




|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Ronald Belczyk, DPM
Transmission of these viruses via fomites does not appear to be a significant risk in the setting of natural outbreaks man health 7 muscle gain order eulexin 250mg on line, but may be greater in laboratory settings (8 prostate fluid color eulexin 250mg online, 9) prostate cancer lancet oncology cheap eulexin 250 mg visa. Specifically prostate cancer vaccine buy eulexin 250mg fast delivery, Ebola virus persists for longer periods on surfaces when environmental factors such as temperature and relative humidity are controlled mens health x factor purchase 250mg eulexin mastercard, and also has a longer half-life on surface materials such as Tyvek which are more common in laboratories (9) mens health urbanathlon training eulexin 250mg mastercard. Standard (universal) precautions denote the basic practices that should be employed to prevent contact or bloodborne transmission of pathogens within the hospital and clinical laboratory. It is important to note that biological safety procedures performed in hospital and clinical laboratories are different than hospital infection control guidelines. In essence, standard (universal) precautions in hospital and clinical laboratories stipulate that all human specimens (respiratory, blood, tissue, stool, etc. Implementation of standard (universal) precautions involve both procedural and engineering controls (discussed in detail in "Engineering and Procedural Controls" section), as well as general safe laboratory practices. Additional components of standard precautions may vary based on the risk assessment 26 associated with the specimen type and laboratory procedures being conducted, but may include the use of gloves, face shields, or respiratory protection. Safe laboratory practices are a procedural control that reduce contact transmission and serve as the basis for preventing laboratory acquired infections. Clearly defining and demarcating "clean" and "dirty" areas within a laboratory with physical barriers (walls, doors), signage, or other visual cues aids in alerting employees and visitors to locations where standard precautions need to be observed. Hand hygiene practices should be rigorously followed whenever the is a recognized exposure to clinical material and before exiting the laboratory. Proper hand washing technique consists of at least 20 seconds of scrubbing all surfaces of hands using soap and clean water. Some experimental data have suggested the use of soap containing antimicrobial agents such as triclosan or chlorhexidine gluconate may be superior to standard soap and alcohol gels, reducing bacterial counts on the hands by 70-99% depending on the antimicrobial and frequency of use (10). Eating, drinking, or storing food products in the laboratory should be forbidden because of the risk of direct contact with contaminated surfaces, including unwashed hands. Similarly, the use of personal electronics such as digital music players or cellular phones should be restricted. These are "high touch" items that can become easily contaminated by soiled hands or gloves during routine laboratory work and have the potential to spread microorganisms outside of the laboratory. Disposable gloves reduce the risk of unrecognized contact transmission when manipulating specimens and should always be worn when handling primary specimen containers. For example, latex gloves are adequate for incidental contact with clinical specimens but are not sufficient for handling of solvents. Additionally, punctures may be difficult to detect and latex can cause allergic reaction in some people. For these reasons, many laboratories use nitrile gloves which are non-allergenic and better withstand contact with solvents. When using disposable gloves, it is good practice to check for rips or punctures before use. Gloves should be removed and changed if visibly soiled and prior to touching objects such as keyboards, phone receivers, door knobs, or water faucets. Dedicated laboratory coats provide an important physical barrier between the laboratory environment and personal "street" clothing or scrubs, which are worn outside the laboratory. Laboratory coats should be impervious to liquids and ideally be snug fitting at both the wrist and collar to provide the maximal level of protection. This barrier can be especially important in the event of unexpected splashes or spills involving liquid specimens. Accidental needle stick or other sharps injury can present the highest risk of laboratory acquired infection through direct inoculation of microorganisms to sterile sites including the bloodstream. Laboratories should have policies in place to address specimens received in syringes with the needle still attached. This may include a strict rejection policy for such specimens as well as notification of the individual, supervisor, or medical director of the hospital unit or clinic submitting the specimen. The use of blunt needles is encouraged for laboratory procedures requiring syringe transfer of liquid specimens. If standard needles are necessary, they should never be recapped and ideally should be equipped with a safety device that can be activated before discard. All sharps, including needles, broken glass, and razor blades should be discarded in hard sided, puncture resistant containers. This will prevent difficulty when discarding sharps and will reduce the chance on injury when sealing the container for disposal. All potential bloodborne exposures involving sharps or contact between a specimen and mucous membrane or non-intact skin should be immediately reported and referred to an occupational health office for assessment of exposure and risk of infection. Most commonly, these include respiratory pathogens present in secretions generated through talking, sneezing, or coughing. Because infection requires direct contact with infectious droplets, natural droplet transmission is restricted to a zone within 3-5 feet of a contagious individual. Highly pathogenic emerging respiratory viruses such as novel strains of influenza A. Importantly, these pathogens are often sensitive to desiccation and other environmental stresses and have limited viability on surfaces. Environmental persistence of influenza is both strain and condition dependent, but typically decreases 2-5 log10 within 24-48 h (11, 14, 15). These data suggest that the risk of contact transmission may be reduced when compared to more hardy organisms; however, laboratory surfaces where specimens containing these organisms are frequently handled still present a potential source of transmission. Many of the laboratory procedures commonly employed during initial processing or downstream manipulation of clinical specimens or cultures have the potential to generate infectious droplets. Specific examples include venting of positive blood culture broths for gram stain and culture inoculation, performance of the catalase test on culture isolates, centrifugation to concentrate specimens, vortexing of isolates to make a bacterial suspension, and the practice of "hot looping" (touching a heat sterilized inoculating loop to agar plate to speed cooling). Unlike natural generation of droplets through coughing or sneezing, mechanical manipulations produce droplets with larger size variation. This impacts both the settle rate and the number of infectious organisms that can be contained in each droplet. Larger droplets will typically settle faster and have a narrower zone of transmission, but can carry a larger number of 28 microorganisms. Conversely, smaller droplets (referred to as aerosol or micronuclei) may take longer to settle which increases the range of transmission beyond the generally accepted 3-5-foot zone. This puts a larger proportion of the laboratory and more laboratory staff at risk of infection, especially when considering microorganisms such as Brucella spp. The attack rate was 40-60% for persons working directly with cultured bacteria; however, 20% of labortorys staff without direct contact also acquired brucellosis. Because of similarities in growth rate, requirement for specific nutrients, and gram stain morphology, F. In light of the recent outbreak of Ebola virus in Western Africa, much attention has focused on the route of transmission to healthcare workers treating these patients, as well as to laboratory workers that handle clinical specimens. Blood borne and direct contact transmission via bodily fluids is associated with a high attack rate and can carry a mortality rate of up to 90% (2). The risk of droplet transmission is likely dependent on the stage of infection (viral load in bodily secretions is highest during the acute phase of infection) and presence of clinical symptoms such as severe diarrhea, vomiting, and severe coughing, all of which can generate infectious droplets. Healthcare workers caring for patients are likely at a higher risk of infection due to the uncontrolled and unpredictable nature of the environment and patient, as well as the medical procedure that may be necessary to care for these patients such as ventilation, mechanical resuscitation, and placement of intravenous catheters. Several cases of laboratory acquired Ebola virus infections have been reported, but these have been restricted to direct percutaneous exposure, primarily in research laboratories (20). The use of sealed rotor centrifuges is another engineering control that should be used to mitigate the release of infectious aerosols. Since droplets are relatively large, the use of surgical or other non-N-95 type masks are acceptable to prevent transmission. Working with specimens behind a clear Plexiglas shield on the benchtop also provides a barrier to droplet transmission; however, this approach may create a false sense of security since small aerosols may extend beyond the edges of the barrier. Other general procedural controls can further minimize the risk of aerosol exposure when working with infectious specimens. Tubes with snap-type lids should be avoided in favor of threaded screw-on caps to reduce creation of droplets when these containers or opened. Further, gauze pads can be used when opening specimen containers to mitigate aerosols released by surface tension bubbles at the mouth of the container. When using a manual pipette, the retention volume should not be expelled since this can be a source of aerosol. This will ensure contact between the agent and disinfectant and reduce the risk of infectious aerosols when ejecting the pipette tip. Microorganisms associated with airborne transmission are typically small, ranging from 1-10 µm in diameter, and are resistant to environmental stresses including heat and desiccation (21). This enables transmission on air currents over long distances (>1 m) and for extended periods of time. Rubeola (measles), Variola (smallpox), Varicella (chickenpox), Mycobacterium tuberculosis, Hantavirus, bacterial endospores. The source of airborne transmission can be aerosol micronuclei, but may also be dust, skin flakes, or the naked organism itself. When delivered via airborne route, inhalation of as few as 10 of these organisms can cause disease with mortality rates of 40-99% if untreated (2). However, transmission may occur through generation of micronuclei during medical procedures such as mechanical ventilation or during episodes of projectile vomiting or diarrhea. Prevention of airborne transmission within the hospital and laboratory relies on directional airflow and physical containment specimens and cultures. Negative pressure is measured as the difference in pressure between two adjacent rooms, and should be > 0. If maintained, negative pressure contains airborne pathogens within the designated room and prevents exposure events within the main laboratory. If a spill occurs, sufficient time should be allowed to reduce the presence of airborne contaminants by 99% (23). A paper towel soaked in disinfectant can be used to initially cover the spill and inactivate microorganisms prior to a more thorough decontamination and cleaning protocol. Unlike masks recommended for prevention of droplet transmission, respirators must effectively prevent inhalation of small airborne particles. Therefore, these respirators must be tight-fitting around the nose and mouth and remove >95% of particulates 0. Importantly, these respirators should only be used after appropriate training and fit testing to ensure maximal protective benefit. Disposable N-95 respirators are adequate for relatively low risk activities such as processing of respiratory specimens or cultures suspected to contain M. Additional respiratory protection may be warranted if working with pure cultures or specimens suspected to contain higher risk group pathogens such as Ebola, or for laboratory staff who cannot wear standard N-95 type respirators (see section 4. The functionality of the blower pack should be tested prior starting work with clinical specimens using a "floating ball" air tube to ensure a constant airflow rate of 115-170 liters/min (26). Included in this policy should be instruction for hospital or provider group(s) to notify the laboratory when diagnostic specimens are collected from patients with symptoms and/or history compatible with these agents. These exposures and resulting infections are often attributable to a low index of suspicion for these agents or failure of the hospital service to notify the lab when there is a compatible patient history and/or clinical presentation. Failure to notify the laboratory of a case of presumed acute pulmonary tularemia resulted in exposure of 11 laboratory workers to cultures of F. It also underscores the need to implement and maintain protocols for safe work practices that pertain to all clinical specimens and cultures. Always perform a risk assessment for all procedures performed in the laboratory and remember to continually update the risk assessment over time. Specimen containers that are visibly leaking pose an increased risk of transmission, but also indicate potential external contamination of the specimen. This is the result of a higher concentration of organism and the conduct of aerosol-generating procedures during routine identification of culture isolates (see section 4. These factors contribute to the increased relative risk of infection among laboratory workers, ranging 8. These exposures may be the result of poor airflow, disturbance of laminar flow, or other unrecognized mechanical or work practice failure. Any procedures that have the potential to generate aerosols or droplets should be avoided. This includes the use of vortex, centrifugation and, forceful pipetting to make bacterial suspensions. These systems rely on biochemical and phenotypic properties, molecular, or protein-based analyses to identify these microorganisms. In many cases, this necessitates subculture of a single colony of interest to achieve sufficient biomass for testing and to ensure purity of the isolate. This step not only exposes the technologist to potentially infectious agents through manual subculture, but also creates a high concentration culture of the isolate which further increases the risk of infection. The combination of concentrated bacterial suspensions and the potential for generating aerosols results in a high risk of laboratory acquired infection when using these test systems. Finally, isolates of Brucella melitensis and Brucella suis have been misidentified as Ochrobactrum anthropi or Bergeyella zoohelcum (3234). These misidentifications can be misleading to the clinician and put laboratory workers at risk of exposure and infection (16, 32). Characteristics including rapid, accurate identification of bacteria and yeast, as well as a low cost per identification have driven initial uptake in large academic or reference laboratories capable of evaluating and validating this new technology. However, unlike these systems, a single well-isolated colony is sufficient for identification. This eliminates the need for subculture and preparation of high concentration suspensions, thereby reducing the risk of laboratory acquired infection during pre-analytic steps. Therefore, it is critical that any potentially infectious organism has been inactivated. Several methods have been evaluated to inactivate vegetative bacterial cells as well as highly resistant endospores such as those produced by B.
