




|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Lorenzo Biassoni, MSc, FRCP, FEBNM
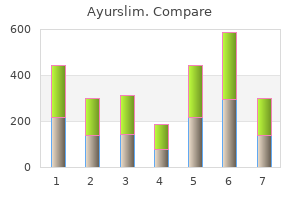
Five of the original nine specimens had evidence of endolabyrinthitis gayatri herbals order 60 caps ayurslim amex, and virus was isolated from the endolymph in three of the nine specimens [420] herbs chips cheap ayurslim 60caps overnight delivery. Viral antigen was detected by immunofluorescence in two cases in which routine histology failed to show viral inclusions [207] yak herbals pvt ltd purchase 60 caps ayurslim otc. Cochlear and vestibular findings were variable and ranged from rare inclusion-bearing cells in or adjacent to the sensory neuroepithelium of the cochlea or vestibular system to more extensive involvement of the nonsensory epithelium herbals that prevent pregnancy generic 60caps ayurslim mastercard. Routine histology failed to detect viral inclusions in the auditory and vestibular neural structures, but viral antigens were detected in the spiral ganglion when specimens were examined by immunofluorescence [207]. Inflammatory infiltrates were minimal and reported in only three patients in this series [420]. In this patient, extensive cellular degeneration, fibrosis, and calcifications were observed in the cochlea and vestibular systems [421]. First, in all but two of these cases, virus, viral antigens, or histopathologic findings consistent with virus infection were present in the cochlea or vestibular apparatus. These findings indicate that virus replication could have occurred in the sensory neuroepithelium and nonsensory epithelium and that cellular damage could be explained by a direct viral cytopathic effect. In addition, viral-induced damage can also result from bystander effects secondary to immune-mediated cytopathology. An alternative and not exclusive possibility is that infection of the inner ear structures is a late, and in some cases a postnatal, event. In this case, findings from specimens of the above-described autopsy series may reflect recent infection before host inflammatory responses. A third possibility is that hearing loss in some infected infants is related to alterations in the neural networks leading from the cochlea to the eighth cranial nerve. Small animal models have provided some information and have mirrored findings in humans. Virus and inflammation are required for the development of pathology in the inner ear. A study in guinea pigs showed that virus infection in immunocompromised animals was not associated with the typical pathologic findings of virus infection in normal animals [422]. Interrupting either virus replication or the local host inflammatory response could offer some therapeutic benefit to these patients. Intrauterine transmission after primary infection occurs in 30% to 40% of cases [121,212]. With regard to the role of gestational age on the expression of disease in the fetus and offspring, infection at an earlier gestational age has been associated with more severe disease and worse outcome [122,212,431,432,434]. Definition of the interval in pregnancy in which maternal seroconversion occurred does not define a similar time of fetal infection, however. Despite the inability of maternal immunity to prevent transmission of this virus to the fetus, congenital infections that result from recurrent infections are thought to be less likely to produce clinical evidence of disease in infected offspring than those resulting from primary infections [121,430]. These studies have shown that clinically apparent congenital infections are frequently observed in infants infected after a recurrent maternal infection and that long-term sequelae such as hearing loss can be present in such infants. Clinical experience continues to suggest, however, that severe multiorgan disease in congenitally infected infants should suggest the possibility of primary maternal infection. It is unknown if preexisting cellular immunity is more important than humoral immunity; however, maternal IgG antibodies are transmitted to the fetus and at a first approximation could alter the virologic parameters of fetal infection. This result would argue that when virus enters the fetus, a critical balance between fetal immunity, maternal immunity that can be transferred to the fetus, and viral inoculum determines the extent and severity of fetal infection. Such a complex relationship between virus and immunity suggests that analysis of specimens derived from human natural history studies would likely provide only a limited insight into this intrauterine infection. Virus is consistently shed into the urine for 6 years or longer and into saliva for 2 to 4 years. Not only does excretion persist much longer in congenitally infected infants than in infected older children and adults, but also the quantity of virus excreted is much greater. B, Genomic copies of human cytomegalovirus in blood from congenitally infected infants with symptomatic (l) and asymptomatic infections. The distinctive features include large cells 20 to 35 mm in diameter with a large nucleus containing round, oval, or reniform inclusions. The cytoplasmic inclusions vary from minute dots to distinct rounded bodies 3 to 4 mm in diameter. The cytoplasmic inclusions are usually aggregated opposite to the eccentrically placed inclusion-bearing nucleus and seem to represent a cytoplasmic site of virus assembly [462]. In most infected infants, the infection can be described grossly as focal encephalitis and periependymitis. Encephalitis can involve cells of the gray and the white matter and cells