




|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Mahmoud Houmsse, MD, FACP, FACC
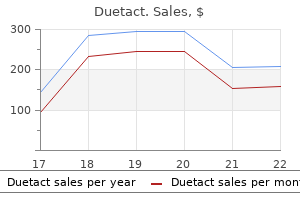
Overall diabetes symptoms neuropathy buy duetact 17 mg free shipping, rates of peritonitis were low blood sugar is low duetact 16mg without prescription, ranging from 2 to 5 percent diabetes mellitus causes discount duetact 16mg on-line, one study reported minor site infections at 59 percent and leakage at 30 percent diabetes insipidus medical alert bracelets safe 17 mg duetact. Deaths ranged from 7 to 29 percent diabetes prevention fruits and vegetables order duetact 16 mg with visa, but were considered not to be related to gastrostomy in all studies diabetic diet weight loss fast cheap duetact 16mg without a prescription. Three studies were specifically intended to analyze harms of tube feeding: one on the potential for tube feeding to induce reflux55 and two others on potential to overfeed. Clearly, surgical interventions can lead to increased weight gain; the degree to which harms outweigh those benefits likely depends on the starting point of the individual, family stressors, and the degree to which harms can be mitigated using appropriate feed and other approaches-an area that warrants continued research. In terms of overfeeding, the two studies on this subject demonstrate that tube fed children may be at risk for obesity without careful attention to the content and quantity of their food products. Effectiveness of Tube Placement With Fundoplication for Reducing Reflux No studies directly compared the use of g-tube with fundoplication to oral feeding for the treatment of reflux. Effectiveness of J-tube Compared With Fundoplication We did not identify any studies addressing this Key Question. Modifiers of the Effectiveness of Surgical Interventions We sought potential modifiers (age, race, severity, functional status, initial nutritional status, and continuous vs. Subanalyses were conducted in two case series46,48 to assess the degree to which age and type of procedure modified outcomes. In the first, children were divided into age bands of <2, 2 to 4, 5 to 7, 8 to 11 and 12 to 18. The other retrospective case series of 57 individuals48 reported that the highest proportion of individuals reaching weight for height were in the groups that had surgery before age 2, had had their gastrostomy for at least 2 years or had fundoplication. One study assessing outcomes by the presence of fundoplication suggested that use of antibiotics and respiratory hospitalizations did not differ by whether the child had a fundoplication. The surgical literature consists of a total of 11 studies meeting our criteria; studies were largely case series. Behavioral studies included in the prior review16 were small, typically short-term, and typically conducted using pre-post designs subject to bias. The authors of the systematic review used a modified Sackett approach to assess the strength of the body of evidence (see Table 5 in the full report). Effects on eating efficiency and swallowing were not consistent, and the small sample sizes suggest imprecision. The strength of the evidence for the effects of oral sensorimotor interventions and oral appliance on feeding safety and efficiency is insufficient based on a paucity of rigorous studies. Poor quality studies had positive results; whereas those with more rigor showed no effect, but may have been underpowered. Low One experimental study that was of adequate size showed some positive effects on increasing feeding safety and efficiency. Better quality studies showed positive effects, but effects were not entirely consistent; small sample sizes suggest imprecision and rigorous studies should be replicated. The low strength of evidence for the effects of gastrostomy on increasing growth measures, including weight, is based on a clearly significant effect measured in five case series and one prospective cohort study and in a small number of children. Additional data are needed on greater numbers of children to better quantify expected effects, particularly in subgroups by severity and age, and to better understand the implications of observed harms. Studies typically provided limited data on health outcomes including hospitalizations, antibiotic use, patient and family satisfaction and quality of life, measures of family stress, and pain/comfort. Evidence from this study is likely primarily applicable to younger children who are able to eat at least some foods orally. The approach studied may not closely match interventions available in practice as it was conducted in the home setting, which is likely highly variable, and was not well described. Thus, individuals wishing to infer the potential results of clinical practice based on the available research need to assess carefully the degree to which the study methods matched those available and used in practice. Those studies that provided data to characterize the participants indicated that children in the studies had experienced substantial lack of growth for up to 12 months prior to intervention. The two studies of fundoplication for reflux similarly included children, but their level of functional impairment was not clearly described. Future Research the study of feeding and nutritional interventions for individuals with cerebral palsy is a nascent field, but certainly one that is growing. Nonetheless, current research is available to provide potential directions for study. For example, studies of sensorimotor interventions currently provide conflicting evidence and more rigorous evidence is needed to answer the open question of whether they can be effective at improving outcomes. Studies should also compare behavioral interventions with one another, with extensive characterization of the participants to better understand what works for which patients. The degree to which improved changes are considered target outcomes