Peritonsillar abscess (Quinsy) · Sometimes a serious complication of exudative pharyngitis · Surgical drainage is required in treatment mens health zone eulexin 250 mg without a prescription. Deep Neck Abscess/ Retropharyngeal Abscess · Surgical drainage is required in treatment mens health living generic eulexin 250mg otc. These cases have a predominance of superficial infections mens health life cheap eulexin 250mg on-line, including subcutaneous abscesses prostate oncology specialists in ohio order eulexin 250 mg mastercard, cellulitis prostate cancer articles buy 250 mg eulexin otc, and recurrent skin infections prostate knot effective eulexin 250 mg. Membranous pharyngitis due to diphtheria · Intensive surveillance and immediate notification to the Department of Health is necessary. Vaccine containing diphtheria toxoid is available in combination with tetanus and pertussis. Routine pediatric immunization should include 5 doses given on ages 6 weeks, 10 weeks, 14 weeks, 12 months (provided there is a minimum interval of 6 months from dose 3) and 4-6 years before school entry. Eradication of the organism should be documented 24 hours after completing treatment by 2 consecutive negative cultures from pharyngeal specimens taken 24 hours apart. If follow-up cultures are positive, erythromycin should be given for an additional 10 days. Vesicular, ulcerative pharyngitis (viral) · More common in patients aged < 3 years · Associated signs and symptoms: o Consistently present: Hoarseness, cough, colds, conjunctivitis, ulcerative stomatitis. Lemierre described Fusobacterium in 1936; other anaerobes and Gram (+) cocci are less common etiologies of suppurative phlebitis postpharyngitis. Note: If not a complication of pharyngitis, and if there is an internal jugular line, treat empirically for methicillinresistant Staphylococcus aureus using vancomycin. May present with life-threatening upper airway obstruction, especially in pediatrics. On its own, erythromycin has poor coverage for Gram (-) bacteria and may not cover for H. The same holds true for clindamycin; however, it makes up for this with the added coverage against anaerobic bacteria. These considerations should be taken into account when prescribing these antibiotics. Mucormycosis: diabetes mellitus with acute ketoacidosis; neutropenia; deferoxamine therapy adults only Early diagnosis is key to treatment success. Symptoms suggestive of fungal sinusitis (or lateral facial pain or numbness) should increase suspicion. Palatal ulcers and/or black eschars and unilateral blindness in immunocompromised or diabetic patients suggests mucor. Complete or partial response rates with Posaconazole salvage protocols is from 60% to 80%. Resistant to Voriconazole: prolonged use of Voriconazole prophylaxis predisposes to mucormycosis infections. Posaconazole may be used for secondary prophylaxis for those on immunosuppressive therapy. Acute sinusitis in adult hospitalized patients with nasotracheal or nasogastric intubation Etiology: Gram negative bacilli (Pseudomonas, Acinetobacter, E. Comments: Treatment is usually with antibiotic therapy for 3 to 6 or up to 10 weeks with appropriately selected agents, but the efficacy of this approach is controversial. A: Ofloxacin ear drops 10 drops/d x 7d Comments: Treatment of choice should be based on factors such as patient allergy, risk of ototoxicity, bacterial resistance, availability, cost, and dosing schedule. For chronic otitis externa (symptoms 6 weeks to >3 months), treatment involves debridement and application of topical anti-inflammatory agents. A: Clotrimazole 1% solution 2-3 drops q8- 12h up to 10-14d Comments: Debridement and dry ear hygiene is crucial in otomycosis. A 1:1 white vinegar + rubbing alcohol solution may be instilled in the external ear canal after swimming to restore proper acidic pH to the ear canal and to dry residual water. Necrotizing otitis externa · Very high erythrocyte sedimentation rates are typical. Treatment from other etiologies should be guided by antibiotic susceptibility results. A: Ofloxacin ear drops 10 drops 1-2x/d x 7d Comments: Ointments should not be used in the ear. For chronic otitis externa (symptoms 6 weeks to > 3 months), treatment involves debridement and application of topical anti-inflammatory agents. Primary vaccination involves 3 doses with an interval of 4 weeks in between doses. Booster is given at age 12-15 months, with an interval of 6 months after the 3rd dose. There may be favorable results in mostly afebrile patients with waiting for 48 hours before deciding to use antibiotics. For patients allergic to -lactam drugs: · If history unclear or rash, may give effective oral cephalosporin · If IgE-mediated allergy. For severe disease, appropriate duration of treatment is unclear, but 5 days may be inadequate. Additional comments for pediatric patients: Co-amoxiclav and Ceftriaxone may be used as a first-line agent if at the onset, the child presents with high fever >39oC and/or if with severe otalgia. If infection is non-responsive to antimicrobial therapy, tympanocentesis or myringotomy may be necessary. Persistent middle ear effusion for 2-3 months after therapy is expected and does not require retreatment. Definition of failure: no change in ear pain, fever, bulging tympanic membrane or otorrhea after 3 days of therapy. Comments: Antibiotic treatment as in acute otitis media if there is acute exacerbation. Appropriate antibiotic use for acute respiratory tract infection in adults: advice for high-value care from the American College of Physicians and the Centers for Disease Control and Prevention. Systemic antibiotics versus topical treatments for chronically discharging ears with underlying eardrum perforations. Aerosolized ribavirin is not available in the Philippines A: Antibiotics are not indicated. The mainstay of therapy is supportive care, which includes hydration, measurement of oxygen saturation and use of supplemental oxygen if needed. Ribavirin is not routinely recommended due to the high cost, toxicity, absence of controlled data. Palivizumab is a humanized mouse monoclonal antibody for the prevention of bronchiolitis, reducing hospitalization rates by 39-82% among high risk infants. If Mycoplasma is documented, prefer doxycycline over macrolides due to increasing macrolide resistance. A throat swab polymerase chain reaction test may be done to diagnose Mycoplasma or Chlamydophila (formerly Chlamydia). Peritonsillar abscess (Quinsy) Persistent cough (>14 days), afebrile during community outbreak: Pertussis (whooping cough) · Presents as 3 stages: 1) catarrhal (1-2 weeks); 2) paroxysmal coughing (2-4 weeks); and 3) convalescence (1-2 weeks). In the non-outbreak setting, the likelihood of pertussis increased if post-tussive emesis or inspiratory whoop is present. Etiology: Viruses in 20%-50%, Chlamydophila pneumonia in 5%, Mycoplasma pneumonia in <1% the role of S. Influenza · Fever, cough, myalgia during influenza season · Complications include influenza pneumonia and secondary bacterial pneumonia due to community-acquired methicillin-resistant and susceptible Staphylococcus aureus, Streptococcus pneumoniae, and Haemophilus influenzae. Allergic bronchopulmonary aspergillosis (clinical manifestation: wheezing, pulmonary infiltrates, bronchiectasis, and fibrosis). Airway colonization is associated with increase blood eosinophils, increase lgE levels and isolation of Aspergillus spp. Comments: Itraconazole decreases the number of exacerbations requiring corticosteroids with improved immunological markers improved lung function and exercise tolerance. Acute asthma attacks associated with allergic bronchopulmonary aspergillosis is treated with corticosteroids. Available Co-amoxiclav preparations in the formulary are the following: 4:1 500 mg amoxicillin (as trihydrate) + 125 mg potassium clavulanate per tablet 7:1 875 mg amoxicillin (as trihydrate) + 125 mg potassium clavulanate per tablet 200 mg amoxicillin (as trihydrate) + 28. Free from pulmonary/ extrapulmonary complications Although the total course of therapy is usually 7 to 10 days for uncomplicated pneumonia, longer courses of 2 to 3 weeks may be required for more severe disease (pleural empyema or pulmonary abscesses). Complaints are related to slowly progressive systemic symptoms over 3 to 7 days, with malaise, pharyngitis, and headache, followed by cough that is irritative and nonproductive (lasting for 2-4 weeks). Physical examination may show rales, rhonchi, and wheezes in the context of a child who does not appear ill ("walking pneumonia"). It is recommended that they be reserved as potential second-line agents for the treatment of pulmonary tuberculosis, particularly for multi-drug resistant tuberculosis. Comments: For those at risk of aspiration, infections with anaerobes should be considered. Because of increasing resistance of gram (-) bacilli to fluoroquinolones, monotherapy with fluoroquinolone is not recommended. Choose antibiotics based on available micro- biological data, or use an oral agent from the same drug class. History of chronic or prolonged (>7 days within the past month) use of broadspectrum antibiotic therapy. Treatment should be modified according to culture/sensitivity results once available. Comments: Do surgical intervention if with failure to improve after 7d of appropriate antibiotics. The recommendations for empiric therapy here are based on national antimicrobial resistance data. Immunosuppressive disease and/ or therapy Etiology: Viral and fungal pathogens in immunocompromised hosts (patients on chronic immunosuppressants, solid organ and bone marrow transplant recipients) Comments: Refer to a specialist. Antibiotic therapy should be de- escalated or modified based on the culture and susceptibility results. Do not use adjunctive rifampicin in patients caused by Acinetobacter species that is sensitive only to colistin. Management of Adults with Hospital-acquired and Ventilator associated Pneumonia; 2016 Clinical Practice Guideline by the Infectious Diseases Society of American Thoracic Society. Task Force: Diagnosis, Empiric Management and Prevention of Community-Acquired Pneumonia in Immunocompetent Adults 2016 Update. Antibiotic therapy is recommended for abscesses with the following conditions: severe or extensive disease. If no response after 2-3 days with oral antibiotics, look for complications and consider: Incision and drainage: culture abscess and blood. Systemic agents should be used in patients who are toxic, who have extensive disease, or who have associated cellulitis. Preferred Regimen: Treat as for furuncles and boils For decolonization: If patient and physician wish to attempt decolonization. Only a modest positive effect in a prospective, randomized single-blinded controlled trial. Topical decolonization is considered if patient has 2 or more episodes in 1 year or other