within the choroid plexus. Inclusion-bearing cells have been identified in neurons, glia, ependyma, choroid plexus, meninges, and vascular endothelium and in cells lying free in the ventricles. Rarely, inclusion-bearing cells have been identified in the cerebrospinal fluid [466]. Previous descriptions have emphasized the periventricular location of calcifications; however, these lesions can be located anywhere in the brain [398,404,408]. The histopathologic changes associated with retinitis begin as an acute vasculitis that spreads into the choroid through the vascular basement membrane. Anecdotal cases of cataracts have been described in congenitally infected infants. Chorioretinitis in congenitally infected infants has been associated with an increased risk of long-term cognitive disorders in congenitally infected infants [476]. Liver calcifications have been detected radiologically in infants with congenital infections [477,478]. Clinical and laboratory evidence of liver disease eventually subsides in surviving infants, and only anecdotal cases of cirrhosis have been reported. Hematopoietic System Hematologic abnormalities, including thrombocytopenia, anemia, and extramedullary hematopoiesis, are common in symptomatically infected infants, but these abnormalities almost invariably resolve within the 1st year of life. The exact mechanism accounting for these disturbances is uncertain, although congestive splenomegaly resulting in platelet and red blood cell trapping must play some part in the overall process. Significant splenomegaly is common, and congestion, extramedullary hematopoiesis, and diminished size of lymphoid follicles can be seen histologically. The presence of indirect hyperbilirubinemia, extramedullary hematopoiesis, and erythroblastemia indicates active hemolysis, but mechanisms that account for these findings have not been well described. Microscopically, inclusion-bearing cells are commonly seen, especially in the cells lining the distal convoluted tubules and collecting ducts [383,479]. Affected cells may desquamate into the lumens of the tubules and appear in the urine sediment. Mononuclear cell infiltration may be present in the peritubular zones of the kidney. Some reports describe intralobular or periductal mononuclear infiltration, suggesting focal pancreatitis. Clinical evidence of hepatitis as manifested by hepatomegaly, elevated levels of serum transaminases, and direct hyperbilirubinemia is frequently seen in infants with symptomatic congenital infections. There are no reliable figures, however, on the frequency of involvement because the examination of the salivary glands is not always part of autopsies [383].
Symptoms in giardiasis are related to the age of the patient: Diarrhea herbals are us best 60 caps ayurslim, vomiting komal herbals ayurslim 60caps overnight delivery, anorexia herbs direct discount 60caps ayurslim with visa, and failure to thrive are more common in younger children vhca herbals buy discount ayurslim 60caps on line. In a study of lactating Bangladeshi mothers and their infants, 82% of women and 42% of infants excreted Giardia once during the study; in some infants, this occurred before they were 3 months old [1094]. Of these infected infants, 86% had diarrhea, suggesting that the early exposure to the parasite resulted in disease. In a prospective study of diarrhea conducted in Mexico, infants frequently were infected with Giardia from birth to 2 months, with a crude incidence rate of first Giardia infection of 1. The symptom status of these children was not reported, but this study strongly suggests that G. In areas with high endemicity, infection of the newborn is likely to be associated with inadequate maternal and delivery care, insufficient environmental sanitation, and poor personal hygiene standards. The occurrence of symptomatic intestinal parasitic infection during the first month of life requires acquisition of the parasite during the first days or weeks; the incubation period for E. The newborn can be infected during delivery by contact with maternal feces [1075], in the hospital through contact with the mother or personnel, or in the household through contact with infected individuals in close contact with the infant. The former can cause acute nonbloody and bloody diarrhea, necrotizing enterocolitis, ameboma, and liver abscess, and the latter is a noninvasive parasite that does not cause disease. Enteric viruses include rotaviruses, enteric adenoviruses, human caliciviruses, and astroviruses. Other viruses such as coronaviruses, Breda viruses, pestiviruses, parvoviruses, toroviruses, and picobirnaviruses have been sporadically associated with acute diarrhea, but are currently considered of uncertain relevance. More recently, Bocaviruses have been postulated as potential respiratory and intestinal pathogens, but the latter seems unclear [1125]. All four enteric viruses could conceivably infect the newborn, but the extent of exposure and clinical manifestations are largely unknown for astrovirus, enteric adenovirus, and human caliciviruses. Neonatal rotavirus infections have similar virologic and clinical characteristics to infection in older children, although some differences exist. Asexual reproduction and sexual reproduction occur, with the latter resulting in formation of new oocysts that can be passed in stools. Because Cryptosporidium infects a wide variety of animal species, there is often a history of animal contact among infected individuals [1104]. Water-borne outbreaks of cryptosporidiosis occur and can be of massive proportions [1111]. The clinical manifestations of cryptosporidiosis in immunocompetent individuals resemble Giardia infection, but are shorter in duration [1112]; asymptomatic carriage is rare. Symptoms and signs include watery diarrhea, abdominal pain, myalgia, fever, and weight loss. Infants infected early in life may develop chronic diarrhea and malnutrition [1118]. Nitazoxanide is effective therapy of immunocompetent adults and children with cryptosporidiosis [1122]. Because illness is usually self-limited in the normal host, attention to fluid, electrolyte, and nutritional status is usually sufficient. Enteric isolation of hospitalized infants with this illness is appropriate because of the high infectivity. Several studies suggest that the risk of infection early in life may be decreased by breast-feeding [1116,1123], Using appropriate filtration systems in areas where water treatment is minimal can have a significant impact in decreasing cases of cryptosporidiosis [1124]. Six distinct rotavirus groups (A through F) have been identified serologically based on common group antigens [1130,1131], of which three (A, B, and C) have been identified in humans [1126]. Because group A rotaviruses represent more than 95% of isolated strains in humans worldwide, further discussion focuses on this group. Group A rotaviruses are subclassified into serotypes based on neutralization epitopes located on the outer capsid. Combining G antigenic with P antigenic and genetic typing, a specific rotavirus strain can be identified: P antigenic type (P genetic type), G type. Some of these strains seem to be associated with occurrence of asymptomatic infections, although the existence of naturally acquired asymptomatic strains is controversial. Neonates can also be symptomatically infected with unusual animal-human reassortant strains in areas of poor sanitary conditions [1146]. Pathogenesis Although mechanisms involved in rotavirus pathogenesis have been extensively studied, current understanding of the exact mechanisms involved in human disease is only partial and may be subject to significant conceptual modifications as more knowledge is obtained in the future. Lactase, which is present only on the brush border of the differentiated epithelial cells at these sites, may act as a combined receptor and uncoating enzyme for the virus, permitting transfer of the particles into the cell [1152]. Perhaps for this reason, infection is limited to the mature columnar enterocytes; crypt cells and cryptderived cuboidal cells, which lack a brush border, seem to be resistant to rotaviral infection [1152,1153]. The upper small intestine is most commonly involved in rotavirus enteritis, although lesions may extend to the distal ileum and rarely to the colon [1156,1157], Interaction between intestinal cell and rotavirus structural and nonstructural proteins occurs, resulting in death of infected villous enterocytes [1158]. When infected, the villous enterocyte is sloughed, resulting in an altered mucosal architecture that becomes stunted and flattened. The gross appearance of the bowel is usually normal; however, under the dissecting microscope, scattered focal lesions of the mucosal surface are apparent in most cases. Light microscopy also shows patchy changes in villous morphology, compatible with a process of infection, inflammation, and accelerated mucosal renewal. The villi take on a shortened and blunt appearance as tall columnar cells are shed and replaced by less mature cuboidal enterocytes [1148,1150,1159]. Ischemia may also play a role in the loss and stunting of villi [1160] and activation of the enteric nervous system; active secretion of fluid and electrolytes may be another pathogenic mechanism [1161]. During the recovery phase, the enteroblastic cells mature and reconstruct the villous structure. Because of the loss of mature enterocytes on the tips of the villi, the surface area of the intestine is reduced. More recent studies suggest that destruction of mature enterocytes does not seem to be a critical element in the pathogenesis of rotavirus infection. The exact mechanism of action of this protein at the intestinal level is only partially understood, but known to be different from the action of bacterial enterotoxins. Rotavirus antigenemia and viremia seem to be common events during rotavirus infection, a concept that revolutionized understanding of this infection [1168]. These events could partly explain the sporadic reports of systemic disease associated with rotavirus intestinal infections mentioned further on. Infection and Immunity Infants with asymptomatic rotavirus infections in the nursery are less likely than uninfected nursery mates to experience severe rotavirus infection later in life [1172,1173]; this finding suggested protective immunity and supported vaccine development. Breast-feeding protects against diarrhea and specifically rotavirus disease during the first year of life [62,72], probably including newborns [1161]. The high prevalence of antirotaviral antibodies in colostrum and human milk has been shown by numerous investigators in widely diverse geographic areas [12]. Rotavirus-specific IgG antibodies have been found during the first few postpartum days in about one third of human milk samples assayed [1184,1187], whereas IgM antibodies were detectable in about half [1187]. The concentration of one milk glycoprotein, lactadherin, was found to be significantly higher in human milk ingested by infants who developed asymptomatic rotavirus infection than in milk ingested by infants who developed symptomatic infection [59].
