of management, leadership, and planning. The 2013 North Dakota Legislature supported this effort, and in 2014, a pilot program was released. Stakeholder meetings were convened, and the program solicited licensed North Dakota ambulance services to participate in the pilot. Four pilots were selected in Rugby, Fargo, Bowman, and Dickinson (covering Billings County and the communities of Belfield, Medora, and Beach). Dickinson Southwestern District Health Unit proceeded under an additional public health grant from a private funder called Million Hearts. More than 12 paramedics from these communities completed additional training in community paramedicine based on a national curriculum. Community paramedics are experienced field paramedics who undergo additional education to provide a wider scope of primary and non-emergent care. Community paramedicine does not require an additional license and community paramedics operate within the standard scope of practice for a paramedic. Medicaid did approve some reimbursement of community paramedics who provide immunizations. Community paramedics could, in time, be an important provider in frontier and rural areas, and the discipline could serve to build closer collaboration between emergency services and primary care, public health, home care, and long-term care. Related to these three areas, and addressed in more detail in Chapter 7, is the concentration of human health resources to better coordinate care and manage services not only for the betterment of the patient but also to create organizational and financial efficiencies. The community paramedic model may be a new provider class that can help to redesign elements of the delivery system, particularly in rural areas. Currently in North Dakota, there is only Medicaid reimbursement to community paramedics performing immunizations. Minnesota allows a much wider scope of services to be reimbursed under Medicaid (health assessments, medication compliance checks, chronic disease monitoring and education, hospital discharge follow-up, and immunizations and vaccinations). A larger health system employing community paramedics that are addressing more population health services offers the opportunity to spread out the costs, which a small or rural system cannot do. In other words, cost savings accrue to the system both in the form of lower cost interventions that replace more expensive services such as repeated visits to the emergency department or rehospitalization, and in the form of maximizing the utilization of a fixed-cost resource. Preliminary data from the community paramedicine efforts in Fargo indicate that, in a relatively small sample of 30 patients, emergency room visits were reduced by one-half and the no-show rate to primary care providers was cut by 30%. Another important area for North Dakota relates to stroke and cardiac systems of care. The highest level of designation is the Comprehensive Stroke Center; however, no North Dakota hospital is so designated. In a similar way, the state works to establish and maintain a comprehensive cardiac system. The department does this in a variety of ways including having developed a Cardiac Ready designation program and process for communities, which is similar to what was previously stated about stroke designations. These designations are for a community that is prepared to take on cardiac emergency events and to improve survival rates. In addition, the department has used the Million Hearts program with the American Heart Association in the community paramedic effort in Dickinson and Billings County to address hypertension referrals. A Cardiac Task Force has worked on a continuum of care with statewide cardiac protocols and recommendations for ambulances and hospitals. The complexity is a part of the ongoing need to construct viable stroke and cardiac systems of care. This also represents a level of integration with the trauma system (discussed in more detail in the following section) because that system also has transport plans. Corresponding with the transport plans are also the designation of hospitals at certain levels and standard practices. However, the focus on stroke and cardiac care is looking at new models that may better reflect the unique quality of these systems as opposed to simply replicating the trauma model. The lessons learned from the exercises assisted in identifying equipment and service gaps, and refining database processes. Continuing the idea of education for cardiac emergency readiness, the Center for Rural Health is in the process of developing an interactive learning module titled, "Continuous Quality Improvement: Time Critical Response Processes," which will be offered to the cardiac system of care stakeholders. Trauma ranks as the third-leading cause of death (fifth in the Third Biennial Report) and is the leading cause of death for people 46 years of age or younger, or 47% of all deaths in that age group. Trauma injury accounts for 30% of all life years lost in the United States; that compares with cancer, which accounts for 16% and heart disease at 12%. Trauma events, as recorded in the state trauma registry, have increased 49% from 2008 to 2014 to a total of 6,008. The numbers in 2014 are slightly below what was reported in the Third Biennial Report when there were 6,227 cases of reported trauma events. The southwest