household members develop infection. Intermittent bathing with chlorhexidine 4% or dilute bleach baths/6% sodium hypochlorite (1/4 cup of bleach in a quarter-filled bathtub or 13 gallons water or 1 tsp bleach in 1 gallon of water) for 15 minutes 3x a week can be used to significantly reduce skin load of S. Systemic therapy in cases of large and multiple lesions should be treated with Penicillinase resistant antibiotics (Cloxacillin or cephalexin). Staphylococcal scalded skin syndrome Etiology: Result of colonization of skin or mucosa by strain of S. Topicals can be used for patients with limited number of lesions and appropriate for those with mild, localized areas of impetigo, no more than 3 areas of impetigo or an area of infection <5 cm. Oral antibiotics are indicated for patients with more extensive areas of infection (those with multiple lesions) if infection is not resolving or is worsening, or those with systemic symptoms; and those with non-bullous impetigo in multiple family members, child care groups, or athletic teams. Impetigo begins as erythematous papules that rapidly evolve into vesicles and pustules that rupture, with the dried discharge forming honeycolored crusts on an erythematous base. Lesions begin as vesicles that rupture, resulting in circular, erythematous ulcers with adherent crusts, often with surrounding erythematous edema. Streptococcus pyogenes infection manifests as "honey crust" lesions or "punched out" ulcers (ecthyma). Gram stain and culture of the pus or exudates from skin lesions of impetigo and ecthyma are recommended to help identify whether S. Oral therapy for ecthyma and impetigo should be a 7-day regimen with an agent active against S. It is an elevated erythematous lesion, sometimes exhibiting blebs filled with yellowish fluid, which may crust over after rupture. Usually, can clinically distinguish between red indurated demarcated inflamed skin of erysipelas (S. Sudden onset of rapidly spreading red edematous tender plaquelike skin on the face in an otherwise healthy host. Cellulitis (non-purulent) Etiology: Usually caused by beta-hemolytic streptococci. Acinetobacter are also found more often in patients with more severe burns and comorbidities. Any evidence of deep infection, especially if it persists or develops more than 72h after injury and particularly in children, is a strong indication for exploration and addition of an anti-pseudomonal agent. Wound infection, post-trauma Etiology: Polymicrobic (microbial flora dependent on nature of the trauma): S. Ciprofloxacin has been used most extensively in children and adolescents and appears to be well tolerated, effective and does not appear to cause arthropathy. Antimicrobial therapy is recommended for deep incisional surgical site infections if systemic signs of sepsis are present, if source control is incomplete or in immunocompromised patients.
Unlabeled or improperly labeled specimen Non-sterile or leaking container Inappropriate specimen transport conditions Illegible androgen hormone questionnaire discount 250mg eulexin with amex, or no submitter information on the request form Mismatched form and specimen Broken specimen/sample container the wrong specimen for test request Inappropriate outfit for requested test Illegible or no patient information on the specimen Expired transport media 24 hours/day androgen hormone joint buy 250mg eulexin fast delivery, 7days/week Brucella species isolated/detected Brucella species not found Call 410-925-3121 before sending specimen to the Laboratory mens health zac efron photoshop 250 mg eulexin otc. Abscesses mens health raspberry ketone buy eulexin 250mg low cost, tissue aspirates prostate psa 05 eulexin 250mg mastercard,body fluids: Collect tissues and fluids rather than swabs man health daily shopping category buy discount eulexin 250 mg on-line, when possible. Continued Next Page> Burkholderia mallei and Burkholderia pseudomallei Guide to Public Health Laboratory Services December 2016 edition v2. Mehsen Joseph Public Health Laboratory Specimen Volume (Optimum): Specimen Volume (Minimum): Collect: 1. Form: Packaging and Shipping*: Blood: Collect appropriate blood volume and number of sets as per routine laboratory protocol. Abscesses, tissues aspirates, body fluids: Collect tissues and body fluids rather than swabs. Urine: Transport in a sterile, well sealed container chilled using wet ice or cold packs. Abscesses, tissues, and fluids: Transport the specimen at room temperature for immediate processing. Unlabeled or improperly labeled specimen Non-sterile or leaking container Inappropriate specimen transport conditions Illegible, or no submitter information on the request form Mismatched form and specimen Broken specimen/sample container the wrong specimen for test request Inappropriate outfit for requested test Illegible or no patient information on the specimen Expired transport media 24 hours/day, 7 days/week B. Unpreserved, shipped in insulated container with freezer pack the following rejection criteria are designed to prevent the reporting of inaccurate results and to avoid misleading information that might lead to misdiagnosis and inappropriate therapy. The Clostridium difficile toxin test is used to diagnose antibiotic-associated diarrhea and pseudomembranous colitis that is caused by C. Positive: Presence of detectable IgM antibody, presumptive infection with Chikungunya virus. A positive IgM result may not indicate a recent infection because IgM may persist for several months after infection. Mehsen Joseph Public Health Laboratory Purpose of Test: Method: Interfering Substances: Testing Site: Comment: For the presumptive detection of IgM antibody to Chikungunya Virus. Specimen Volume (Optimum): Specimen Volume (Minimum): Collect: Form: Packaging and Shipping*: Transport Conditions: Specimen Rejection Criteria: Availability: Results and Interpretation: Additional Information: Purpose of Test: Method: Interfering Substances/Limitations: Testing Site: Comment: Guide to Public Health Laboratory Services December 2016 edition v2. This test is limited to medico-legal specimens: cervical, rectal, male urethral; and noncervical, non-rectal, and non-male urethral specimens. Diagnostic, qualitative detection of Chlamydia Cell culture A negative result does not exclude the possibility of infection. Transport Conditions: Specimen Rejection Criteria: Availability: Results and Interpretation: Additional Information: Purpose of Test: Method: Interfering Substances: Testing Site: Comment: Ambient temperature for specimens on the blood clot, separated serum at 2-8°C (refrigerated) or -20°C (frozen). Hemolysis; insufficient volume, specimen collected > 5 days prior to arrival without being frozen. Does not rule out recent exposure and collection of sample prior to development of IgG antibodies. Swab: Tube, Prefilled with 2 ml of diluent Urine: Optimal quality specimen is 20-60 ml of "first of the void" urine collected in a plastic collection cup. Swab: Tube, Prefilled with 2 ml of diluent Urine: Collect a minimum of 4ml (20-60 best) in a plastic collection cup. The patient should not have urinated for at least 1 hour prior to specimen collection. Only cell culture isolation should be used when testing for the evaluation of suggested sexual abuse or other medico-legal purposes. Botulism Office of Laboratory Emergency Preparedness and Response: 410-925-3121 (24/7 emergency contact number) Select Agents Microbiology Laboratory: 443-681-3954 Division of Microbiology Laboratory: 443-681-3952 3-7 days [from specimen receipt in the Laboratory] Continued Next Page> Turnaround Time: Guide to Public Health Laboratory Services December 2016 edition v2. Mehsen Joseph Public Health Laboratory Specimen Required: Specimen Identification: Specimen Volume (Optimum): Specimen Volume (Minimum): Collect: Form: Packaging and Shipping*: Suspected foodborne botulism cases: Suitable specimens for examination are: serum, feces, vomitus, gastric contents. Suspected wound botulism cases: Suitable specimens for examination are: serum, tissue, feces. Transport Conditions: Specimen Rejection Criteria: Availability: Results and Interpretation: Additional Information: Purpose of Test: Method: Interfering Substances: Serum: Transport to the Laboratory on wet ice or cold packs. If an unavoidable delay of several days is anticipated, the specimen should be kept frozen and then packed in an insulated container with dry ice and proper cushioning material for shipment. Unlabeled or improperly labeled specimen Non-sterile or leaking container Inappropriate specimen transport conditions Illegible, or no submitter information on the request form Mismatched form and specimen Broken specimen/sample container the wrong specimen for test request Inappropriate outfit for requested test Illegible or no patient information on the specimen Expired transport media 24 hours/day, 7 days/week Clostridium botulinum toxin detected/not detected. Must have consent of the State Epidemiologist before sending specimen to the Laboratory (410-767-6685). Botulism Office of Laboratory Emergency Preparedness and Response: 410-925-3121 (24/7 emergency contact number) Select Agents Microbiology Laboratory: 443-681-3954 Division of Microbiology Laboratory: 443-681-3952 Continued Next Page> Guide to Public Health Laboratory Services December 2016 edition v2. Mehsen Joseph Public Health Laboratory Turnaround Time: Specimen Required: Specimen Identification: Specimen Volume (Optimum): Specimen Volume (Minimum): Collect: Form: Packaging and Shipping*: 3-30 days [from specimen receipt in the Laboratory] Suspected infant botulism cases: Suitable specimens: Stool, rectal swabs (not necessary to collect serum. Stool: 10-50 grams (English walnut size) N/A Stool: Collect in a sterile, well-sealed, unbreakable container. Enema (if needed): Use minimal amount of sterile water or non-bacteriostatic water, place 20 ml of liquid into a sterile, well-sealed, unbreakable container. Transport Conditions: Specimen Rejection Criteria: Availability: Results and Interpretation: Additional Information: Purpose of Test: Method: Interfering Substances: Stool: Transport to the Laboratory on wet ice or cold packs. If the patient has been taking any medication that might interfere with toxin assays or culturing of the stool, the Laboratory should be notified. For example, it has been demonstrated that anticholinesterase drugs given orally to patients for myasthenia gravis can interfere with mouse botulinum toxin assays of stool extracts. Transport Conditions: Specimen Rejection Criteria: Availability: Results and Interpretation: Ambient temperature for specimens on the blood clot (whole blood specimens transported on ice packs are acceptable), separated serum at 2-8°C (refrigerated) or 20°C (frozen). A 4-fold IgG antibody endpoint titer increase is considered supportive evidence of