by families is not well established. It is also not clear whether short-term outcomes translate to longer term health outcomes. The ethics of conducting comparative surgical studies or studies of nutritional interventions in the absence of appropriate comparison groups may preclude rigorous comparative designs. Case series can be conducted in ways that move them closer to providing effectiveness data; in addition, well-developed registries may provide a source of data for observational study designs. Of particular importance is the need to conduct large enough studies to fully characterize both participants and interventions so that the question of whether treatment approaches are better for individuals who, for example, aspirate or do not aspirate, can be answered. In addition to the interventions included in this review, it is necessary to consider the nutritional makeup (energy composition) of the food products themselves. Prospective, comparative studies should be carefully conducted to determine what type of nutrition is appropriate for obtaining positive health outcomes without inducing excessive weight gain. Implications for Clinical and Policy Decisionmaking the effectiveness of feeding and nutrition interventions for individuals with cerebral palsy remains largely unknown, with strength of evidence not exceeding moderate for any intervention. Nonetheless, clinical decisionmakers can use this review to understand what interventions are available, what outcomes have been seen, and, to some degree, to balance potential harms. When a child has a severe feeding disorder, is unable to consume adequate nutrition, and is affected by frequent aspiration and pneumonias, the health outcomes can be dire. Conclusions Evidence for behavioral interventions for feeding disorders in cerebral palsy ranges from insufficient to moderate. Some studies suggest that sensorimotor interventions such as oral appliances (moderate strength of evidence) and positioning (low strength of evidence) may be beneficial, but there is a clear need for rigorous, comparative studies. Longer-term, comprehensive case series are needed to understand potential harms in the context of benefits and potential risk of not treating. Prevalence and severity of feeding and nutritional problems in children with neurological impairment: Oxford Feeding Study. Caregiver stress and outcomes of children with pediatric feeding disorders treated in an intensive interdisciplinary program. Quantitative and qualitative analysis of gastroesophageal reflux after percutaneous endoscopic gastrostomy. Assessing the Risk of Bias of Individual Studies in Systematic Reviews of Health Care Interventions. Effect of oral sensorimotor treatment on measures of growth, eating efficiency and aspiration in the dysphagic child with cerebral palsy. The effect of gastrostomy tube feeding on body protein and bone mineralization in children with quadriplegic cerebral palsy. Nissen fundoplication and gastrostomy in severely neurologically impaired children with gastroesophageal reflux. Method of delivering nourishment that involves the drip of formula by gravity or assisted by a pump in an ongoing manner over a specified number of hours into a gastrostomy, jejunostomy, or gastrojejunal tube. This procedure is one of the methods used in the percutaneous placement of gastrostomy, jejunostomy, or gastrojejunal tubes. The Nissen fundoplication may be performed using a laparoscope, an instrument that is inserted through tiny incisions in the abdomen, and uses small instruments to hold a camera to look at the abdomen and pelvis, which is less invasive and promotes faster recovery but requires more technical skill. The G tube opening empties into the stomach and can be used for medication and the J-(jejunum) tube opening which empties into the small intestine can be used for feedings and water. Outreach Services of Indiana fact sheet health & safety aspiration prevention: Feeding tubes and feeding/medication administration options. National Institute of Neurological Disorders and Stroke National Institutes of Health. The motor disorders of cerebral palsy are often accompanied by disturbances of sensation, cognition, communication, perception, and/or behaviour, and/or by a seizure disorder. The diversity of the clinical features is reflected in multiple classification systems that include reference to type of motor dysfunction, body parts affected, severity, and functional abilities (see Table 1). The epidemiologic Oxford Feeding Study reported significant correlations between severity of motor impairment and feeding problems including choking, underweight, prolong feeding times, vomiting, and need for gastrostomy feeding (p values typically <0. Still, this method is common and offers a simple method of communicating the scope of impairment, which can be useful when accuracy is not necessary. Topographical Distribution · Monoplegia/monoparesis means only one limb is affected. Muscles continually contract, transition, walking, and gross motor skills making limbs stiff, rigid, and resistant such as running, jumping, and navigating to flexing or relaxing. Tongue, mouth, home, at school, and at outdoor and indoor and pharynx can be affected, as well, venues. The injury to the and balancing, but not as able as Level I to brain occurs in the pyramidal tract run or jump; may require use of mobility and is referred to as upper motor devices when first learning to walk, usually neuron damage. Requires hand-held impairments; one main characteristic mobility assistance to walk indoors, while is involuntary movement, can be slow utilizing wheeled mobility outdoors, in the or fast, often repetitive, and community and at school; can sit on own or sometimes rhythmic. Planned with limited external support; and has some movements can exaggerate the effect independence in standing transfers. Usually movements, whereas