Buy 60caps ayurslim with amex. HIMALAYA HERBALS PURIFYING NEEM FACE WASH HONEST REVIEW.
Some investigators suggest that too many healthy term infants have a diagnostic evaluation for sepsis aasha herbals purchase 60 caps ayurslim with amex, including lumbar puncture herbals for hot flashes buy ayurslim 60 caps low cost, based solely on maternal risk features and that lumbar puncture rarely provides clinically useful information herbalsmokecafecom discount 60 caps ayurslim with amex. Three of the four infants with meningitis were bacteremic with the same pathogen [548] herbs for weight loss discount ayurslim 60caps on-line. Fielkow and colleagues [550] found no cases of meningitis among 284 healthy-appearing infants who had lumbar puncture performed because of maternal risk factors, whereas 2. The value of lumbar puncture has been established for infants with clinical signs of sepsis, but lumbar puncture performed because of maternal risk features in a healthy-appearing neonate is less likely to be useful. One third (45 of 134) of these high-risk neonates with meningitis has negative blood cultures. Lower gestational age and prior sepsis were important risk factors for development of meningitis, which carried a significant risk of mortality compared with uninfected infants (23% versus 2%). These results indicate the critical importance of lumbar puncture and suggest that meningitis may be significantly underdiagnosed in very low birth weight infants [545]. Weisman and colleagues [555] observed that transient hypoxemia occurred during lumbar puncture performed in the lateral position. Ventriculitis is diagnosed on the basis of elevated white blood cell count (>100 cells/mm3) or identification of bacteria by culture, Gram stain, or antigen detection. Ventricular puncture is a potentially hazardous procedure and should be performed only by a physician who is an expert in the technique. If a Lumbar Puncture Is Not Performed Is it sufficient to culture only blood and urine for the diagnosis of neonatal bacterial meningitis Franco and colleagues [557] reported that in 26 neonates with bacterial meningitis, only 13 had a positive blood culture. A significant number of infants with meningitis do not have this diagnosis established unless lumbar puncture is performed. Ideally, lumbar puncture should be performed before the initiation of antimicrobial therapy, but there are alternative strategies for infants who may not tolerate the procedure. If the physician believes that lumbar puncture would endanger the infant with presumed sepsis and meningitis, therapy should be initiated after blood (and urine for late-onset illness) is obtained for culture. Gleason and colleagues [551] suggested that the procedure be performed with the infant in the upright position or, if performed in the flexed position, be modified with neck extension. Pinheiro and associates [552] evaluated the role of locally administered lidocaine before lumbar puncture and found that the local anesthesia decreased the degree of struggling of the infant. Other investigators concluded, however, that local anesthesia failed to influence physiologic changes in the neonate undergoing lumbar puncture [553]. Fiser and colleagues [554] suggested that the administration of oxygen before lumbar puncture prevents most hypoxemia resulting from this procedure in infants. Patients 135 20 87 35 40 108 Age (Days) 1 7 Most <7 0-4 wk 4-8 wk 0-30 White Blood Cells (mm3)* 12 (0-42) 3 (0-9) 8. Samples 6 17 15 8 14 11 Red Blood Cells (mm3)* 335 (0-1780) 1465 (0-19,050) 808 (0-6850) 407 (0-2450) 1101 (0-9750) 661 (0-3800) White Blood Cells (mm3)* 3 (1-8) 4 (0-14) 4 (0-11) 4 (1-10) 7 (0-44) 8 (0-23) Neutrophils (%)* 11 (0-50) 8 (0-66) 2 (0-36) 4 (0-28) 10 (0-60) 11 (0-48) Glucose (mg/dL)* 70 (41-89) 68 (33-217) 49 (29-90) 74 (50-96) 59 (39-109) 47 (31-76) Protein (mg/dL)* 162 (115-222) 159 (95-370) 137 (76-260) 136 (85-176) 137 (54-227) 122 (45-187) Birth Weight (g) <1000 1000-1500 0-7 8-28 29-84 *Expressed as mean with range (number in parentheses) or +/- standard deviation unless otherwise specified. In term infants, total protein concentration decreases with age, reaching values of healthy older infants (<40 mg/dL) before the third month of life. Healthy term infants may have blood glucose levels of 30 mg/dL, and preterm infants may have levels of 20 mg/dL [568]. Explanations that have been offered include possible mechanical irritation of the meninges during delivery and increased permeability of the blood-brain barrier. Only the study by Ahmed and colleagues [562] included in the definition of normal the absence of viral infection, defined by lack of evidence of cytopathic effect in five cell lines and negative polymerase chain reaction for enteroviruses. None of the studies included information about the health of the infant after the newborn period. Observations of these infants over the course of months or years can reveal abnormalities that are inapparent at birth. Presumably, the initial lumbar puncture was performed early in the course of meningitis before an inflammatory response