current or recent acute infection. Specimens obtained too early in the infection may not contain detectable antibody levels. Additional Information: Purpose of Test: Methods: Interfering Substances: Testing Site: Comment: Guide to Public Health Laboratory Services December 2016 edition v2. If status of patient suggest a cryptococcal infection, subsequent specimens and culture strongly recommended. Transport Conditions: Ambient temperature for specimens on the blood clot (whole blood specimens transported on ice packs are acceptable), separated serum at 2-8°C (refrigerated) or 20°C (frozen). Continued Next Page> - Guide to Public Health Laboratory Services December 2016 edition v2. If shipping is delayed beyond 48 hours, specimen can be frozen at -20°C and shipped on dry ice. Monday-Friday Negative: No detectable IgM antibody, the result does not rule out Dengue virus infection. An additional sample should be tested within 7-14 days if early infection is suspected. Positive: Presence of detectable IgM antibody, presumptive infection with Dengue virus. Mehsen Joseph Public Health Laboratory Additional Information: Purpose of Test: Method: Interfering Substances: Testing Site: Comment: the term "Arbovirus" has no taxonomic significance, but is a shortened name give to viruses that are transmitted by blood feeding arthropods (mosquitoes, ticks, etc). N/A N/A Swab infected areas thoroughly, getting swab well into membranes or other lesions present. Transport Conditions: Specimen Rejection Criteria: Room temperature Availability: Results and Interpretation: Reference Range: Additional Information: Purpose of Test: Method: Guide to Public Health Laboratory Services December 2016 edition v2. Unlabeled or improperly labeled specimen Non-sterile or leaking container Inappropriate specimen transport conditions Illegible, or no submitter information on the request form Mismatched form and specimen Broken specimen/sample container the wrong specimen for test request Inappropriate outfit for requested test Illegible or no patient information on the specimen Expired transport media Monday through Friday Definitive identification of Corynebacterium diptheriae. Diagnosis of toxigenic strains of Corynebacterium diptheriae and antibiotic treatment are essential in limiting spread of infection. Microbiology-Enterics, 443-681-4570 4 10 days [from specimen receipt in the Laboratory] Pure isolate of E. Unlabeled or improperly labeled specimen Non-sterile or leaking container Inappropriate specimen transport conditions Illegible, or no submitter information on the request form Mismatched form and specimen Broken specimen/sample container the wrong specimen for test request Inappropriate outfit for requested test Illegible or no patient information on the specimen Expired transport media Monday through Friday E. Specimens must be packaged in a triple packaging system to ensure that under normal conditions of transport they cannot break, be punctured or leak their contents (Refer to pages 9 & 10 for triple packing guidance). Microbiology - Enterics 443-681-4570 Usually four (4) days to several weeks [from specimen receipt in the Laboratory]. Stool in stool culture transport media (Para Pak for Enteric pathogens [orange cap]). Fresh stool in Para Pak for enteric pathogens (Cary-Blair transport media), select portion of stool containing pus, blood or mucous; rectal swab inserted one (1) inch beyond anal sphincter, rotate carefully, withdraw and place in Cary-Blair transport medium. Transport Conditions: Orange top Para-Pak Transport Media: store and ship refrigerated (2-8°C) temperature. Mehsen Joseph Public Health Laboratory Specimen Rejection Criteria: Availability: Results and Interpretation: Reference Range: Additional Information: Purpose of Test: Method: Interfering Substances/Limitations: Testing Site: Comment: the following rejection criteria are designed to prevent the reporting of inaccurate results and to avoid misleading information that might lead to misdiagnosis and inappropriate therapy. Unlabeled or improperly labeled specimen Non-sterile or leaking container Inappropriate specimen transport conditions Illegible, or no submitter information on the request form Mismatched form and specimen Broken specimen/sample container the wrong specimen for test request Inappropriate outfit for requested test Illegible or no patient information on the specimen Expired transport media Specimen received after prolonged delay (usually more than 96 hours) Dry specimen Specimen contaminated with urine or water Stool containing barium Insufficient quantity Specimen frozen Monday through Friday Identification of pathogenic enteric organisms and determination of antimicrobial susceptibilities, if clinically appropriate. Normal stool flora Enteric culture screens routinely for Salmonella, Shigella, Campylobacter, and Shiga toxin producing E. Yersinia culture and Vibrio culture must be specifically indicated as they are not part of routine testing. Collect specimens early in the course of enteric disease and prior to antimicrobial therapy. Collect 2 or 3 stools on separate days to increase the likelihood of isolating enteric pathogens. Isolation, identification and if clinically appropriate, antimicrobial susceptibilities of potentially pathogenic organisms. Transport Conditions: Specimen Rejection Criteria: Availability: Results and Interpretation: Additional Information: Purpose of Test: Method: Interfering Substances: Testing Site: Comment: Ambient temperature for specimens on the blood clot (whole blood specimens transported on ice packs are acceptable), separated serum at 2-8°C (refrigerated) or 20°C (frozen). Transport Conditions: Specimen Rejection Criteria: Availability: Results and Interpretation: Reference Range: Ship on wet ice the following rejection criteria are designed to prevent the reporting of inaccurate results and to avoid misleading information that might lead to misdiagnosis and inappropriate therapy. Unlabeled or improperly labeled specimen Non-sterile or leaking container Inappropriate specimen transport conditions Illegible, or no submitter information on the request form Mismatched form and specimen Broken specimen/sample container the wrong specimen for test request Inappropriate outfit for requested test Illegible or no patient information on the specimen Expired transport media Stool in preservative Specimen received after prolonged delay (usually more than 72 hours) Monday through Friday Staph. Mehsen Joseph Public Health Laboratory Additional Information: Purpose of Test: Method: Interfering Substances: Testing Site: Comment: Bacillus cereus: the symptoms of B. The onset of watery diarrhea, abdominal cramps, and pain occurs 6-15 hours after consumption of contaminated food. The emetic type of food poisoning is characterized by nausea and vomiting within 0. The illness is usually over within 24 hours but less severe symptoms may persist in some individuals for 1 or 2 weeks. The most common symptoms are nausea, vomiting, retching, abdominal cramping, and prostration. Some individuals may not always demonstrate all the symptoms associated with the illness. In more severe cases, headache, muscle cramping, and transient changes in blood pressure and pulse rate may occur. Recovery generally takes two (2) days; however, it is not unusual for complete recovery to take three (3) days and sometimes longer in severe cases. Culture, isolation and identification of Bacillus cereus, Clostridium perfringens or Staph aureus. Colony count performed on specimens for Bacillus cereus and Clostridium perfringens. Continued Next Page> Page 56 of 128 Guide to Public Health Laboratory Services December 2016 edition v2. Mehsen Joseph Public Health Laboratory Specimen Volume (Optimum): Specimen Volume (Minimum): Collect: Form: Packaging and Shipping*: N/A N/A 1. Blood Culture: Collect appropriate blood volume and number of sets per routine laboratory protocol. For small amount tissue samples, add several drops of sterile normal saline to keep the tissue moist. Isolates: Transport the specimen at room temperature on a sealed chocolate agar plate or slant. Unlabeled or improperly labeled specimen Non-sterile or leaking container Inappropriate specimen transport conditions Illegible, or no submitter information on the request form Mismatched form and specimen Broken specimen/sample container the wrong specimen for test request Inappropriate outfit for requested test Illegible or no patient information on the specimen Expired transport media 24 hrs/day, 7 days/week Francisella tularensis isolated/detected. Required supplemental information: Please include submitting agency, contact name, address, phone number, specimen identifier, patient name, specimen source and type, sex and date of birth, symptoms of onset, sample collection date, and clinical information including type and date of treatment patient has received. Roll swab directly on the medium in a large "Z" (1a) (to provide adequate exposure of the swab to the medium for transfer of organisms. Cut off the corner of one foil-wrapped tablet to expose the tablet and place it in the bag. If an incubator is available, incubate the plates in an inverted (medium facing down) position at 35°C until picked up by courier. If an incubator is not available, invert the plates and hold them at room temperature until picked up by the courier. When packing plates for transport, keep them inverted and place in a suitable container that will protect them from extreme heat or cold. Unlabeled or improperly labeled specimen Non-sterile or leaking container Inappropriate specimen transport conditions Illegible, or no submitter information on the request form Mismatched form and specimen Broken specimen/sample container the wrong specimen for test request Inappropriate outfit for requested test Illegible or no patient information on the specimen Expired transport media Monday through Friday Neisseria gonorrhea isolated and identified. No Neisseria gonorrhea isolated Continued Next Page> Guide to Public Health Laboratory Services December 2016 edition v2. Mehsen Joseph Public Health Laboratory Additional Information: Purpose of Test: Method: Interfering Substances: Testing Site: Comment: Store unused plates under refrigeration upside down (media facing down). Discard any plate(s) with an expired expiration date or that exhibit growth prior to use (never use contaminated plates). Always allow plates to warm to room temperature before using (cold kills Neisseria gonorrhea). Do not incubate inoculated plates in the clinic longer than 24 hours (over-incubation leads to more growth of contaminating normal flora). If an incubator is not available, invert the inoculated plates and hold them at room temperature until picked up by the courier. Isolation, identification and antibiotic susceptibility testing for Neisseria gonorrhea.