sleeping often supported when sitting; self-mobility is eliminates them. An injury in the brain limited; and likely to be transported in outside the pyramidal tract causes manual wheelchair or powered mobility. Caregiver burden is also a significant concern, as the feeding process may require considerable time and may be associated with stress and caregiver fatigue34; stress and fatigue may in turn affect the feeding process. Positioning techniques address poor postural alignment and control that exacerbates swallowing difficulties, and include stabilizing the neck and trunk. Multiple approaches may be used in children with growth failure, including sensorimotor stimulation, positioning, food thickeners, and caloric supplementation. The method of tube feeding is based on the likely time span needed for tube supplementation, the availability of an experienced surgeon, and specific symptoms of the child. For example, a child may be considered too medically fragile for surgery, so a nasal tube may be 3 used for a time, which may be advanced beyond the stomach into the jejunum to reduce gastroesophageal reflux, and then later replaced with a surgically placed tube. Limited information is available on the impact on health outcomes, including quality of life. However, these same interventions could have less value in less mobile populations that are experiencing pharyngeal dysphagia with aspiration. Additional interventions, such as positioning and caloric supplementation may still be needed. Importance of this Review Families of children with cerebral palsy face significant challenges in providing the best care for their children. The known high rates of morbidity, including aspiration and pneumonia, associated with feeding difficulties, cause substantial stress and have significant health implications. Collecting what data exist in one location, and assessing the studies objectively, will provide families and clinicians with an overview of potential interventions and what they might expect with them. When compared with other nonsurgical interventions or no intervention, how effective are nutritional interventions (food thickeners, caloric supplementation with formulas, vitamin supplementation, and altering food consistency [e. Is the effectiveness of nutritional interventions modified by age, race, severity, functional status. Organization of this Report the Methods section describes our search strategy, inclusion and exclusion criteria, approach to review of abstracts and full publications, and our method for extraction of data into evidence 5 tables and compiling evidence. We also describe our approach to grading of the quality of the literature and to evaluating the strength of the body of evidence. The Results section presents the findings of the evidence report, including data from prior systematic reviews of high quality and findings from primary studies not included in those reviews synthesized by Key Question and outcomes reported. We report the number and type of studies identified, and we differentiate between total numbers of publications and unique studies. The final section of the report discusses key findings and expands on methodologic considerations relevant to each Key Question. In addition, this review will be of use to the National Institutes of Health, Centers for Medicare & Medicaid Services, and the Health Resources and Services Administrationall of which have offices or bureaus devoted to developmental issues. Researchers can obtain a concise analysis of the current state of knowledge in this field. We drafted the initial Key Questions and analytic framework and refined them with input from key informants with expertise in child health and development, pediatric gastroenterology, occupational therapy, neurodevelopment, and developmental disabilities. During the topic development phase we identified a recent, rigorously conducted systematic review addressing behavioral feeding interventions. They included both researchers and clinicians with expertise in behavioral, medical, surgical, and allied health approaches. The framework illustrates multiple indications of disrupted nutrition among this population, including signs of malnourishment or failure to thrive, episodes of aspiration or pneumonia, swallowing difficulties, or other clinical concerns for nutritional support. Individuals typically undergo a feeding and nutrition assessment, which could be followed by a behavioral (Key Question 1a) or nutritional (Key Question 2a) feeding intervention or a combination of such approaches, or the placement of a tube for feeding (Key Questions 3ac). Individuals without pre-existing reflux who undergo a tube placement may develop reflux following the procedure44-46 and require additional treatment via a jejunostomy tube or fundoplication (Key Question 3c). Patient-centered and health outcomes following intermediate outcomes can include mortality, incidences of hospitalizations, antibiotic use, quality of life, patient and family satisfaction and stress, changes in time spent on feeding activities, physical and mental health of the primary caregiver, pain or comfort, and various adverse effects. We limited searches to literature published since 1980 to ensure that interventions used currently would be represented. Prior Systematic Reviews We identified systematic reviews retrieved by the searches for primary literature as well as through a search of the Cochrane Database of Systematic Reviews using the search terms cerebral palsy, feeding, and nutrition. Grey Literature and Regulatory Information To ensure that we captured relevant research that may not yet be published in biomedical journals, we located conference abstracts presented at annual meetings of the American Academy of Cerebral Palsy and Developmental Medicine and the American Academy of Physical Medicine and Rehabilitation (as available) from 2009 to 2012.