quadrant experienced an increase of 64%; northeast, 54%; and southeast, 33%. The area with the highest number of trauma events was found in the southeast, where there were 1,812. Likely because of the rapid expansion in oil and other energy development resources, the incidence of natural-resources-employment-related trauma increased by 49% from 2009 to 2014 (from 32 incidents in 2009 to 166 in 2014). Agriculture has experienced a decline in trauma rates from 104 to 85 occurrences (down 18% from 2009 to 2014). Verification of trauma centers has been based upon nationally recognized standards by the American College of Surgeons Committee on Trauma. The standards address hospital organization, clinical capabilities, facility and equipment availability, quality improvement processes, prevention and public education, trauma research, continuing education, trauma service support personnel, and transfer agreements. Level I is a comprehensive regional resource-tertiary care center-providing total care for every area of injury from prevention to rehabilitation. It offers 24-hour immediate coverage by general surgeons, including orthopedic surgery, neurosurgery, anesthesiology, emergency medicine, radiology, and critical care. This level can provide prompt assessment, resuscitation, surgery, intensive care, and stabilization of injured patients. This level provides evaluation, stabilization, and diagnostic capabilities for injured patients. A Level V trauma center provides initial evaluation, stabilization, and diagnostic capabilities and prepares patients for transfer to higher levels of care. Studies have found a number of factors that are advantages and assets to the North Dakota trauma system. The term "telemedicine" refers specifically to patient and healthcare provider encounters for diagnosis and treatment. The term "telehealth" is a broader term that includes telemedicine but also includes using technology for preventive, educational, and healthrelated administrative activities. Both telemedicine and telehealth involve interactive medical equipment, computer technology, and telecommunications technology. It can serve as a vehicle to move critical information quickly and efficiently, thus improving organizational performance. One of the steps supported was a provider-needs survey in 2008 administered by the Center for Rural Health. Survey results indicated that 70% would not have been able to purchase an electronic health record system without the loan funding. In addition to the previously mentioned resources available for providers, the Center for Rural Health and Quality Health Associates of North Dakota (formerly the North Dakota Healthcare Review, a quality improvement organization that is the state subcontractor to the multi-state regional quality improvement organization) partnered with Key Health Alliance, an association of Stratis Health; National Rural Health Resource Center; and the College of St. Ambulance Chriopractic Nonaffiliated Clinics X X X X X X X X X X X X electronically exchange health information. In fact, the report states that "in 2013, the percentage of physicians who had a system meeting the criteria for a basic system ranged from 21% in New Jersey to 83% in North Dakota. In a 2011 Surescripts report, North Dakota ranked 49th in e-prescribing activity; currently, North Dakota is ranked 15th. In 2012, pharmacies listed phone and fax as the top two ways they received new prescriptions and renewals. In December 2015, opioids made up 32% of all controlled substance e-prescriptions. Communicate is a simple, secure method for participants to send encrypted health information directly to known, trusted recipients. Some examples of information that providers and payers exchange include documents, images, Health Level 7 message strings, claims attachments, and continuity-of-care documents. The portal provides authorized users with a complete summary of care, including information such as allergies, medical history, diagnostic results. All of this information can be used by healthcare providers to make the right decisions for patients. To minimize the number of places providers need to go to obtain information, clinical portal users can also query the North Dakota Immunization Information System and the Prescription Drug Monitoring Program. Another feature includes subscription and notification services, which allows a provider that has a medical treatment relationship with another provider to "subscribe" to a patient and receive notifications when an event is triggered. Event triggers may include an inpatient admission or discharge, abnormal lab result, panic results, new final radiology result, and emergency room admittance. Future enhancements include adding medication information to the clinical portal, as well as partnering with other healthcare providers, such as long-term care and behavioral health providers. The repository will allow citizens to upload an advance directive and give permission for authorized users, such as their provider, to access it. The environmental scan was completed June 2016, and a business plan was completed October 2016. As discussed previously, telehealth is the more general term and means the electronic transfer of medical information for the purpose of patient care. Telemedicine is specifically the use of these technologies to deliver