InfectionwithS mansoniandotherspecies(exceptS haematobium)isdeterminedby microscopicexaminationof stoolspecimenstodetectcharacteristiceggs androgen insensitivity syndrome hormone therapy order eulexin 250 mg line,butresultsmay benegativeif performedtooearlyinthecourseof infection mens health zyzz eulexin 250mg with mastercard. Serologictests prostate cancer 10 year survival buy eulexin 250 mg cheap,availablethroughtheCentersforDisease ControlandPreventionandsomecommerciallaboratories mens health hairstyles 250 mg eulexin otc,candetectschistosomeinfection;additionaltestscandistinguishbetweeninfectionwithS mansoni prostate cancer zytiga buy 250mg eulexin with amex, S haematobium mens health zimbabwe discount eulexin 250 mg visa, or S japonicum. Thus,massorselectivetreatmentof infectedpopulations,sanitarydisposal of humanwaste,andeducationaboutthesourceof infectionarekeyelementsof current controlmeasures. AmongShigellaisolatesreportedinindustrializednationsincludingtheUnitedStatesin 2009,approximately86%wereShigella sonnei,12%wereShigella flexneri, 1%wereShigella boydii,andlessthan1%wereS dysenteriae( Otherimportantcontrolmeasuresincludeimprovedsanitation,asafewatersupply throughchlorination,propercookingandstorageof food,theexclusionof infected peopleasfoodhandlers,andmeasurestodecreasecontaminationof foodandsurfaces byhouseflies. Becausevaricella eruptsincropsof lesionsthatevolvequickly,lesionsonanyonepartof thebodywillbe indifferentstagesof evolution(papules,vesicles,andcrusts),whereasallsmallpoxlesions onanyonepartof thebodyareinthesamestageof development. Inadditiontothetypicalpresentationof smallpox(90%of casesorgreater),there are2uncommonformsof variolamajor:hemorrhagic(characterizedeitherbyahemorrhagicdiathesispriortoonsetof thetypicalsmallpoxrash[earlyhemorrhagicsmallpox] orbyhemorrhageintoskinlesionsanddisseminatedintravascularcoagulation[latehemorrhagicsmallpox])andmalignantorflattype(inwhichtheskinlesionsdonotprogress tothepustularstagebutremainflatandsoft). Theshortincubationperiod,brevityof illness,andusuallackof fever helpdistinguishstaphylococcalfromothertypesof foodpoisoningexceptthatcaused byBacillus cereus. Identification(bypulsed-fieldgelelectrophoresis orphagetyping)of thesametypeof S aureusfromstoolorvomitusof 2ormoreillpeople,fromstoolorvomitusof anillpersonandanimplicatedfood,orstoolorvomitusof anillpersonandapersonwhohandledthefoodalsoconfirmsthediagnosis. Staphylococcus aureus Toxic Shock Syndrome: Clinical Case Definitiona Clinical Findings · Fever:temperature38. Centralnervoussystem:disorientationoralterationsinconsciousnesswithoutfocalneurologicsignswhenfeverandhypotensionareabsent Laboratory Criteria · Negativeresultsonthefollowingtests,if obtained: Blood,throat,orcerebrospinalfluidcultures;bloodculturemaybepositiveforS aureus SerologictestsforRockyMountainspottedfever,leptospirosis,ormeasles Case Classification · Probable:acasethatmeetsthelaboratorycriteriaandinwhich4of 5clinicalfindings arepresent · Confirmed:acasethatmeetslaboratorycriteriaandall5of theclinicalfindings,including desquamation,unlessthepatientdiesbeforedesquamationoccurs. Additionalriskfactorsforhealth care-associatedacquisitionof S aureusincludeillnessrequiringcareinneonatalorpediatricintensivecareorburnunits;surgicalprocedures;prolongedhospitalization;localepidemicof S aureusinfection;andthepresenceof indwellingcathetersorprostheticdevices. Apatient whohasanonseriousallergytopenicillincanbetreatedwithafirst-orsecond-generation cephalosporin,andif thepatientisnotalsoallergictocephalosporins,withvancomycin orwithclindamycin,if endocarditisorcentralnervoussysteminfectionisnotaconsiderationandtheS aureusstrainissusceptible. S aureus and "D" test-negative I c Consider prevalence of clindamycin-susceptible methicillin-susceptible b community-associated methicillin-resistant S aureus strains in the community. T c onsiderprevalenceofclindamycin-susceptiblemethicillin-susceptibleS aureusand"D"test-negative C community-associatedmethicillin-resistantS aureusstrainsinthecommunity. Parenteral Antimicrobial Agent(s) for Treatment of Bacteremia and Other Serious Staphylococcus aureus Infections Susceptibility Antimicrobial Agents Comments I. Healthcare-associated(multidrugresistant) Drugsof choice: Vancomycin+gentamicina A lternatives:susceptibilitytestingresults availablebeforealternativedrugsareused Trimethoprim-sulfamethoxazole Linezolidb Quinupristin-dalfopristinb Fluoroquinolones Notrecommendedforpeopleyoungerthan18yearsof ageorasmonotherapy (seeFluoroquinolones,p800) Table 3. Parenteral Antimicrobial Agent(s) for Treatment of Bacteremia and Other Serious Staphylococcus aureus Infections, continued Comments Forlife-threateninginfections Forpneumonia,septicarthritis,osteomyelitis,skinorsofttissueinfections Forskinorsofttissueinfections Susceptibility Antimicrobial Agents B. If bloodcultures remainpositiveforstaphylococciformorethan3to5daysorif theclinicalillnessfailsto improve,thecentrallineshouldberemoved,parenteraltherapyshouldbecontinued,and thepatientshouldbeevaluatedformetastaticfociof infection. Prophylacticadministrationof anantimicrobialagentintraoperativelylowerstheincidenceof infectionafter cardiacsurgeryandimplantationof syntheticvasculargraftsandprostheticdevicesand oftenhasbeenusedatthetimeof cerebrospinalfluidshuntplacement. Measurestopreventhealthcare-associatedS aureus infectionsinindividualpatients includestrictadherencetorecommendedinfection-controlprecautionsandappropriate intraoperativeantimicrobialprophylaxis,andinsomecircumstances,useof antimicrobial regimenstoattempttoeradicatenasalcarriageincertainpatientscanbeconsidered. Carefulpreparationof theskinbeforesurgery,includingcleansingof skinbefore placementof intravascularcathetersusingbarriermethods,willdecreasetheincidence of S aureus woundandcatheterinfections. Useof intermittentorcontinuousintranasalmupirocinforeradicationof nasalcarriagealsohasbeenshowntodecreasetheincidenceof invasiveS aureus infectionsinadultpatientsundergoinglong-termhemodialysisorambulatoryperitoneal dialysis. Theseincludegeneral recommendationsforallsettingsandfocusonadministrativeissues;engagement,education,andtrainingof personnel;judicioususeof antimicrobialagents;monitoring of prevalencetrendsovertime;useof standardprecautionsforallpatients;anduseof contactprecautionswhenappropriate. Othermeasures recommendedduringoutbreaksincludereinforcementof handhygiene,alleviating overcrowdingandunderstaffing,colonizationsurveillanceculturesof newborninfants atadmissionandperiodicallythereafter,useof contactprecautionsforcolonizedor infectedinfants,andcohortingof colonizedorinfectedinfantsandtheircaregivers. Twoormoreof thefollowingsigns: · Renalimpairment:creatinineconcentration177mol/L(2mg/dL)orgreaterfor adultsoratleast2timestheupperlimitof normalforage · Coagulopathy:plateletcount100000/mm3orlessordisseminatedintravascular c oagulation · Hepaticinvolvement:elevatedalaninetransaminase,aspartatetransaminase,ortotal bilirubinconcentrationsatleast2timestheupperlimitof normalforage · Adultrespiratorydistresssyndrome · Ageneralizederythematousmacularrashthatmaydesquamate · Softtissuenecrosis,includingnecrotizingfasciitisormyositis,organgrene AdaptedfromTheWorkingGrouponSevereStreptococcalInfections. Aswiththroatswabcultures,sensitivityof thesetestsishighlydependentonthequalityof thethroatswabspecimen,the experienceof thepersonperformingthetest,andtherigorof theculturemethodused forcomparison. Anumberof antimicrobialagents,includingclindamycin,cephalosporins, amoxicillin-clavulanate,azithromycin,andacombinationof rifampinforthelast4days of treatmentwitheitherpenicillinVorpenicillinGbenzathinehavebeendemonstrated tobemoreeffectivethanpenicillinineliminatingchronicstreptococcalcarriage. Management of Streptococcal Toxic Shock Syndrome Without Necrotizing Fasciitis · Fluidmanagementtomaintainadequatevenousreturnandcardiacfillingpressuresto preventend-organdamage · Anticipatorymanagementof multisystemorganfailure · Parenteralantimicrobialtherapyatmaximumdoseswiththecapacityto: Killorganismwithbactericidalcellwallinhibitor(eg,beta-lactamaseresistant