Diseases
The legs may hang up diabetes diet high blood sugar cheap duetact 16mg with visa, so a second helper can lift the legs to straighten the body diabetes type 2 medication list 16 mg duetact otc. Some boats will be 2 to 3 feet/60cm to 90cm up to the deck blood glucose 71 discount duetact 16mg overnight delivery, but use this same method blood glucose urine test strips 16mg duetact amex. The person being helped should be facing the helper on the deck diabetes test zeist discount duetact 17mg online, so they can communicate diabetes insipidus brain injury 17mg duetact sale, and the body naturally bends that way. The legs may need to be lifted as the person uses their elbows to crawl forward onto the deck. An able bodied diver with fins grasps the person by the legs, with their buttocks on one shoulder. A second helper on board may be necessary if the gunwale is high (2 - 3 feet / 60cm to 90cm) or the person has weak upper body strength, such as a quadriplegic. Mobility and sight-impaired divers are not able to dash around and find things just before the dive, as easily as organized able-bodied divers. If they are not organized, chances are you will be looking around trying to find their equipment. So, dive smart, and if the current is too much, swim to the surface and have the boat pick you up. Entries through the Surf are difficult, and for the handicapped diver the challenge is greatly enhanced. It is hard to say who is having more trouble here, Larry, on the left, who is paraplegic, or Gatacre, his instructor! Para Diver, in prone position, uses breast stroke to push tired buddy 1 length of pool. Para Diver, Tow buddy while Ventilating 1 length of pool, 3 strokes pinch & ventilate. Swim 5 minutes minimum - or until comfortable Make eye contact often & maintain communication. This is a pleasure dive, practice until both you and the Quad Diver are enjoying the dive. Topside Assistant place Quad Divers arm so it is not rolled on, roll Quad Diver onto back & it them up. Neutral: Circular motion applied to back of hand, followed by "ascend" if too negative, by "descend" if too positive. Air Pressure: Trace circle, followed by 1 squeeze (their air), each finger = 100psi or 10 millibar. Blind Diver performs Regulator Recovery; Sighted Buddy uses Tactile Signal for Regulator Recovery. Dive master (with four in dive team) Caution: When you are a buddy with a disability the Primary Buddy is in charge the dive! Primary Dive Buddy decides proper method for entry, location of secondary dive buddy, point of entry, etc. Position quad for descent, maintain eye contact and descend keeping diver upright. At the end of the Dive Buddy Course fill in all the information asked for, print your name and member number then Sign and date it. The purpose of this form is to insure the candidate understands the risks they are accepting when they engage in diving activities. If their response is positive to any of the conditions listed they are then required to have a physical examination and be approved for diving by a Medical Doctor. You must purchase 1 Dive Buddy Kit (Manual), paper copy or electronic, for each Dive Buddy Candidate. Certified Open Water Scuba Diver, or above, by a recognized Diver Training Agency. Logged a minimum of 20 scuba dives within 2 years prior to the starting date of Dive Buddy Course. Stay proficient in diving skills, log your dives and attempt to make at least twelve (12) dives per year. Strive to increase your diving skills through continuing education and review them in a controlled environment (a pool) after inactivity in diving. Use correct, complete, well-maintained equipment with which you are familiar and inspect it for correct fit and function prior to each dive. Know the limitations of yourself, your dive buddy(ies) and your equipment and spend time discussing your diving needs with a new dive buddy(ies). Discuss dive duration, hand signals, emergency procedures such as sharing air and the location and use of your alternate air sources. Adjust weighting for neutral buoyancy, maintain neutral buoyancy during descent, while underwater and during ascent. Be buoyant at the surface and keep the regulator mouthpiece in your mouth until you are buoyant. Make sure weights are clear for easy removal to establish buoyancy at the surface or underwater, in case of distress while diving. Use good judgment and common sense in planning each dive, set moderate limits for depth and time in the water and avoid dangerous places or poor diving conditions. Initials: Be prepared to ditch your weight belt, make an emergency ascent, clear your mask or mouthpiece or take any other emergency action needed. Initials: © 1987-2019-1hq Handicapped Scuba Association 64 Dive Buddy Manual 10. Get out of the water if you are cold, tired, injured, low on air, or in anyway not feeling well. Initials: Beware of sunburn even on overcast days, abrasions and tissue breakdown on hard surfaces while diving and after being in the water. Never buddy assist a diver if for any reason you are uncomfortable with your equipment, yourself or the diver. Always use the three (3) person buddy system when diving with a Level B or Level C diver. Thoroughly understand the equipment and capabilities of both the diver you are assisting and your secondary dive buddy. Be proficient in dive table and dive computer use, decompression and emergency procedures. Make all dives no-decompression dives and always allow a margin of safety by staying well within the no-decompression limits. Have a means to monitor depth and time while underwater and ascend at a rate of 