patient-care services. Through technologies such as videoconferencing and other online applications, telehealth allows care providers to reach more people. However, providers have continued to grow their utilization of videoconferencing beyond meetings and educational purposes. Through a twoway video technology, board-certified emergency physicians and emergency-trained nurses are made available to assist local providers in treating trauma, heart attack, stroke, and other critical conditions. Lastly, efforts are gaining ground to utilize telehealth to meet mental and behavioral care needs (discussed in more detail in the Mental Health section). This Workgroup provided comments about telehealth to the North Dakota Board of Medicine, as well as testimony during the 2014 legislative session relating to individual and group health insurance coverage of telehealth services. The report will be used to determine how to proceed with a law related to reimbursement for telehealth services for the general public. As was discussed in Chapter 1, North Dakota must contend with an aging population that has a corresponding effect on policy decisions (federal and state) as it relates to health infrastructure, health status, education, housing, transportation, economic development, and other sectors. In North Dakota, from an organizational framework, long-term care facilities include assisted living, basic care, and nursing care. In a previous chapter, the significant workforce issues found in longterm care were discussed. The top three factors affecting the need for nursing home care are 1) being female, 2) being 80 or older, and 3) living alone. The association also found that the most common reasons provided for nursing home placement include 1) the need for assistance with daily care throughout the day, 2) complex medical needs, and 3) the need for continuous supervision. There are 68 basic-care facilities in North Dakota (with 47 or 69% located in rural areas). North Dakota has 72 assisted living facilities (with 44 or 61% located in rural areas). More than 31,000 North Dakotans (65 years of age and older) live alone or 30% of that age cohort. North Dakota is projected to see an increase in the 65-years-of-age-or-older population by 44% from 2013 to 2025, to almost 150,000 people (148,060). A basic plan typically covers meals, housekeeping, activities, transportation, and laundry. The assisted-living facility typically provides health services from bathing to medication management to hospice. In North Dakota, the age range of current residents is from 51 to 104, with the average age being 85. The most common reasons people have for choosing assisted living include the following: 1) assistance with daily care, 2) social isolation, 3) confusion, and 4) need for supervision. More than half (55%) who move out of an assistedliving facility are admitted to a skilled nursing facility.
Purchase 250 mg lamisil mastercard. Here's Why I Quit Using Antibacterial Soap.
Major clinical manifestations of diabetic autonomic neuropathy include hypoglycemia unawareness antifungal regimen discount lamisil 250 mg overnight delivery, resting tachycardia fungus youtube generic 250mg lamisil with mastercard, orthostatic hypotension antifungal susceptibility testing generic lamisil 250 mg with mastercard, gastroparesis antifungal inhaler discount lamisil 250 mg fast delivery, constipation antifungal agents discount lamisil 250 mg otc, diarrhea antifungal cream side effects cheap lamisil 250mg with amex, fecal incontinence, erectile dysfunction, neurogenic bladder, and sudomotor dysfunction with either increased or decreased sweating. Gastrointestinal Neuropathies Gastrointestinal neuropathies may involve any portion of the gastrointestinal tract with manifestations including esophageal dysmotility, gastroparesis, constipation, diarrhea, and fecal incontinence. Gastroparesis should be suspected in individuals with erratic glycemic control or with upper gastrointestinal symptoms without another identified cause. Although the evidence for the benefit of near-normal glycemic control is not as strong for type 2 diabetes, some studies have demonstrated a modest slowing of progression without reversal of neuronal loss (16,85). Neuropathic Pain Diabetic autonomic neuropathy may also cause genitourinary disturbances, including sexual dysfunction and bladder dysfunction. In men, diabetic autonomic neuropathy may cause erectile dysfunction and/or retrograde ejaculation (76). Female sexual dysfunction occurs more frequently in those with diabetes and presents as decreased sexual desire, increased pain during intercourse, decreased sexual arousal, and inadequate lubrication (80). Lower urinary tract symptoms manifest as urinary incontinence and bladder dysfunction (nocturia, frequent urination, urination urgency, and weak urinary stream). Evaluation of bladder function should be performed for individuals with diabetes who have recurrent urinary tract infections, pyelonephritis, incontinence, or a palpable bladder. Neuropathic pain can be severe and can impact quality of life, limit mobility, and contribute to depression and social dysfunction (87). No compelling evidence exists in support of glycemic control or lifestyle management as therapies for neuropathic pain in diabetes or prediabetes, which leaves only pharmaceutical interventions. Adverse