antimicrobialagent) Decreaseenzyme,toxin,orcytokineproductionwithproteinsynthesisinhibitor (eg,clindamycin) · ImmuneGlobulinIntravenousmaybeconsideredforinfectionrefractorytoseveralhours of aggressivetherapyorinthepresenceof anundrainablefocusorpersistentoliguriawith pulmonaryedema Table 3. Management of Streptococcal Toxic Shock Syndrome With Necrotizing Fasciitis · PrinciplesoutlinedinTable3. Early-onsetdisease usuallyoccurswithinthefirst24hoursof life(range,06days)andischaracterizedby signsof systemicinfection,respiratorydistress,apnea,shock,pneumonia,andlessoften, meningitis(5%10%of cases). The anginosusgroup(S anginosus,Streptococcus constellatus, andStreptococcus intermedius)canhave variablehemolysis,andapproximatelyonethirdpossessgroupA,C,F,orGantigens. Althoughmostvancomycin-resistantisolatesof E faecalisandE faeciumaredaptomycinsusceptible,daptomycin isapprovedforuseonlyinadultsfortreatmentof infectionsattributabletovancomycinresistantE faecalis. Forthesepatients,earlyinstruction inproperdiet;oralhealth,includinguseof dentalsealantsandadequatefluorideintake; andpreventionorcessationof smokingwillaidinpreventionof dentalcarriesandpotentiallylowertheirriskof recurrentendocarditis. Someconsequencesof intrauterine infectionmaynotbecomeapparentuntilmanyyearsafterbirth,suchasinterstitialkeratitis(520yearsof age),eighthcranialnervedeafness(1040yearsof age),Hutchinson teeth(peg-shaped,notchedcentralincisors),anteriorbowingof theshins,frontalbossing,mulberrymolars,saddlenose,rhagades(perioralfissures),andCluttonjoints(symmetric,painlessswellingof theknees). Algorithm for evaluation and treatment of infants born to mothers with reactive serologic tests for syphilis. Infantswhohaveanormalphysicalexaminationandaserumquantitativenontreponemalserologictitereitherthesameasorlessthanfourfold(eg,1:4isfourfoldlower than1:16)thematernaltiterareatminimalriskof syphilisif (1)theyareborntomotherswhocompletedappropriatepenicillintreatmentforsyphilisduringpregnancyand morethan4weeksbeforedelivery;and(2)themotherhadnoevidenceof reinfectionor relapse. Childrenyoungerthan8yearsof ageshouldnotbegiven t etracyclineordoxycyclineunlessthebenefitsof therapyaregreaterthantherisksof d entalstaining(seeTetracyclines,p801). Nontreponemalantibodytitersshoulddecreaseby3monthsof ageandshouldbe nonreactiveby6monthsof ageif theinfantwasinfectedandadequatelytreatedorwas notinfectedandinitiallyseropositivebecauseof transplacentallyacquiredmaternalantibody. Because moistopenlesions,secretions,andpossiblybloodarecontagiousinallpatientswith syphilis,glovesshouldbewornwhencaringforpatientswithcongenital,primary,and s econdarysyphiliswithskinandmucousmembranelesionsuntil24hoursof treatment hasbeencompleted. Other Tapeworm Infections (Including Hydatid Disease) Mostinfectionsareasymptomatic,butnausea,abdominalpain,anddiarrheahavebeen observedinpeoplewhoareheavilyinfected. People19yearsof ageand olderwhorequireatetanustoxoid-containingvaccineaspartof woundmanagement shouldreceiveTdapinsteadof Tdif theypreviouslyhavenotreceivedTdap. Otherrecommendationsfortetanusimmunization,includingrecommendationsfor olderchildren,areasfollows: · Forcatch-upimmunizationforchildren7through10yearsof age,Tdapvaccine shouldbesubstitutedforasingledoseof Tdinthecatch-upseries(seeFig1. Forpreventionof neonataltetanus,preventivemeasures(inadditiontomaternal immunization)includecommunityimmunizationprogramsforadolescentgirlsand womenof childbearingageandappropriatetrainingof midwivesinrecommendations forimmunizationandsteriletechnique. Microsporum canis, Microsporum audouinii, Trichophyton violaceum, andTrichophyton mentagrophytesarelesscommon. Afrequent sourceof confusionisanalterationintheappearanceof lesionsasaresultof application of atopicalcorticosteroidpreparation,termedtineaincognito. Recurrenceispreventedbyproperfoothygiene,whichincludeskeepingthefeet dryandcool,gentlecleaning,dryingbetweenthetoes,useof absorbentantifungalfoot powder,frequentairingof affectedareas,andavoidanceof occlusivefootwearandnylon socksorotherfabricsthatinterferewithdissipationof moisture. Theclassicaltriadof cerebral alcifications,chorioretinitis,andhydrocephalusisrarebutitishighlysuggestive c of congenitaltoxoplasmosis,anditisseenprimarilyinbabieswhosemotherswerenot treatedfortoxoplasmosisduringgestation. Theseroprevalenceof T gondiiinfection(areflectionof thechronic infectionandmeasuredbythepresenceof T gondii-specificIgGantibodies)variesby geographiclocaleandthesocioeconomicstrataof thepopulation. However,thepresenceof low-avidity antibodiesisnotareliableindicationof recentinfection,andtreatmentmayaffectthe maturationof IgGavidityandprolongthepresenceof low-avidityantibodies. Serialfetalultrasonographicexaminationscanbeperformedincasesof suspectedcongenitalinfectionto detectanyincreaseinsizeof thelateralventriclesof thecentralnervoussystemorother signsof fetalinfection,suchasbrain,hepatic,orspleniccalcifications. Oralingestionof viableT gondiicanbeavoidedby:(1)avoidingconsumptionof raw orundercookedmeatandcookingmeat articularlypork,lamb,andvenison oan -p -t internaltemperatureof 65. Commercialandhome-raisedpork remainasourceof humaninfections,butmeatsotherthanpork,suchas enison,horse v meat,andparticularlymeatsfromwildcarnivorousoromnivorousgame(bear,boar,seal, andwalrus)nowarecommonsourcesof infection. WithTrypanosoma brucei gambiense(WestAfrican) infection,acutaneousnoduleorchancremayappearatthesiteof parasiteinoculation withinafewdaysof abitebyaninfectedtsetsefly. Bothformsof Africantrypanosomiasishavehighfatalityrates;withouttreatment,infectedpatientsusuallydiewithinweeksto monthsafterclinicalonsetof diseasecausedbyT brucei rhodesienseandwithinafewyears fromdiseasecausedbyT brucei gambiense. Theincubation periodforT brucei rhodesienseinfectionis3to21daysandusually is5to14days;forT brucei gambienseinfection,theincubationperiodusuallyislongerbut isnotwelldefined. ConcentrationandGiemsastainingof thebuffycoat layerof peripheralbloodalsocanbehelpfulandiseasierforT brucei rhodesiense,because thedensityof organismsinbloodcirculatingishigherthanforT brucei gambiense. M boviscanbedistinguishedroutinelyfrom M tuberculosis,andalthoughthespectrumof illnessthatiscausedbyM bovisissimilar tothatof M tuberculosis,theepidemiology,treatment,andpreventionaredistinct. Chestradiographicfindingsafternfection i rangefromnormaltodiverseabnormalities,suchaslymphadenopathyof thehilar, subcarinal,paratracheal,ormediastinalnodes;atelectasisorinfiltrateof asegmentor lobe;pleuraleffusion;cavitarylesions;ormiliarydisease. Thedurationof contagiousnessof anadultreceivingeffective treatmentdependsondrugsusceptibilitiesof theorganism,thenumberof organisms insputum,andfrequencyof cough. Commonly Used Drugs for Treatment of Tuberculosis in Infants, Children, and Adolescents Drugs Ethambutol Dosage Forms Tablets 100mg 400mg 2030 Twiceaweek,900mg Daily,300mg Daily Dosage, mg/kg 20 Maximum Dose 2. Less Commonly Used Drugs for Treatment of Drug-Resistant Tuberculosis in Infants, Children, and Adolescents,a continued Maximum Dose Adverse Reactions 400mg Arthropathy,arthritis Drugs Moxifloxacin Dosage, Forms Tablets 400mg Intravenoussolution 400mg/250mL in0. D c evofloxacinisnotapprovedforuseinchildrenyoungerthan18yearsof age;itsuseinyoungerchildrennecessitatesassessmentof thepotentialrisksandbenefits L (seeAntimicrobialAgentsandRelatedTherapy,p799). Althoughchildrenbetween2and12years of agewereenrolledinthetrial,dataforsafety,tolerability,andefficacyof thisregimenin thisgroupcurrentlyarenotavailable,andtheregimenisnotrecommendedforchildren youngerthan12yearsof age. If thesource caseisfoundtohaveisoniazid-resistant,rifampin-susceptibleorganisms,iso iazidshould n 1 CentersforDiseaseControlandPrevention. People at Increased Risk of Drug-Resistant Tuberculosis Infection or Disease · Peoplewithahistoryof treatmentfortuberculosisdisease(orwhosesourcecaseforthe contactreceivedsuchtreatment) · Contactsof apatientwithdrug-resistantcontagioustuberculosisdisease · Peoplefromcountrieswithhighprevalenceof drug-resistanttuberculosis · Infectedpeoplewhosesourcecasehaspositivesmearsforacid-fastbacilliorculturesafter 2monthsof