occurred. Dissemination of the organisms from the blood to the meninges can occur after the first lumbar puncture before sterilization of the blood by appropriate antimicrobial therapy occurs. This dissemination is especially likely to occur in neonates with intense bacteremia where sterilization by b-lactam agents. Among products that have been evaluated and found to be inadequate to distinguish bacterial meningitis from other neurologic disease (including cerebroventricular hemorrhage and asphyxia) are g-aminobutyric acid [574], lactate dehydrogenase [575], and creatine kinase brain isoenzyme [576]. In a cohort study of lumbar punctures performed at 150 neonatal units from 1997-2004, 39. The authors found that adjustment of the leukocyte count to account for blood contamination resulted in loss of sensitivity and only marginal gain in specificity, and would not aid in the diagnosis of bacterial (or fungal) meningitis [593]. Because a "bloody tap" is difficult to interpret, it may be valuable to repeat the lumbar puncture 24 to 48 hours later. If the results of the second lumbar puncture reveal a normal white blood cell count, bacterial meningitis can be excluded. If respiratory abnormalities are apparent or respiratory status has changed, a radiograph of the chest should be performed. Because the clinical manifestations of sepsis can be subtle, the progression of the disease can be rapid, and the mortality rate remains high compared with mortality for older infants with serious bacterial infection, presumptive treatment should be initiated promptly. Many infants who have a clinical course typical of bacterial sepsis are treated empirically because of the imperfect sensitivity of a single blood culture in the diagnosis of sepsis. Brain Abscess Brain abscess is a rare entity in the neonate, usually complicating meningitis caused by certain gram-negative bacilli. Treatment of the infant who becomes septic while in the nursery after age 6 days (late-onset disease) must include therapy for hospital-acquired organisms, such as S. There are no clinical data to indicate that continuing an aminoglycoside in combination with a penicillin after 72 hours results in more rapid recovery or improved outcome for infected neonates (see Chapter 12). Mehr and Doyle [607] reviewed the more recent literature on cytokines as aids in the diagnosis of neonatal bacterial sepsis. Many of these organisms are susceptible to penicillinase-resistant penicillins, such as nafcillin, and to first-generation cephalosporins. Methicillin-resistant staphylococci that are resistant to other penicillinaseresistant penicillins and cephalosporins have been encountered in many nurseries in the United States. Bacterial resistance must be considered whenever staphylococcal disease is suspected or confirmed in a patient, and empirical vancomycin therapy should be initiated until the susceptibility pattern of the organism is known. Virtually all staphylococcal strains isolated from neonates have been susceptible to vancomycin. Synergistic activity is provided by the combination of an aminoglycoside (see Chapter 14). Enterococcus species are only moderately susceptible to penicillin and highly resistant to cephalosporins. Optimal antimicrobial therapy for neonatal infections caused by Enterococcus includes ampicillin or vancomycin in addition to an aminoglycoside, typically gentamicin or tobramycin. The choice of antibiotic therapy for infections caused by gram-negative bacilli depends on the pattern of susceptibility for these isolates in the nursery that cares for the neonate. These patterns vary by hospital or community and by time within the same institution or community. Although isolates from neonates should be monitored to determine the emergence of new strains with unique antimicrobial susceptibility patterns, the general pattern of antibiotic susceptibility in the hospital is a good guide to initial therapy for neonates. Aminoglycosides, including gentamicin, tobramycin, netilmicin, and amikacin, are highly active in vitro against virtually all isolates of E. The thirdgeneration cephalosporins provide concentrations of drug at most sites of infection that greatly exceed the minimum inhibitory concentrations of susceptible pathogens, and there is no dose-related toxicity. Because ceftriaxone can displace bilirubin from serum albumin, it is not recommended for use in neonates unless it is the only agent effective against the bacterial pathogen. Meropenem is a broad-spectrum carbapenem antibiotic with extended-spectrum antimicrobial activity including P. The rapid development of resistance of gram-negative enteric bacilli when cefotaxime is used extensively for presumptive therapy for neonatal sepsis suggests that extensive use of third-generation or fourth-generation cephalosporins can lead to rapid emergence of drugresistant bacteria in nurseries [625]. Also of concern, studies have identified a principal risk factor for development of invasive infection with Candida and other fungi in preterm neonates to be extended therapy with third-generation cephalosporins [626,627].
