




|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
R. Bryan Bell, MD, DDS, FACS
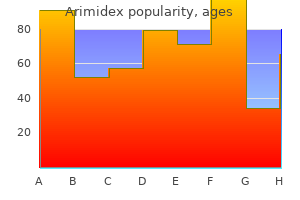
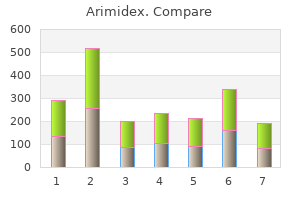
An interdigitating womens health 21740 purchase arimidex 1mg with visa, microcystic pregnancy 3 weeks symptoms purchase arimidex 1mg visa, diffuse lymphatic malformation menstruation gas pain purchase arimidex 1 mg overnight delivery, with involvement of the neck menstruation problems generic 1mg arimidex mastercard, mandible womens health usa arimidex 1mg otc, floor of mouth womens health texas medicaid purchase 1mg arimidex with visa, and near-total infiltration of the tongue. The mylohyoid muscle is a typical boundary used to divide these massive lesions into several "zones. For instance, the physician should attempt to deal with the tongue before dealing with the floor of mouth and then approach the neck; this approach prevents superior swelling of the untreated zone. In addition, children with diffuse cervicofacial disease also frequently require maxillomandibular reconstruction owing to overgrowth of the facial bones. It is also advisable in the care of children with diffuse disease to involve a child psychiatrist. These children will likely have long-term morbidity, and a means for dealing with the psychosocial implications is essential. The cause of the trauma can be quite variable, ranging from industrial and motor vehicle accidents to interpersonal trauma involving either fists or weapons. It is common for trauma to be related to substance abuse or to behavior that can be linked to substance abuse. Sometimes trauma is related to sports activities or simply to accidental or work-related occurrences. In contrast, soft-tissue injuries are often repaired as soon as it is practically possible. Low-velocity injuries, such as isolated nasal and mandible fractures, do not usually require the same highly consultative and collaborative team approach, especially if no other injuries are found or suspected. With isolated injuries, which tend to be more minor than multisystem injuries, treatment can be better directed; it can proceed on a pace both commensurate with and concentrated upon the direct injury. Committee on Trauma, Advanced Trauma Life Support for Doctors, Instruction Manual, 6th ed. In the initial management period, even occurrences of severe craniofacial trauma may be examined after cases of abdominal, thoracic, and-at times-limb trauma. A neurosurgical examination and clearance are frequently desirable in severe high-velocity injuries. When ocular injury is suspected, an examination by an ophthalmologist can be indispensable. Patients on the most severe end of the injury spectrum often require airway control via orotracheal intubation or, in certain cases, via cricothyroidotomy or tracheotomy. Most attempts to repair maxillofacial trauma will be considered after the patient is stabilized. A temporal injury may lacerate the superficial temporal artery or a scalp laceration may contribute to the loss of many units of blood. The discrete clamping of an arterial vessel in a laceration may be necessary if the physician is unable to gain adequate control of blood loss by applying simple pressure. Scalp injuries usually respond to closure with a few simple mattress sutures or a pressure dressing. This blood loss management allows time for the rest of the trauma evaluation to proceed and for the patient to be stabilized. Primary closure is direct edge-to-edge skin approximation using fine sutures with precise suture approximation of deeper tissue layers. Protecting the patient prophylactically with tetanus immunoglobulin and tetanus toxoid should be considered. In contaminated wounds, which are extremely common, prophylactic antibiotic administration should also be strongly considered. This closure can be improved with the discrete undermining of skin flaps, where necessary, to produce a tension-free closure. The key elements to obtaining good results with wound closure are (1) having a clean and sterile wound, (2) respecting anatomic boundaries, (3) avoiding tension on the suture line, and (4) having atraumatic surgical technique. The wound should be closed in layers, in the following order: (1) muscle, (2) subcutaneous tissue, (3) subcuticular tissue, and (4) superficial skin. Chromic gut sutures are useful for deep closure; fine nylon or proline stitches are useful for skin closure. Although polyglactin (eg, Vicryl) and polyglycolic acid (eg, Dexon) can also be used for deep stitches, they can