30 feet /9m per minute or slower. Always decompress at 15 ft/5m for three (3) minutes when diving at a depth deeper than 60 feet/18m. Use a boat or float as a surface station whenever this will increase the safety of the dive. Fly the diver-down flag and surface close to the boat or surface station, while watching and listening for possible hazards. Be aware of current changes during the dive, use natural clues such as seaweed or look for current lines trailed behind the boat at the surface. Always plan your dive into the current, then at the end of the dive you can return with the current. When boat diving, select a licensed boat that is fully equipped with the required safety equipment and Oxygen. Only sign up for trip destinations that are consistent with your training and experience. These safety rules and procedures will be covered in detail during your scuba-training course. This is called an Air Embolism and it can cause very serious injuries, even death. Ears: Your ears may experience some pressure, or even hurt, when you descend underwater. This is normal, and you have probably already experienced this pressure in your ears if you have dove underwater, flown in an airplane, or driven in the mountains. The pool and open water environments have hard and abrasive surfaces that can cause abrasions and tissue breakdown for people with reduced circulation. Dive Duration: Because you are breathing compressed air underwater your body fluids and tissues absorb more nitrogen than at sea level. Hard Surfaces: Place padding, such as an exercise mat or towel, on pool and boat deck surfaces, and on other hard surfaces, to protect the skin, if needed. Transfer from your wheelchair: Be sure to tell those assisting your transfer what method you use, and then have them explain what they intend to do before they assist you. Have them lift your legs (not drag them) at the knee, so that your legs bend naturally. Be sure to tell them if you have poor balance and to provide support until you are stable. Swimming too fast to the surface can cause an Air Embolism, which is very serious. Recompression Chamber: A recompression chamber is needed to treat various diving related injuries, primarily Decompression Sickness and Air Embolism. I understand that diving with compressed air involves risks of decompression sickness, embolism or other hyperbaric injuries that require treatment in a recompression chamber. I further understand that these diving activities may be conducted at sites that are remote by time and distance from a recompression chamber. Additionally, I understand that there are also risks involved with dive travel, including, but not limited to , dive boat accidents, and traveling to and from the dive sites. Nevertheless, I choose to proceed with such diving activities and I freely accept and expressly assume all risks, dangers and hazards that may arise from such diving activities which could result in injury, loss of life and property damage to me. In consideration of being allowed to participate in these diving activities, as well as the use of any facilities and the use of equipment, I hereby personally assume all risks in connection with said diving activities, for any harm, injury or damage that may befall me while I am participating, including all risks connected therewith, whether foreseen or unforeseen. I further save and hold harmless said diving activities and Released Parties from any claim or lawsuit by me, my family, estate, heirs, or assigns, arising out of my participation in these diving activities including claims arising during or after the diving activities. I also understand that snorkeling, skin diving and scuba diving are physically strenuous activities and that I will be exerting myself during the diving activities, and that if I am injured as a result of, but not limited to , a heart attack, panic, or hyperventilation, that I expressly assume the risk of said injuries and that I will not hold the Released Parties responsible for the same. I hereby declare that I am of legal age and competent to sign this agreement or, if not, that my parent or guardian shall sign on my behalf, and that my parent or guardian is in complete understanding and concurrence with this agreement. I hereby state and agree that this agreement will be effective for all diving activities in which I participate until revoked in writing by the Released Parties. A positive response to a question does not necessarily disqualify you; it simply means you must seek approval from a doctor before engaging in diving activities. I agree to accept responsibility for omissions regarding my failure to disclose any existing or past health condition. Based on a physical examination, your opinion of the applicants Medical Fitness for scuba diving is requested. The answers to the following questions will give us a "general" accessibility profile of your Resort/Hotel facilities. However, because barriers to accessibility are often subtle and difficult to assess, it is impossible to give an accessibility rating without an on-site inspection. Yes No Yes No How many Step height inches/cm Is there a ramp? Yes No Grade R L inches/cm Doorway width inches/cm. Door opens to inside; does it block the; Width inches/cm Yes No Pocket Door Yes No Wash basin Bathtub Toilet Can it be opened and closed from the inside while in a wheelchair? Yes No Access Space (36 inches/90 cm) next to door inches/cm Clear floor space area, minimum turning area is 5 ft/150 cm x 5 ft/150 cm. Access space inches/cm o Standard height l6 inches/40 cm to l9 inches/48 cm. Toilet