effects may be more severe in older patients (98) and may be attenuated by lower starting doses and more gradual titration. In longer-term studies, a small increase in A1C was reported in people with diabetes treated with duloxetine compared with placebo (100). Adverse events may be more severe in older people, but may be attenuated with lower doses and slower titrations of duloxetine. A recent systematic review and meta-analysis by the Special Interest Group on Neuropathic Pain of the International Association for the Study of Pain found the evidence supporting the effectiveness of tapentadol in reducing neuropathic pain to be inconclusive (88). The therapeutic goal is to minimize postural symptoms rather than to restore normotension. Dietary changes may be useful, such as eating multiple small meals and decreasing dietary fat and fiber intake. Withdrawing drugs with adverse effects on gastrointestinal motility including opioids, anticholinergics, tricyclic antidepressants, glucagon-like peptide 1 receptor agonists, pramlintide, and possibly dipeptidyl peptidase 4 inhibitors, may also improve intestinal motility (103,104). It should be reserved for severe cases that are unresponsive to other therapies (104). Erectile Dysfunction c c c c Treatments for erectile dysfunction may include phosphodiesterase type 5 inhibitors, intracorporeal or intraurethral prostaglandins, vacuum devices, or penile prostheses. C Obtain a prior history of ulceration, amputation, Charcot foot, angioplasty or vascular surgery, cigarette smoking, retinopathy, and renal disease and assess current symptoms of neuropathy (pain, burning, numbness) and vascular disease (leg fatigue, claudication). B the examination should include inspection of the skin, assessment of foot deformities, neurological assessment (10-g monofilament testing with at least one other assessment: pinprick, temperature, vibration, or ankle reflexes), and vascular assessment including pulses in the legs and feet. B Patients who are 50 years or older and any patients with symptoms of claudication or decreased and/or absent pedal pulses should be referred for further vascular assessment as appropriate. B Refer patients who smoke or who have histories of prior lowerextremity complications, loss of protective sensation, structural abnormalities, or peripheral arterial disease to foot care specialists for ongoing preventive care and lifelong surveillance. B the use specialized therapeutic footwear is recommended for high-risk patients with diabetes including those with severe neuropathy, foot deformities, or history of amputation. B and treatment of patients with diabetes and feet at risk for ulcers and amputations can delay or prevent adverse outcomes. Early recognition All adults with diabetes should undergo a comprehensive foot evaluation at least annually. A general inspection of skin integrity and musculoskeletal deformities should be performed. The selection of appropriate footwear and footwear behaviors at home should also be discussed. Treatment neuroarthropathy is the best way to prevent deformities that increase the risk of ulceration and amputation. Use of custom therapeutic footwear can help reduce the risk of future foot ulcers in high-risk patients (106,108). Wounds without evidence of softtissue or bone infection do not require antibiotic therapy. Empiric antibiotic therapy can be narrowly targeted at gram-positive cocci in many patients with acute infections, but those at risk for infection with antibiotic-resistant organisms or with chronic, previously treated, or severe infections require broader-spectrum regimens and should be referred to specialized care centers (109). Foot ulcers and wound care may require care by a podiatrist, orthopedic or vascular surgeon, or rehabilitation specialist experienced in the management of individuals with diabetes (109). Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Chronic kidney disease and intensive glycemic control increase cardiovascular risk in patients with type 2 diabetes. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. Angiotensinreceptor blockade versus converting-enzyme inhibition in type 2 diabetes and nephropathy. Cardiovascular outcomes in the Irbesartan Diabetic Nephropathy Trial of patients with type 2 diabetes and overt nephropathy. The effect of intensive treatment of diabetes on the development and progression of long-erm complications in insulin-dependent diabetes mellitus. The sensitivity and specificity of nonmydriatic digital stereoscopic retinal imaging in detecting diabetic retinopathy. Canadian Ophthalmological Society evidence-based clinical practice guidelines for the management of diabetic retinopathy. Photocoagulation for diabetic macular edema: Early Treatment Diabetic Retinopathy Study report number 1. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for S98 Microvascular Complications and Foot Care Diabetes Care Volume 40, Supplement 1, January 2017 diabetic macular edema. Evidencebased guideline: treatment of painful diabetic neuropathy: report of the American Academy of Neurology, the American Association of Neuromuscular and Electrodiagnostic Medicine, and the American Academy of Physical Medicine and Rehabilitation. Pharmacologic interventions for painful diabetic neuropathy: an umbrella systematic review and comparative effectiveness network meta-analysis. From guideline to patient: a review of recent recommendations for pharmacotherapy of painful diabetic neuropathy. C Screening for geriatric syndromes may be appropriate in older adults experiencing limitations in their basic and instrumental activities of daily living, as they may affect diabetes self-management and be related to health-related quality of life. C Annual screening for early detection of mild cognitive impairment or dementia is indicated for adults 65 years of age or older. B Older adults ($65 years of age) with diabetes should be considered a highpriority population for depression screening and treatment. B Older adults who are cognitively and functionally intact and have significant life expectancy may receive diabetes care with goals similar to those developed for younger adults. C Glycemic goals for some older adults might reasonably be relaxed using individual criteria, but hyperglycemia leading to symptoms or risk of acute hyperglycemic complications should be avoided in all patients. C Treatment of hypertension to individualized target levels is indicated in most older adults. C Treatment of other cardiovascular risk factors should be individualized in older adults considering the time frame of benefit. Lipid-lowering therapy and aspirin therapy may benefit those with life expectancies at least equal to the time frame of primary prevention or secondary intervention trials. E When palliative care is needed in older adults with diabetes, strict blood pressure control may not be necessary, and withdrawal of therapy may be appropriate. E Consider diabetes education for the staff of long-term care facilities to improve the management of older adults with diabetes. E Patients with diabetes residing in long-term care facilities need careful assessment to establish glycemic goals and to make appropriate choices of glucoselowering agents based on their clinical and functional status. E Overall comfort, prevention of distressing symptoms, and preservation of quality of life and dignity are primary goals for diabetes management at the end of life. Older individuals with diabetes have higher rates of premature death, functional disability, and coexisting illnesses, such as hypertension, coronary heart disease, and stroke, than those without diabetes. S100 Older Adults Diabetes Care Volume 40, Supplement 1, January 2017 Screening for diabetes complications in older adults should be individualized and periodically revisited, as the results of screening tests may impact therapeutic approaches and targets. Older adults are at increased risk for depression and should therefore be screened and treated accordingly (2). Diabetes management may require assessment of medical, mental, functional, and social domains. Particular attention should be paid to complications that can develop over short periods of time and/or that would significantly impair functional status, such as visual and lower-extremity complications. People with diabetes have higher incidences of all-cause dementia, Alzheimer disease, and vascular dementia than people with normal glucose tolerance (6). The effects of hyperglycemia and hyperinsulinemia on the brain are areas of intense research. Clinical trials of specific interventionsd including cholinesterase inhibitors and glutamatergic antagonistsdhave not shown positive therapeutic benefit in maintaining or significantly improving cognitive function or in preventing cognitive decline (7). The presence of cognitive impairment can make it challenging for clinicians to help their patients to reach individualized glycemic, blood pressure, and lipid targets. Cognitive dysfunction makes it difficult for patients to perform complex self-care tasks, such as glucose monitoring and adjusting insulin doses. It also hinders their ability to appropriately maintain the timing and content of diet. When clinicians are managing these types of patients, it is critical to simplify drug regimens and to involve caregivers in all aspects of care. Poor glycemic control is associated with a decline in cognitive function (11), and longer duration of diabetes worsens cognitive function. However, studies examining the effects of intensive glycemic and blood pressure control to achieve specific targets have not demonstrated a reduction in brain function decline (12). Older adults with diabetes should be carefully screened and monitored for cognitive impairment (3). Several organizations have released simple assessment tools, such as the Mini-Mental State Examination (13) and the Montreal Cognitive Assessment (14), which may help to identify patients requiring neuropsychological evaluation, particularly those in whom dementia is suspected. Annual screening for cognitive impairment is indicated for adults 65 years of age or older for early detection of mild cognitive impairment or dementia (15). People who screen positive for cognitive impairment should receive diagnostic assessment as appropriate, including referral to a behavioral health provider for formal cognitive/neuropsychological evaluation (16). Hypoglycemic events should be diligently monitored and avoided, whereas glycemic targets and pharmacologic interventions may need to be adjusted to accommodate for the changing needs of the older adult (3). Older adults are at higher risk of hypoglycemia for many reasons, including