appropriateantituberculosistherapyandpatientswhodonotrespondtoa standardtreatmentregimen · Residenceingeographicareawithahighpercentageof drug-resistantisolates bediscontinuedandrifampinshouldbegivenforatotalcourseof 6months. Someexpertswouldadminister3drugs(isoniazid, rifampin,andpyrazinamide)astheinitialregimenif asourcecasehasbeenidentified withknownpansusceptibleM tuberculosis,if thepresumedsourcecasehasnoriskfactors fordrug-resistantM tuberculosis,orif thesourcecaseisunknownbutthechildresidesin anareawithlowratesof isoniazidresistance. Ingeneral,extrapulmonarytuberculosis iththeexceptionof meningitis anbetreatedwiththesameregimensas -w -c usedforpulmonarytuberculosis. Atleast6monthsof therapyisindicatedfor drug-susceptibletuberculosisdiseaseif pyrazinamideisused;atleast9monthsof therapy isindicatedif pyrazinamideisnotused. If thechestradiographof themother (orhouseholdcontact)appearsabnormalbutisnotsuggestiveof tuberculosisdisease andthehistory,physicalexamination,andsputumsmearindicatenoevidenceof tuberculosisdisease,theinfantcanbeassumedtobeatlowriskof tuberculosisinfectionand neednotbeseparatedfromthemother(orhouseholdcontact). Controlledclinicaltrialsfortreatmentof M bovisdisease havenotbeenconducted,andtreatmentrecommendationsforM bovisdiseaseinadults andchildrenarebasedonresultsfromtreatmenttrialsforM tuberculosisdisease. TapwateristhemajorreservoirforMycobacterium kansasii, Mycobacterium lenteflavum, Mycobacterium xenopi, Mycobacterium simiae, andhealthcareassociatedinfectionsattributabletotherapidlygrowingmycobacteriaM abscessusand M fortuitum. Cautionmustbe exercisedininterpretationof culturesobtainedfromnonsterilesites,suchasgastricwashingspecimens,endoscopymaterial,asingleexpectoratedsputumsample,orurinespecimensandif thespeciesculturedusuallyisnonpathogenic(eg,Mycobacterium terraecomplex orMycobacterium gordonae). Althoughtheseantigensarenotfoundon M avium-intracellulare,crossreactionscanoccurwithinfectioncausedbyM kansasii, M marinum,andMycobacterium szulgai(SeeTuberculosis,p736). Isolatesof rapidlygrowingmycobacteria(M fortuitum, M abscessus,andM chelonae) shouldbetestedinvitroagainstdrugstowhichtheycommonlyaresusceptibleandthat havebeenusedwithsometherapeuticsuccess(eg,amikacin,imipenem,sulfamethoxazole ortrimethoprim-sulfamethoxazole,cefoxitin,ciprofloxacin,clarithromycin,linezolid,and doxycycline). Treatment of Nontuberculous Mycobacteria Infections in Children Initial Treatment Completeexcisionof lymphnodes;if excisionincompleteordiseaserecurs,clarithromycinorazithromycinplusethambutoland/orrifampin(orrifabutin). Twocasesof congenitalvaricella s yndromehavebeenreportedininfantsof womeninfectedafter20weeksof pregnancy, thelatestoccurringat28weeks. In tropicalclimates,theepidemiologyof varicellaisdifferent;acquisitionof diseaseoccurs atlaterages,resultinginahigherproportionof adultsbeingsusceptibletovaricella comparedwithadultsintemperateclimates. Theageof peak varicellaincidenceisshiftingfromchildrenyoungerthan10yearsof agetochildren10 through14yearsof age,althoughtheincidenceinthisandallagegroupsislowerthanin theprevaccineera. Types of Exposure to Varicella or Zoster for Which Varicella-Zoster Immune Globulin Is Indicated for People Without Evidence of Immunitya · Household:residinginthesamehousehold · Playmate:face-to-facebindoorplay · Hospital: Varicella:Insame2-to4-bedroomoradjacentbedsinalargeward,face-to-facebcontact withaninfectiousstaff memberorpatient,orvisitbyapersondeemedcontagious. Candidates for Varicella-Zoster Immune Globulin, Provided Significant Exposure Has Occurreda · Immunocompromisedchildrenbwithoutevidenceof immunityc · Pregnantwomenwithoutevidenceof immunityd · Newborninfantwhosemotherhadonsetof chickenpoxwithin5daysbeforedeliveryor within48hafterdelivery · Hospitalizedpreterminfant(28wkormoreof gestation)whosemotherlacksevidence of immunityagainstvaricella · Hospitalizedpreterminfants(lessthan28wkof gestationorbirthweight1000gorless), regardlessof maternalimmunity a SeetextandTable3. Administrationof varicellavaccinetopeoplewithout e videnceof immunity12monthsof ageorolder,includingadults,assoonaspossible within72hoursandpossiblyupto120hoursaftervaricellaexposuremaypreventor modifydiseaseandshouldbeconsideredinthesecircumstancesif therearenocontraindicationstovaccineuse. ThedecisiontoadministerVaricella-ZosterImmune Globulindependson3factors:(1)thelikelihoodthattheexposedpersonhasnoevidence of immunitytovaricella;(2)theprobabilitythatagivenexposuretovaricellaorzoster willresultininfection;and(3)thelikelihoodthatcomplicationsof varicellawilldevelop if thepersonisinfected. Subsequent exposures and follow-up of Varicella-Zoster Immune Globulin recipients. Because administrationof Varicella-ZosterImmuneGlobulincancausevaricellainfection tobeasymptomatic,testingof recipients2monthsorlaterafteradministrationof Varicella-ZosterImmuneGlobulintoascertaintheirimmunestatusmaybehelpfulin theeventof subsequentexposure. Mostexperts,however,wouldadviseVaricella-Zoster ImmuneGlobulinadministrationaftersubsequentexposuresregardlessof serologic resultsbecauseof theunreliabilityof serologictestresultsinimmunocompromised peopleandtheuncertaintyaboutwhetherasymptomaticinfectionafterVaricella-Zoster ImmuneGlobulinadministrationconferslastingprotection. If Varicella-ZosterImmuneGlobulinisnotavailableormore than96hourshavepassedsinceexposure,someexpertsrecommendprophylaxiswith acyclovir(20mg/kgperdose,administered4timesperday,withamaximumdailydose of 3200mg)orvalacyclovir(20mg/kgperdose,administered3timesperday,witha maximumdailydoseof 3000mg)beginning7to10daysafterexposureandcontinuing for7daysforimmunocompromisedpatientswithoutevidenceof immunitywhohave beenexposedtovaricella. Inaddition,theGulf Coastof LouisianaandTexas hasanendemicfocusof auniquestrainof toxigenicV choleraeO1. Theadministrationof doxycycline,tetracycline,ciprofloxacin, ofloxacin,ortrimethoprim-sulfamethoxazolewithin24hoursof identificationof the indexcasemaypreventcoprimarycasesof choleraamonghouseholdcontacts. Clinical featurescanmimicthoseof Kawasakidisease;inHiroshima,Japan,nearly10%of childrenwithadiagnosisof Kawasakidiseasehaveserologicorcultureevidenceof Y pseudotuberculosisinfection. InfectionwithY enterocoliticaisbelievedtobetransmitted byingestionof contaminatedfood(raworincompletelycookedporkproducts,tofu,and unpasteurizedorinadequatelypasteurizedmilk),bycontaminatedsurfaceorwellwater, bydirectorindirectcontactwithanimals,bytransfusionwithcontaminatedpackedred bloodcells,andrarely,byperson-to-persontransmission. Crossreactionsof theseantibodieswithBrucella, Vibrio, Salmonella,andRickettsiaorganismsand Escherichia colileadtofalse-positiveY enterocoliticaandY pseudotuberculosistiters. Otherthandecreasingthedurationof fecalexcretionof Y enterocoliticaand Y pseudotuberculosis,aclinicalbenefitof antimicrobialtherapyforimmunocompetent patientswithenterocolitis,pseudoappendicitissyndrome,ormesentericadenitishasnot beenestablished. Onthebasisof pastexperience,thesedrugs appeartobewelltolerated,donotappeartocausearthropathy,andare ffectiveasoral e agentsfortreatinganumberof diseasesinchildrenthat therwisewouldrequirepareno teraltherapy. Theperiodof odontogenesistocompletionof formationof enamelinpermanentteethappearstobethecriticaltimeforeffectsof thesedrugsandvirtuallyends by8yearsof age,atwhichtimethedrugcanbegivenwithoutconcernfordentalstaining. Doxycyclineusuallyistheagentof choicein childrenwiththeseinfections,becausedoxycyclinehasnotbeendemonstratedtocause cosmeticstainingof developingpermanentteethwhenusedinthedoseandduration r ecommendedtotreattheseseriousinfections. Principles of Appropriate Use for Upper Respiratory Tract Infections Morethanhalf of alloutpatientprescriptionsforantimicrobialagentsforchildrenare givenfor5conditions:otitismedia,sinusitis,coughillness/bronchitis,pharyngitis,and nonspecificupperrespiratorytractinfection(thecommoncold). Rarely, otherbacteriamaycausepharyngitis(eg,Corynebacterium diphtheriae, Francisella tularensis, groupsGandChemolyticstreptococci,Neisseria gonorrhoeae, Arcanobacterium haemolyticum), andtreatmentshouldbeprovidedaccordingtorecommendationsindisease-specific chaptersinSection3.