In contrast herbs used for protection generic ayurslim 60 caps, urine should be collected for culture from infants with suspected late-onset sepsis before initiation of antimicrobial therapy herbals in india 60 caps ayurslim with mastercard. Because of the difficulty in collecting satisfactory cleanvoided specimens of urine from newborns elchuri herbals effective ayurslim 60caps, bladder catheterization or suprapubic needle aspiration of bladder urine frequently is performed herbals ltd buy ayurslim 60 caps on line. If a suprapubic aspirate cannot be performed for technical or medical reasons, catheterization is a satisfactory method of obtaining urine, although ambiguous results can occur because of contamination from the urethra, especially in very low birth weight neonates. Application of a clinical pain scoring system employing a blinded observer and video recording found suprapubic aspiration to produce more discomfort than transurethral catheterization in female and circumcised male infants younger than 2 months of age [529]. In contrast to findings reported for adult populations [517], there were no false-positive results among almost 200 infants with negative blood cultures. Failure to identify organisms was attributed to extreme neutropenia in several patients. Cultures of Tracheal Aspirates and Pharynx Because of the association of pneumonia and bacteremia, investigators have sought to determine the risk of sepsis on the basis of colonization of the upper respiratory tract. Growth of a bacterial pathogen from a tracheal aspirate culture does not predict which infants will develop sepsis, however. Similarly, cultures of the pharynx or trachea do not predict the causative organism in the blood of a neonate with clinical sepsis [531]. A review of the literature by Srinivasan and Vidyasagar [532] suggests endotracheal aspirates are of poor sensitivity (approximately 50%), modest specificity (approximately 80%), and poor positive predictive value. Unless the patient has a change in respiratory status documented clinically and radiographically, routine use of cultures from the pharynx or trachea provide low diagnostic yield and seem unjustified given their expense. Diagnostic Needle Aspiration and Tissue Biopsy Direct aspiration of tissues or body fluids through a needle or catheter is used for the diagnosis of a wide variety of infectious and noninfectious diseases [533]. Aspiration of an infectious focus in lung, pleural space, middle ear, pericardium, bones, joints, abscess, and other sites provides immediate and specific information to guide therapy. Biopsy of the liver or bone marrow can assist in diagnosing occult infections, but this rarely is necessary. Autopsy Microbiology Two factors must be considered in interpreting bacterial cultures obtained at autopsy: the frequent isolation of organisms usually considered to be nonpathogenic and the difficulty of isolating fastidious organisms such as anaerobic bacteria. To minimize these problems, it is important that specimens be collected with proper aseptic technique and as early as possible after death. It is a common belief that organisms in the intestinal and respiratory tracts gain access to tissues after death, but it also is possible that bacteremia occurs shortly before death and is not a postmortem phenomenon. Eisenfeld and colleagues [534] identified the same organisms in specimens obtained before and within 2 hours after death. Confusion in the interpretation of results of bacteriologic cultures often is obviated by the review of slides prepared directly from tissues and fluids. If antimicrobial treatment was administered before death, organisms can be observed on a smear even though they are not viable. Pathogens would be expected to be present in significant numbers and accompanied by inflammatory cells, whereas contaminants or organisms that invade tissues after death, if they are seen, would be present in small numbers with no evidence of an inflammatory process [535,536]. Counterimmunoelectrophoresis also was used successfully for detecting the capsular polysaccharide antigens of various pathogenic bacteria, including S. Latex agglutination detection now is preferred because of its speed, simplicity, and greater sensitivity for selected organisms. Kits designed to detect cell wall or capsular or cell wall antigen released into body fluids are commercially available. The overall incidence of bacterial meningitis is less than 1 case per 1000 infants, but the incidence for low birth weight (<2500 g) infants or premature infants is severalfold higher than the incidence for term infants. Empirical use of cefotaxime in neonates should be restricted to infants with evidence of meningitis or with gram-negative sepsis. Continued cefotaxime therapy