height inches/cm o Is there a padded multi-positional seat available? Shower, control knobs within reach; Height 36-40 inches/90-100 cm Length, reach distance from faucets Yes No Height inches/cm Yes No Yes No Height inches/cm Reach inches/cm Yes No Yes No Height inches/cm Drain in bathroom floor? Doorway width inches/cm Bed height, 22 inches/55 cm for independent transfers into and out bed. Bed height inches/cm Bed space, minimum distance from one wall is 36 inches/90 cm. Yes No Telephone access, passageway to telephone at least 32 inches/80 cm. Passageway width inches/cm Light control switches; height 36 inches/90 cm to 40 inches/100 cm high. Yes No Opens degrees the refrigerator is in a corner with one side blocked by a wall or cabinet, the door will open to l80 degrees? Yes No Opens degrees Is there a 36 inches/90 cm wheelchair access space? Yes No Grade R L inches/cm Is there a smooth pool deck area, minimum width 5 ft/1. Yes No Width inches/cm Is there a walkway across the sand to the water? Yes No Width inches/cm Is the sand on the beach "hard packed? Sand Rock other Special considerations: Access to shore dive site is: Are there any other barriers? Yes No Clear deck area feet/meters X feet/meters o o Is there shade available? They are also available for Instructor referral, training advice and various other related services. This is a question that many dive professionals have, and for which there are many inaccurate answers. Inglis of South Carolina introduced the following bill; which was referred to the Committee on the Judiciary. The Congress finds and declares that-(1) the willingness of volunteers to offer their services is deterred by potential for liability actions against them and the organizations they serve; (2) as a result, many nonprofit public and private organizations and governmental entities, including voluntary associations, social service agencies, educational institutions, and other civic programs, have been adversely affected by the withdrawal of volunteers from boards of directors and service in other capacities; (3) the contribution of these programs to their communities is thereby diminished, resulting in fewer and higher cost programs than would be obtainable if volunteers were participating; and (4) because Federal funds are expended on useful and cost-effective social service programs, many of which are national in scope, depend heavily on volunteer participation, and represent some of the most successful public-private partnerships, protection of volunteerism through clarification and limitation of the personal liability risks assumed by the volunteer in connection with such participation is an appropriate subject for Federal legislation.
Buy discount duetact 17 mg on line. Information for parents whose baby may be at risk of low blood sugars.
Built of sturdy materials so that it can contain participants and equines during a lesson (rope diabete 97 discount duetact 16mg line, barbed or slick wire diabetes prevention china quality 17 mg duetact, electric wire or tape is not acceptable)? The support posts of the outdoor arena should be located on the outside of the arena fencing metabolic disease laboratory uab duetact 16mg fast delivery. Support posts or any exposed beams of indoor arenas should be protected with a padded covering or covered by kick boards managing diabetes chart generic duetact 16 mg amex. Every effort should be made to minimize the risk of injury to participants diabetes medications classes discount duetact 16 mg with visa, equines and personnel metabolic endocrine disease summit 2013 purchase duetact 17mg. Is there an implemented procedure to ensure that each arena is clear of objects that might injure equines, participants and personnel? Unnecessary equipment, structural elements and natural hazards that are not utilized during the session should be cleared from the arena. Is there an implemented policy to ensure that grooming and tacking areas and/or aisles are clear of obstacles, accessible and spacious enough to allow freedom of movement for participants, volunteers and/or personnel for safety and performance of activities? Grooming and tacking areas can be a stall, cross-tie area, wash stall or hitching post. If the center serves participants in wheelchairs, there should be sufficient space to allow wheelchair accessibility for adequate clearance to both sides of the equine and for movement away from the equine in the event of emergency. Aisles need to be wide enough for equines and individuals to pass without contact. Compliance Demonstration: Visitor observation of grooming and tacking areas while in use by participants and personnel. F33 Is there an implemented procedure to minimize distractions or disruptions in and around the activity/treatment area while in use? Yes No Interpretation: Controlling the amount of distractions in the arena as well as in the area surrounding the arena helps maintain participant attention. Standards for Certification & Accreditation 2018 67 F34 Is there a system to minimize exposure to dust in the activity area? Yes Interpretation: Excessive exposure to dust for both humans and animals may create health problems. A system of control may include watering the surface, type of surface utilized, additives to footing for moisture retention, scheduling, restricting use of areas, etc. Compliance Demonstration: Visitor observation of arena(s) and personnel explanation of system. Placed in a location convenient to , but not within, the working area of the arena? Designed and constructed of materials of a strength and size to accommodate