sometimes become infected due to sluggish absorption, which can lead to their eventual migration out of the wound. These sutures have the advantage of leaving little trace of their placement and dissolving without requiring removal. These types of stitches may also be useful in children to prevent the need for future stitch removal or when patient follow-up is doubtful. When taking care of patients with heavy beards or dark facial hair, it is best to use a skin suture color other than black to facilitate future removal. If wound coverage is difficult because of lost skin, transposition flaps can be used to create closure. If they are required, it is often best to accomplish the closure in the operating room setting as instrument sets and nursing assistance become more critical. The risk in using transposition flaps is that the wound is usually contaminated; utilizing these flaps may increase the risk of tissue loss if the wound becomes infected. In these cases, wounds may be allowed to heal by second intention (secondary) healing through the granulation and contracture process with a subsequent plan, if necessary, for wound revision. A special circumstance of trauma involves bite injuries, which may be of animal, insect, or human origin. Allowing a bite injury to heal by first-intention healing should be considered carefully because the wound is likely to be contaminated. Although infection may ensue, primary closure is still recommended for these wounds after thorough irrigation and with concomitant antibiotic administration. The antibiotic coverage should be directed at a polymicrobial spectrum including hemolytic streptococci, Staphylococcus aureus, and anaerobes such as Bacteroides. Typically, injectable 1% lidocaine with epinephrine mixed 1:100,000 is adequate to obtain anesthesia for closure. This preparation can be injected with a fine, 27-gauge needle and a control-type syringe. During the procedure, it is often possible to keep the patient comfortable with a small amount of sedation if no contraindication exists. Wound Irrigation Once anesthesia takes effect, the wound should be irrigated to help prevent future infection. If glass, gravel, or other foreign material is suspected to be in the wound, a finger can be used to probe the wound and remove the foreign material. Sometimes the skin is abraded so badly that the area needing to be anesthetized would be too large to safely administer lidocaine to the patient without causing lidocaine toxicity. In some wounds contaminated by tar, as sometimes occurs in motorcycle accidents or other road injuries, administering general anesthesia is the best recommended option for wound manipulation that is comfortable for the patient. Once the wound is thoroughly clean, povidone-iodine, commonly known as Betadine, can be used to create a sterile environment for wound closure. Any small bleeding areas can be handled with a disposable electric cautery or by using individual clamps and suture ties. A severe laceration may sometimes require general anesthesia to properly identify cut nerves and provide a stable condition for operative closure. It is likely that the result will be no worse if an attempt at closure is made, even if the wound eventually becomes infected compared with leaving the wound open to heal by second intention. Special attention must be directed to evaluation of the airway because airway obstruction may develop rapidly after inhalation injury. Specific risk factors for airway compromise include a history of burn injury within a confined space, evidence of soot in the oral cavity, production of carbonaceous sputum, and concomitant facial and body burns. Laboratory evidence, including arterial blood gases and carboxyhemoglobin levels, may further suggest potential airway impairment. If time permits, serial flexible fiberoptic nasolaryngoscopy exams allow for diagnosis of oropharyngeal, true and false vocal fold edema. In management of burn patients, there should be a low threshold for early intubation. First-degree burns involve the epidermis only (eg, sunburn), and clinical findings include erythema. Second-degree or partial-thickness burns involve the epidermis and a portion of the dermis. These burns are extremely painful and present with blistering and open, weeping surfaces of skin. As such, they are characterized as insensate, swollen, and white or gray in color. Extent of burn injury is estimated by the "rule of nines," whereby the head and neck region represents approximately 9% of total body surface