should be limited to infants with gramnegative meningitis caused by susceptible organisms or infants with ampicillin-resistant enteric infections [628]. If there is a concern for endemic or epidemic staphylococcal infection, typically occurring beyond 6 days of age, the initial treatment of late-onset neonatal sepsis should include vancomycin. The hospital laboratory must regularly monitor isolates of pathogenic bacteria to assist the physician in choosing the most appropriate therapy. The clinical pharmacology and dosage schedules of the various antimicrobial agents considered for neonatal sepsis are provided in Chapter 37. In complicated cases of neonatal meningitis, the proper duration of therapy may be prolonged and is best determined in consultation with an infectious diseases specialist. The third-generation cephalosporins, cefotaxime, ceftriaxone, and ceftazidime, have important theoretical advantages for treatment of sepsis or meningitis compared with therapeutic regimens that include an aminoglycoside. In contrast to the aminoglycosides, third-generation cephalosporins are not associated with ototoxicity and nephrotoxicity. Little toxicity from aminoglycosides occurs when use is brief, however, or, when continued for the duration of therapy, if serum trough levels are maintained at less than 2 mg/mL. Because cephalosporins have no dose-related toxicity, measurements of serum concentrations, which are required with the use of aminoglycosides beyond 72 hours or in infants with renal insufficiency, are unnecessary. Routine use of cephalosporins for presumptive sepsis therapy in neonates often leads to problems with drug-resistant enteric organisms, however. Extensive use of third-generation cephalosporins in the nursery could result in the emergence of resistance caused by de-repression of chromosomally mediated b-lactamases [630]. Ceftazidime or meropenem in combination with an aminoglycoside should be used in therapy for P. Use of ceftriaxone in the neonate should be determined on a case-by-case basis because of its ability to displace bilirubin from serum albumin and result in biliary sludging. When ampicillin or penicillin is administered to the mother, drug concentrations in the fetus are more than 30% of the concentrations in the blood of the mother [638]. Parenteral antibiotic therapy administered to a mother with signs of chorioamnionitis in labor essentially is treating the fetus early in the course of the intrapartum infection [639,640]. For some infected fetuses, the treatment administered in utero is insufficient, however, to prevent signs of early-onset group B streptococcal disease. Although maternal intrapartum prophylaxis has been associated with a 75% decrease in the incidence of early-onset group B streptococcal disease since 1993 [641,642], the regimen has had no impact on the incidence of late-onset disease [643]. Infants who have signs of sepsis should receive a full diagnostic evaluation and should be treated, typically with ampicillin and gentamicin, until laboratory studies are available. The same management probably is necessary for infants of any gestation whose mothers received vancomycin for prophylaxis because nothing is known about the amniotic fluid penetration of this drug or its efficacy in preventing early-onset group B streptococcal disease. The first two clinical scenarios are readily identified, but the third category often leads to controversy regarding optimal management. Recommendations for prevention and treatment of early-onset group B streptococcal infection are discussed in detail in Chapter 12. Management of the infant born to a mother who received an antimicrobial agent within hours of delivery must include consideration of the effect of the drug on cultures obtained from the infant after birth. Antimicrobial agents cross the placenta and achieve concentrations in fetal tissues that are parallel to concentrations achieved in other well-vascularized organs. If the neonate seems to be well and there is reason to believe that infection was unlikely, treatment can be discontinued at 48 hours. If the clinical condition of the infant remains uncertain and suspicion of an infectious process remains, therapy should be continued as outlined for documented bacterial sepsis unless another diagnosis becomes apparent. Squire and colleagues [645] found that results of premortem blood cultures were negative in 7 (18%) of 39 infants with unequivocal infection at autopsy. Some infants with significant systemic bacterial infection may not be identified by the usual single blood culture technique. The physician must consider this limitation when determining length of empirical therapy. If treatment for infection is deemed necessary, parenteral administration for 10 days is recommended.