the participants, personnel, equipment and activities for which they are used? Set up with a second physical barrier, placed parallel approximately 28" to 36" from the mounting side of the mounting ramp, to keep the equine in alignment with the ramp during mounting procedures? To determine space, strength and size of the ramp, consider the number of personnel used in the mounting process as well as the types of wheelchairs and adapted equipment used. Other factors to consider include the following: activities offered, population served and the ability to provide progressive mounting. The mounting ramp should be separated from the working area by a visual barrier that is clearly visible to equines, participants and volunteers, such as cones, poles, etc. An offside barrier is used in order to prevent the equine from swinging away from the ramp. A person should not be the offside barrier due to safety considerations for the individual. Designed and constructed of materials of a strength and size to accommodate the participants, personnel, equipment and activities for which it is used? To determine space, strength and size of the block, consider the number of personnel used in the mounting process as well as the types of wheelchairs and adapted equipment used. Other factors to consider include activities offered, population served and the ability to provide progressive mounting. The mounting block should be separated from the working area by a physical barrier that is clearly visible to equines, participants and volunteers, such as cones, poles, etc. Designed and constructed to accommodate the participants and activity for which it is used? The working area is defined as those locations where mounted lessons are being held. The mechanical lift should be separated from the working area by a physical barrier that is clearly visible to equines. Compliance Demonstration: Visitor observation of the use of the mechanical lift and interview of personnel. Has the center implemented a program of training and rehearsal in utilizing the lift that prepares personnel, equines, volunteers and participants for the normal and emergency operation of the lift, and is a written list of trained personnel and equines maintained? The center administration should determine appropriate rehearsal intervals for safety regulations. Is there written evidence that a systematic maintenance routine is in effect to ensure that the lift and all related equipment is safe and in good repair? Equipment that is not in good condition should be removed from service immediately. Does the instructor ensure that a lift equipment safety check is conducted at the beginning of each use? Are there written safety and emergency procedures directly related to the use and operation of the lift? Personnel directly involved in the use of the lift should have knowledge of the safety and emergency procedures. Sufficiently padded, free of sharp and/or protruding objects and includes built-in or attached handles? The vaulting barrel may be used for other activities such as participant evaluations, warm-up activities, volunteer training or other uses in addition to vaulting. The support of the barrel should not interfere with the movement of the participants while mounting or dismounting. Handles should be protected for safety and comfort of the user (for example, may be wrapped with vet wrap or duct tape). Some prefer to construct the vaulting barrel without built-in handles and add a surcingle on the barrel to provide the handles in a more realistic manner. The vaulting barrel needs to be stable enough to avoid tipping over when used vigorously. Compliance Demonstration: Visitor observation of the vaulting barrel(s) and interview of personnel. Evaluation of the suitability of new equines prior to participating in center activities/ therapies? Evaluation for the permanent removal of equines no longer/not suited for participating in center activities/therapies? Yes Interpretation: Having written standard procedures for evaluation and removal of equines provides centers an unbiased tool for effective measurement of the abilities and suitability of all equines participating in center activities/therapies. The written procedures for intake suitability should delineate the following: · Who is the ultimate decision maker? Once these written procedures are developed and implemented, they should be reviewed and modified as needed, as long as the written procedures match center practices. It is understood that the quality of the results achieved in hippotherapy are directly related to the quality of movement of the hippotherapy equine. It is important to maintain the suppleness and strength of the hippotherapy equine through training and conditioning. The equine has to become gradually accustomed to the distribution of weight behind the center of gravity and desensitized to the input of the additional leg pressure near the flank. Compliance Demonstration: Visitor interview and personnel description of training and conditioning program. Does the equine training and conditioning program for interactive vaulting also include the following: 1. Ongoing training to varied vaulting exercises and movement games on and around the equine? A progressive training and conditioning program is one that allows the equine to build skills based on previous training sessions. Strength and endurance must be developed over a period of time for the equine to become comfortable performing the work that is being asked. The equipment and activities used are specific to the discipline and require additional