area. Inpatient management is universally required for second- or third-degree burns of the face. Early treatment goals involve the prevention of infection via sterile dressings, burn excision, and wound closure if permissible. To attenuate contracture and scar formation, temporary wound cover may be accomplished with cadaver grafts, porcine grafts, and a variety of synthetic skin substitutes. Permanent wound coverage is obtained by split-thickness skin grafts, local flaps, or microvascular free tissue transfer. Microstomia commonly results from perioral facial burns, or thermal burns that occur when small children chew electric cords. Oral splints are available for prevention of microstomia, but the efficacy of these appliances is controversial. Contracture of the eyelid, or ectropion, occurs when the eyelids are everted from the globes following burn injury. Factors that predict the need for intubation in patients with smoke inhalation injury. The successful repair of midface skeletal fractures requires an understanding of the impact of forces on the skeletal buttresses; it also requires a recognition of the weakness patterns common to this buttress system. In general, the midface creates a vertical maxillary dentition and palate height that needs to be maintained if the repair process is to maximize function. Orbital floor fractures known as "blowout" fractures are commonly encountered as isolated fractures. The mechanism of injury for these fractures is usually from direct anterior orbital trauma, such as from a fist or from a ball during a sporting activity. The orbit is made up of buttresses connected by very thin bones that include maxilla, sphenoid, lacrimal, frontal, zygomatic, ethmoid, and palatine bones. The orbital floor is also the roof of the maxillary sinus and has a natural weakness where the second division of the trigeminal nerve traverses it; the bone in this area is quite thin. Sudden anterior pressure on the orbital contents can cause a fracture of the orbital floor, which results in periorbital fat sagging into the maxillary sinus. In some cases, the inferior orbital rim may be involved at the level of the infraorbital foramen, which may also result in numbness in the V2 distribution (ie, the second division of the trigeminal nerve). In this latter scenario, the patient is at risk for late enophthalmos, and repair would be more easily accomplished within a few weeks of the injury rather than months later, when scarring will cause the procedure to be more difficult. It is highly recommended to obtain a baseline ophthalmologic exam of vision acuity and range of motion for all patients with orbital fractures, especially before proceeding with operative repair. The operative technique involves either a subciliary or transconjunctival incision, both of which give access to the orbital periosteum. The orbital contents are then raised out of the fracture line and supported with a titanium plate, cartilage, bone, absorbable plate, or other material. Many permanent orbital implant materials have a long history of use, including Medpore (ie, porous polyethylene), Marlex (ie, polypropylene mesh), silicone, and other materials. Titanium has the advantage of being able to be fixed to bone via screws, which decreases the chance of late migration. Conchal or nasal cartilage is autologous and is therefore a good material for supporting orbital repairs of this type. After the repair is completed, a forced duction test of extraocular motility should be performed to ensure that any entrapment of the extraocular muscles is relieved. Classification and surgical management of orbital fractures: experience with 111 orbital reconstructions. Subunit principles in midface fractures: the importance of sagittal buttresses, soft-tissue reductions, and sequencing treatment of segmental fractures. The horizontal buttress is the nasal root and the vertical buttress is the frontonasal maxillary pillar. Nasoethmoid complex fractures usually require high velocity and a more powerful force in order to be produced compared with isolated nasal fractures or orbital floor fractures. The key physical findings are often severe orbital swelling and ecchymosis with traumatic telecanthus (widening of the intercanthal distance), which gives the impression of widening of the eyes. Because the anterior ethmoid cells have an impact on frontal sinus drainage, patients with severe nasoethmoid complex fractures may require follow-up to ensure that the frontal sinus drainage is physiologically functional.