insulin deficiency necessitating insulin therapy and progressive renal insufficiency. In addition, older adults tend to have higher rates of unidentified cognitive deficits, causing difficulty in complex self-care activities. These cognitive deficits have been associated with increased risk of hypoglycemia, and, conversely, severe hypoglycemia has been linked to increased risk of dementia. Therefore, it is important to routinely screen the care of older adults with diabetes is complicated by their clinical, mental, and functional heterogeneity. Some older individuals may have developed diabetes years earlier and have significant complications, others are newly diagnosed and may have had years of undiagnosed diabetes with resultant complications, and still other older adults may have truly recent-onset disease with few or no complications (18). Some older adults with diabetes have other underlying chronic conditions, substantial diabetes-related comorbidity, limited cognitive or physical functioning, or frailty (19,20). Providers caring for older adults with diabetes must take this heterogeneity into consideration when setting and prioritizing treatment goals (21) (Table 11. Healthy Patients With Good Functional Status There are few long-term studies in older adults demonstrating the benefits of intensive glycemic, blood pressure, and lipid control. Patients who can be expected to live long enough to reap the benefits of long-term intensive diabetes management, who have good cognitive and physical function, and who choose to do so via shared decision making may be treated using therapeutic interventions and goals similar to those for younger adults with diabetes. As with all patients with diabetes, diabetes selfmanagement education and ongoing diabetes self-management support are vital components of diabetes care S101 for older adults and their caregivers. In addition, declining or impaired ability to perform diabetes self-care behaviors may be an indication for referral of older adults with diabetes for cognitive and physical functional assessment using age-normalized evaluation tools (16,22). Consideration of patient and caregiver preferences is an important aspect of treatment individualization. By "multiple," we mean at least three, but many patients may have five or more (40). Although hyperglycemia control may be important in older individuals with diabetes, greater reductions in morbidity and mortality are likely to result from control of other cardiovascular risk factors rather than from tight glycemic control alone. There is strong evidence from clinical trials of the value of treating hypertension in older adults (25,26). There is less evidence for lipid-lowering therapy and aspirin therapy, although the benefits of these interventions for primary prevention and secondary intervention are likely to apply to older adults whose life expectancies equal or exceed the time frames of the clinical trials. For patients receiving palliative care and end-of-life care, the focus should be to avoid symptoms and complications from glycemic management.
After burial the family members typically gather in one home anti fungal liquid soap order lamisil 250 mg line, often that of the deceased fungus acne best 250mg lamisil, and receive visitors fungus gnats in plants cheap lamisil 250 mg. Muslim: In Islam the deceased are buried as soon as possible sand for fungus gnats discount lamisil 250mg overnight delivery, and it is a requirement that the community be involved in the ritual fungus gnats thc cheap 250mg lamisil with amex. The individual is first washed and then wrapped in a plain white shroud called a kafan fungus on toenails quality lamisil 250 mg. The shrouded dead are placed directly in the earth without a casket and deep enough not to be disturbed. They are also positioned in the earth, on their right side, facing Mecca, Saudi Arabia. Roman Catholic: Before death an ill Catholic individual is anointed by a priest, commonly referred to as the Anointing of the Sick. The priest recites a prayer and applies consecrated oil to the forehead and hands of the ill person. The individual also takes a final communion consisting of consecrated bread and wine. The funeral mass is next which includes an opening prayer, bible readings, liturgy, communion, and a concluding rite. The funeral then moves to the cemetery where a blessing of the grave, scripture reading, and prayers conclude the funeral ritual. Green burials attempt to reduce the impact on the environment at every stage of the funeral. Grief, Bereavement, and Mourning the terms grief, bereavement, and mourning are often used interchangeably, however, they have different meanings. Grief can be in response to a physical loss, such as a death, or a social loss including a relationship or job. The time spent in bereavement for the loss of a loved one depends on the circumstances of the loss and the level of attachment to the person who died. Mourning is greatly influenced by cultural beliefs, practices, and rituals (Casarett, Kutner, & Abrahm,2001). Grief Reactions: Typical grief reactions involve mental, physical, social and/or emotional responses. These reactions can include feelings of numbness, anger, guilt, anxiety, sadness and despair. The individual can experience difficulty concentrating, sleep and eating problems, loss of interest