training to ensure safety. Check for changes in physical soundness and behavior of each equine prior to its assignment to an activity or therapy session so as to ensure that the equine is able to perform as needed? Make assignment and proceed with session as scheduled or remove equine from participation in session(s) until soundness and behavior issues can be addressed? Equines with underlying soundness issues or other health problems that negatively impact their ability to work should be removed from activity or therapy sessions until their problems can be resolved. Compliance Demonstration: Visitor observation and personnel description of procedures. Written records of the number of hours and types of sessions for each equine per day? Yes No Interpretation: A Some equines may not be conditioned sufficiently to maintain a schedule based on current recommendations for a specific activity or therapy and will need additional adjustments in scheduling. Centers may set any workday/continuous hour limit policy as long as it is implemented by the center and does not exceed the maximum. Centers may want to consider giving each equine a day off per week as working with participants may be stressful. Consideration should be given to the size and type of participant served when scheduling each equine. A record should be kept of the number of hours and in what capacity each equine works, whether it is ground, mounted, driving, interactive vaulting, hippotherapy, tandem hippotherapy, psychotherapy sessions, etc. Many activities have additional scheduling recommendations that should be followed. As climate, equine conditioning and center activities/therapies vary considerably from center to center, each center should define "lengthy break" for themselves. The definition of "lengthy" does not need to be written, but center personnel should be consistent in their definition. Are there current, written equine health records available on-site that include the following: 1. Is there a written feed chart for each equine easily accessible to the person feeding? Centers may find more than one activity that describes how their programs are delivered. Mounted activities may be part of programs in therapeutic riding, hippotherapy, tandem hippotherapy or mounted equine-facilitated psychotherapy, in addition to others. Ground activities may be used in equinefacilitated psychotherapy, therapeutic riding, interactive vaulting, driving, hippotherapy or other equine activities and therapies. Instructor Certification at the registered, advanced or master level demonstrates compliance with this standard. Yes No Interpretation: For the safety of the participants, the personnel mounting and dismounting should be designated and trained to be familiar with proper mounting techniques, disabilities, body mechanics and individual equine personalities. The written policy may address use of safety stirrups, use of boots by participants or both. Examples may be the handle of a surcingle, a properly fitting neck strap or other reliable tack. Yes No Interpretation: this standard applies to all participants engaged in center mounted activities. It is recommended that participants also wear helmets during groundwork conducted with or near equines. Helmets not approved for equestrian use must have written documentation that meets the Guidelines for Alternative Helmet Use found in the Guideline section of this manual. Standards for Certification & Accreditation 2018 Driving Standards Centers with existing driving programs and those considering adding a driving program should also review the following standard sections for standards that may impact their driving program: Core Administration and Business, Facility and Equine Welfare and Management contain standards that may apply to a driving program. Equestrian Skill Standards can be found in the Service section of the Standards manual and apply to driving activities since the goal for the participant is to gain the equestrian skill of driving. To select an appropriate equine for driving activities, review the Equine Selection Criteria for driving found in the Guideline section of the standards manual. Yes No Interpretation: A lead rope should be available for ease of control by the header. This can be attached to any type of halter, a head collar with a ring or a ring attached to the noseband. Yes No Interpretation: the motion provided by the suspension and balance of the vehicle should be appropriate for the participant. Participants must be able to brace their feet or be otherwise supported and may need a footrest. Traditional vehicles with easy access may be used for semi-ambulatory participants. Compliance Demonstration: Visitor observation of vehicles and personnel description of procedures. Require the presence of the Professional Association of Therapeutic Horsemanship International Certified Driving Instructor? Yes No Interpretation: Each program should establish procedures so that participants can quickly and safely enter and exit from each vehicle. These procedures will vary from vehicle to vehicle and should include but not be limited to the following: 1. Holds the reins and takes control of the equine before the participant enters and remains in the vehicle until after the participant exits? Has a second set of reins to take control of driving the equine during the session if needed? Reins for the participant may be attached to the halter, terrets, saddle rings or bit depending on his/her skill level.
Spartium scoparium (Scotch Broom). Duetact.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96389