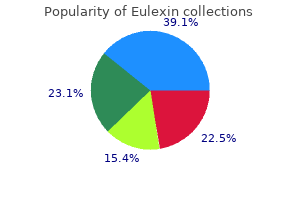
Many States and the District of Columbia require that charitable organizations regis ter and report to a governmental authority before they solicit contributions in their jurisdiction androgen hormone 1 order eulexin 250 mg on-line. A pro gram may qualify as a recipient of funds for capital prostate 75 purchase 250 mg eulexin overnight delivery, operations prostate exercises eulexin 250mg for sale, or other types of sup port such as board development from foun dations mens health zma buy cheap eulexin 250 mg line, the Community Chest prostate 7 confidence inc eulexin 250mg online, United Way prostate cancer xenograft model purchase 250mg eulexin mastercard, or other charities. Schools Local public schools may be a source of fund ing for assessments; however, they rarely pay for ongoing treatment. Some services may be reimbursable under the special entitlements for children with disabilities. Most health plans offered by large employers operate under managed care arrangements. Sometimes, a health plan may cover some substance abuse treatments under the mental health benefit portion of their plan; others may provide coverage through the medical component. Because substance abuse coverage is a minor cost to employers, accounting for about 0. Local employers may contract directly with substance abuse services providers if the ben Financing and Organizational Issues 155 · Alumni. Graduates from a program may donate money to the program or provide support for clients. Local colleges and universities may need internship slots for their students who are planning careers in human ser vices. Faithbased agencies and community centers may let the program use rooms for meetings, alumni groups, recovery support groups, or classes. Local businesses may contribute useful supplies such as snacks, office supplies, or even computers. A program can hire a consultant to write the application or use its own planning or research staff, if available. Successful grant applications address areas of genuine need, propose ideas worthy of support, express these ideas well, and explicitly follow the requirements of the request for applica tion or proposal. To design a fundable pro ject, the program may need to establish links with other resources. Each donor agency or foundation has its own application format and requirements that should be followed exactly. It is especially important when using a consultant to have program staff closely involved in the process of developing a grant application to ensure that affirmations in the application are completely aligned with agen cy capabilities. Programs that fail to involve their own staff in the grant application pro cess risk falling into the "implementation trap" when a grant is awarded for projects they are not prepared to perform. See the text box on page 157 for sources of informa tion on grants for treatment and detoxifica tion programs. For current funding opportunities, visit the National Institute on Drug Abuse Web site. Selfpay patients Some patients pay for some or all of a course of treatment themselves, without seeking reimbursement from a thirdparty payor. These patients may have no or inadequate thirdparty coverage for substance abuse treatment and are not eligible for public pay ment sources. Some patients who have cover age may prefer to pay out of their own pock ets due to concerns about the confidentiality of their information with their employer or others. Grants Government agencies and private foundations offer funding through competitive grants. Information on grants throughout the Federal government is available from. Among individuals covered by employer-sponsored benefits in 2003, 95 percent were covered under managed care arrangements (Kaiser Family Foundation and Health Research and Educational Trust 2003). The penetration of managed care into employersponsored health plans is relatively new; as recently as 1993, 46 percent were covered by indemnity plans. It is estimated that more than 160 million Americans have their behavioral health care (treatment for substance use and mental disorders) covered by a managed behavioral health care organization (Oss and Clary 1999). Behavioral health care carve-outs, so named because management of substance abuse treatment and mental health benefits are separated (carved out) from the provision and management of other healthcare services, are now the dominant approach to managed care for mental health treatment. The "carve-in" approach, which theoretically integrates traditional medical services with services for substance use and other mental disorders, is re-emerging but as of 2004 was still relatively rare. Even when health plans carve-in substance abuse services, they often use a subcontracted specialty vendor or a separate internal division with specialty expertise to manage the carve-in benefits. By 1998, all but four States had implemented some form of managed behavioral health care in their public sector treatment programs. However there is wide variation among States and large counties in the extent and form of reliance on managed Financing and Organizational Issues 157 care and in the vendors who operate such programs on behalf of government or private entities. A distinct terminology has evolved in the managed care industry-terms such as capi tation, network, or staffmodel as well as a host of acronyms. The third fundamental aspect of managed care arrangements is the requirement for per formance measurement and reporting. The staff makes a determination of what services are "medically necessary" and therefore eligible for health plan reimburse ments. If a treatment plan from a detoxification program does not meet criteria for medical necessity, it is likely to be denied and referred to a higher level clinician for review, delaying approval and payment. First, an arrangement begins It is estimated that with a managed care contract that specifies the obliga more than 160 tions of each party. It should be noted million Americans that small communi ty providers may have their have little or no negotiating leverage behavioral health in the contracting process; their only care (treatment decision may be whether or not to for substance use accept what is offered, including the rate of payment and mental and all other con tract provisions. One key aspect of any man aged care contract is the financial arrangement between the par ties, including the basis for payment and the amount of risk assumed by each party, if any. Case management programs operated in the private sector often are utilization review programs rather than the clinical case man agement programs typical in the public sec tor. Moreover, the process of case manage ment in the private sector often differs from the one found in traditional public sector mental health or substance abuse treatment agencies. Instead, it primarily involves tele phone contact, usually with a nurse, in high risk or highcost cases. If a detoxification program client has a public sector and a man aged care case manager, the detoxification program will have to interact with both to obtain initial and continuing approvals of treatment in what is called a case or utiliza tion management program. Programs will have to bear the cost of pursuing denials and requesting exceptions as well. Once a program identifies the name of the managed care plan from which payment is to be requested staff should be sure to check its Web site. Some managed care plans offer electronic data interchange with network providers to facilitate claims submission. The cost of services includes staff time spent with clients, administrative time spent on meetings and paperwork, and capital and operating expenses. Only when the actual cost of delivering a unit of a particular service is known can an agency negotiate a reasonable rate for specific services when negotiating contracts and a fiscally prudent arrangement. Determining the cost of services often entails many challenges but is absolutely essential in the current environment of accountability. Uniform System of Accounting and Cost Reporting for Substance Abuse Treatment Providers. A structured instru ment for estimating the economic cost of drug abuse treatment. Can the Treatment Services Review be used to estimate the costs of addiction and ancillary services? Benefitcost analysis of a modified therapeutic community for mentally ill chemical abusers. Measuring and Improving Cost, CostEffectiveness, and CostBenefit for Substance Abuse Treatment Programs: A Manual. Three major categories of financial arrange ments may be distinguished in managed care contracts: (1) feeforservice agreements, (2) capitation agreements, and (3) case rate agreements. Program administrators need to understand the differences among these types of arrangements so they can manage financial risk. However, the existence of a contract is no guarantee of a referral; it only enables referrals that are medically necessary. Managed care contracts vary according to two principal dimensions: (1) the method of pay ment and the corresponding type of risk assumed by the provider, and (2) the amount of payment. Each of the three major types of financial arrangements or methods of pay ment (described in Figure 61, p. Risk, of course, is a continuous variable, so that no arrangement is devoid of any risk whatsoever. The key is to ensure that a program has the tools and capabilities to manage the risks it assumes. Many managed care systems rely on feeforservice arrange ments with providers, so that most providers are paid on a discounted feeforservice basis, based on a schedule of fees described in the contract. Capitation agreements usually are reserved for very large networks of providers, who in turn pay individual providers on a feeforservice basis. Usually such providers are licensed in psy chology, nursing, medicine, or social work. They gen erally require precertification and utilization management for some or all procedures and ser vices. In a feeforservice contract, a rate is received for the services provided; typical ly, a standard program session with specific ser vices bundled in. Thus the payment rate for one visit may include a 50minute group counseling session and a urine drug screen. The rate for a day of treat ment could include, for example, onefifth of a 25 minute psychologist visit, onehalf of a urine drug screen, onehalf of a vocational training session, and two sessions of group counseling. Psychiatric services can be incorporated into the bundled services, but usual ly they are negotiated separately and treated as an additional service. Many managed care plans have separate provider networks for behavioral health ser vices. It is important for detoxification providers to participate in both medical and behavioral health networks, given that detoxi fication benefits may be considered either medical or behavioral benefits. In addition to the credentials of the staff and practitioners, the program itself may have to be accredited by one of the major national health care accrediting organizations. These include the Commission on Accreditation of Rehabilitation Facilities, the National Committee for Quality Assurance and the Joint Commission on Accreditation of Healthcare Organizations. All ser vices should be costed out prior to negotiation, so actual costs of treatment components are known and can be compared to the reimbursement offered. Programs must understand that even if a feeforservice contract is successfully negotiated, referrals may or may not follow. The provider agrees to provide all or some of the treatment services for an expected number of managed care "covered lives". Usually only large service providers have the assets and volume of services to engage in capitated agreements. Cautions/Risks for Programs the two critical elements are the per member/per month (pm/pm) rate and the utilization rate. If many more people than are predicted require treatment, the provider may not be able to cover service delivery costs, much less make a profit/sur plus. If the provider bears in mind these caveats, this regular, guaranteed payment can be an excellent arrangement but carries with it the risks of both "overutilization" (when com pared to the assumption used in developing the rate) and the need for a greater intensity of treat ment than the capitation rate can cover. In some cases a program may want to accept a somewhat speculative capitation rate in order to join a panel and then renegotiate that rate after the program has collected data that show that it needs a higher rate to cover its costs. In any case, it is crucial to track actual dollars against the budget in real time to avoid unexpected deficits. A case rate agreement removes some of the utiliza tion risk from the service provider. However, the risk remains that clients will need services more frequently or at higher levels than the case rate covers. It is essential that programs track costs by specific client in order to assess the adequacy of a proposed case rate. However, it is a mistake to consider a case rate as a cap for any specific patient; the goal is to ensure that the average cost per case is lower than the negotiated case rate, not that the cost for each case is less than the negotiat ed rate. Once again, it is crucial to track actual average dollars per case against the contracted case rate in real time to avoid unexpected deficits. The case rate is a fixed rate per client paid for delivery of specific ser vices to specified types of consumers. For this fee, a provider such as a clinic covers all the services that a client requires for a specific period. Usually those receiving services under capitation are a small minority of those covered. The case rate may be "riskadjusted" to compensate for the higher costs of serving clients who predictably need more services than average. Organizational Performance Measurement Performance measurement is becoming an increasingly important component of man aged and feeforservice care in both the public and private sectors. Their cus tomers, employers, or public purchasers may use adequacy of performance on these mea sures in their decisions to acquire or retain their plans for their employees. Nevertheless, it is equally important to recognize that employing mea surement is an integral component of external and internal accountability as well as continu ous clinical improvement. One of the primary independent entities involved in the construction of national per formance measures for substance abuse treat ment is the Washington Circle Group. Treatment ·Initiation of alcohol and other plan ser vices ·Linkage of detoxification and alcohol and other drug plan services ·Treatment engagement ·Use of interventions for family members and significant others 4. Performance measurement is becoming increasingly important outside of managed care contracts as well as inside them. Each State will expect pro grams to understand and be able to measure the required indicators accurately and in a timely way.
Order eulexin 250 mg with visa. mens health home gym review part 1.
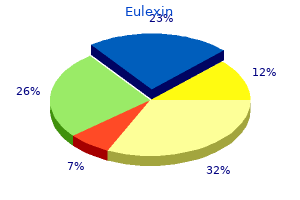
References