in pleasurable activities, physical problems, and even illness. Research has demonstrated that the immune systems of individuals grieving is suppressed and their healthy cells behave more sluggishly, resulting in greater susceptibility to illnesses (Parkes & Prigerson, 2010). However, the intensity and duration of typical grief symptoms do not match those usually seen in severe grief reactions, and symptoms typically diminish within 6-10 weeks (Youdin, 2016). Complicated Grief: After the loss of a loved one, however, some individuals experience complicated grief, which includes atypical grief reactions (Newson, Boelen, Hek, Hofman, & Tiemeier, 2011). Additionally, these symptoms may last six months or longer and mirror those seen in major depressive disorder (Youdin, 2016). Those who seek assistance for complicated grief usually have experienced traumatic forms of bereavement, such as unexpected, multiple and violent deaths, or those due to murders or suicides (Parkes & Prigerson, 2010). Disenfranchised Grief: Grief that is not socially recognized is referred to as disenfranchised grief (Doka, 1989). Due to the type of loss, there is no formal mourning practices or recognition by others that would comfort the grieving individual. Consequently, individuals experiencing disenfranchised grief may suffer intensified symptoms due to the lack of social support (Parkes & Prigerson, 2010). Anticipatory Grief: Grief that occurs when a death is expected, and survivors have time to prepare to some extent before the loss is referred to as anticipatory grief. A death after a long-term, painful illness may bring family members a sense of relief that the suffering is over, and the exhausting process of caring for someone who is ill is also completed. Models of Grief There are several theoretical models of grief, however, none is all encompassing (Youdin, 2016). These models are merely guidelines for what an individual may experience while grieving. However, if individuals do not fit a model, it does not mean there is something "wrong" with the way they experience grief. It is important to remember that there is no one way to grieve, and people move through a variety of stages of grief in various ways. These "stages" are not really stages that a person goes through in order or only once; nor are they stages that occur with the same intensity. Nevertheless, these stages help us to understand and recognize some of what a dying person experiences psychologically, and by understanding, we are more equipped to support that person as they die. Denial, or disbelief or shock, protects us by allowing such news to enter slowly and to give us time to come to grips with what is taking place. The person who receives positive test results for life-threatening conditions may question the results, seek second opinions, or may simply feel a sense of disbelief psychologically even though they know that the results are true. Anger also provides us with protection in that being angry energizes us to fight against something and gives structure to a situation that may be thrusting us into the unknown. Anger can be focused on a person, a health care provider, at God, or at the world in general. It can be expressed over issues that have nothing to do with our death; consequently, being in this stage of loss is not always obvious. Living better, devoting self to a cause, being a better friend, parent, or spouse, are all agreements one might willingly commit to if doing so would lengthen life. Asking to just live long enough to witness a family event or finish a task are examples of bargaining. Feeling the full weight of loss, crying, and losing interest in the outside world is an important part of the process of dying. This depression makes others feel very uncomfortable and family members may try to console their loved one. Sometimes hospice care may include the use of antidepressants to reduce depression during this stage. Acceptance involves learning how to carry on and to incorporate this aspect of the life span into daily existence. Reaching acceptance does not in any way imply that people who are dying are happy about it or content with it. It means that they are facing it and continuing to make arrangements and to say what they wish to say to others. Some terminally ill people find that they live life more fully than ever before after they come to this stage. It is clear from her 2005 book that anger played a central role in "her" grief and did so for many years (Friedman & James, 2008). There have been challenges to the notion that denial and acceptance are beneficial to the grieving process (Telford, Kralik, & Koch, 2006). Denial can become a barrier between the patient and health care specialists and reduce the ability to educate and treat the patient. Similarly, 459 acceptance of a terminal diagnosis may also lead patients to give up and forgo treatments to alleviate their symptoms. This does not mean that others who are grieving the loss of someone would necessarily experience grief in the same way. Results indicated that acceptance was the most commonly reported reaction from the start, and yearning was the most common negative feature for the first two years. The other variables, such as disbelief, depression, and anger, were typically absent or minimal. It is often someone else who makes the decision if and when and where a patient should be hospitalized. Dual-Process Model of Grieving: the dual-process model takes into consideration that bereaved individuals move back and forth between grieving and preparing for life without their loved one (Stroebe & Schut, 2001; Stroebe, Schut, & Stroebe, 2005). This model focuses on a loss orientation, which emphasizes the feelings of loss and yearning for the deceased and a restoration orientation, which centers on the grieving individual reestablishing roles and activities they had prior to the death of their loved one. When oriented toward loss grieving individuals look back, and when oriented toward restoration they look forward. As one cannot look both back and forward at the same time, a bereaved person must shift back and forth between the two. Both orientations facilitate normal grieving and interact until bereavement has completed. Grief: Loss of Children and Parents Loss of a Child: According to Parkes and Prigerson (2010), the loss of a child at any age is considered "the most distressing and long-lasting of all griefs" (p. Bereaved parents suffer an increased risk to both physical and mental health and exhibit an increased mortality rate. Additionally, they earn higher scores on inventories of grief compared to other types of bereavement. Of those recently diagnosed with depression, a high percentage had experienced the death of child within the preceding six months, and 8 percent of women whose child had died 460 attempted or committed suicide. Archer explained that women have a greater chance of having another child when younger, and thus with added age comes greater grief as fertility declines. Certainly, the older the child the more the mother has bonded with the child and will experience greater grief. Even when children are adults, parents may experience intense grief, especially when the death is sudden. Adult children dying in traffic accidents was associated with parents experiencing more intense grief and depression, greater symptoms on a health check list, and more guilt than those parents whose adult children died from cancer (Parkes & Prigerson, 2010). Additionally, the deaths of unmarried adult children still residing at home and those who experienced alcohol and relationship problems were especially difficult for parents. Overall, in societies in which childhood deaths are statistically infrequent, parents are often unprepared for the loss of their daughter or son and suffer high levels of grief. Loss of Parents in Adulthood: In contrast to the loss of a child, the loss of parents in adult life is much more common and results in less suffering. In their literature review, Moss and Moss (1995) found that the loss of a parent in adult life is "rarely pathological. In contrast, those who are in satisfying marriages are less likely to require grief assistance (Parkes & Prigerson, 2010). To determine the effects of gender on parental death, Marks, Jun and Song (2007) analyzed longitudinal data from the National Survey of Families and Households that assessed multiple Source dimensions of psychological well-being in adulthood including depression, happiness, self-esteem, mastery, psychological wellness, alcohol abuse, and physical health. Ellis, Dowrick and Lloyd-Williams (2013) identified several negative outcomes associated with childhood grief including increased chance of substance abuse, greater susceptibility to depression, higher chance of criminal behavior, school underachievement, and lower employment rates. Typically, professional help is not required in helping children and teens who are dealing with the death of a loved one. When explaining death to children it is important to use real words, such as died and death (Dresser & Wasserman, 2010). Children do not understand the meanings of such phrases as "passed away", "left us", or "lost", and they can become confused as to what happened. Saying a loved one died of a disease called cancer, is preferable to saying he was "very sick". Consequently, it is important that children have someone who will listen to , and accurately address their concerns. We often grieve privately, quickly, and medicate our suffering with substances or activities. Employers grant 3 to 5 days for bereavement, if the loss is that of an immediate family member, and such leaves are sometimes limited to no more than one per year. Yet grief takes much longer and the bereaved are seldom ready to perform well on the job after just a few days. Obviously, life does have to continue, but we need to acknowledge and make more caring accommodations for those who are in grief. Four Tasks of Mourning: Worden (2008) identified four tasks that facilitate the mourning process. Worden believes that all four tasks must be completed, but they may be completed in any order and for varying amounts of time. Support groups reduce isolation, connect individuals with others who have similar experiences, and offer those grieving a place to share their pain and learn new ways of coping (Lynn & Harrold, 2011). Support groups are available through religious organizations, hospitals, hospice, nursing homes, mental health facilities, and schools for children. An international comparison of the percentage of deaths occurring in hospital and residential aged care settings in 45 populations, using published and available statistics.