Medications listed in the Formulary Adjunct chapter have been moved to the Formulary for ease of reference women's health center amarillo tx discount arimidex 1mg with amex. It had been an honor to watch these fine doctors mature and refine their skills since internship menopause 30 symptoms 1mg arimidex with amex. We are grateful to each of them along with their faculty advisors menopause hormones purchase 1mg arimidex mastercard, who selflessly dedicated their time to improve the quality and content of this publication women's health hands purchase 1mg arimidex fast delivery. The Formulary women's health magazine 6 week boot camp generic 1 mg arimidex visa, which is undoubtedly the most popular handbook section breast cancer stage 0 recurrence purchase 1 mg arimidex visa, is complete, concise, and up to date thanks to the tireless efforts of Carlton K. As recent editors, Megan Tschudy, Jamie Flerlage, and Branden Engorn have been instrumental in helping us to navigate this process. Our special thanks go to our friends and mentors, Jeffrey Fadrowski and Thuy Ngo, for your unwavering support and timely reality checks. Standard drug concentrations and smart-pump technology reduce continuous-medication-infusion errors in pediatric patients. Assess pulse: If infant/child is unresponsive and not breathing (gasps do not count as breathing), healthcare providers may take up to 10 seconds to feel for pulse (brachial in infants, carotid/femoral in children). Assess capillary refill (<2 s = normal, 2 to 5 s = delayed, and >5 s suggests shock), mentation, and urine output (if urinary catheter in place). Recognize signs of distress (grunting, stridor, tachypnea, flaring, retractions, accessory muscle use, wheezes). Bag-mask ventilation is used at a rate of 20 breaths/min (30 breaths/ min in infants) using the E-C technique: a. Hook remaining fingers around the mandible (not the soft tissues of the neck), with the fifth finger on the angle creating an E, and lift the mandible up toward the mask. Administer inhaled -agonists: metered-dose inhaler or nebulized albuterol as often as needed. If air movement is still poor despite maximizing above therapy: (1) Epinephrine: 0. Intubation of those with acute asthma is potentially dangerous, and should be reserved for impending respiratory arrest. Upper Airway Obstruction26-29 Upper airway obstruction is most commonly caused by foreign body aspiration or infection. Epiglottitis: Most often affects children between 2 and 7 years, but may occur at any age. Patient is usually febrile, anxious, and toxic appearing, with sore throat, drooling, respiratory distress, stridor, tachypnea, and tripod positioning (sitting forward supported by both arms, with neck extended and chin thrust out). Mild (no stridor at rest): Treat with minimal disturbance, cool mist, hydration, antipyretics, and consider steroids. If unsuccessful, turn infant over and give five chest thrusts (not abdominal thrusts). Status Epilepticus33,34 See Chapter 20 for nonacute evaluation and management of seizures. Dallas: American Heart Association, Subcommittee on Pediatric Resuscitation; 2011. Effectiveness of cricoid pressure in preventing gastric aspiration during rapid sequence intubation in the emergency department: study protocol for a randomised controlled trial. Adverse hemodynamic effects of interrupting chest compressions for rescue breathing during cardiopulmonary resuscitation for ventricular fibrillation cardiac arrest. Noninvasive positive pressure ventilation for the treatment of status asthmaticus in children. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Diphenhydramine and dimenhydrinate poisoning: An evidence-based consensus guideline for out-of-hospital management. In general, 1% lidocaine buffered with sodium bicarbonate is adequate for local analgesia. Do not clean probes with chlorhexidine, isopropyl alcohol, or alcohol-containing cleaners as they will damage the probe. Wipe away the first drop of blood, and then collect the sample using a capillary tube or container. Alternate between squeezing blood from the leg toward the heel (or from the hand toward the finger) and then releasing the pressure for several seconds. After removing tourniquet, attach a syringe and apply gentle negative pressure to withdraw blood for serum sampling. The saphenous veins in the calves, veins in the forearms, antecubital areas, inside of the upper arms, and external jugular veins are areas where ultrasound guidance can help. Puncture: Insert a butterfly needle attached to a syringe at a 30-to 60-degree angle over the point of maximal impulse. Alternatively, pass the needle and catheter through the artery to transfix it, and then withdraw the needle. Apply a sterile dressing and infuse heparinized isotonic fluid (per protocol) at a minimum of 1 mL/hr. Insert the needle into the skin at a 45-degree angle at the midline of the probe near where it contacts the skin. Posterior tibial artery: Puncture the artery posterior to medial malleolus while holding the foot in dorsiflexion. Secure patient, prepare site, and drape according to the following guidelines for sterile technique7: (1) Wash hands. Insert needle at a 30-to 45-degree angle, applying negative pressure to the syringe to locate vessel. For internal jugular and subclavian vessels, obtain a chest radiograph to confirm placement and rule out pneumothorax. Introducer needle enters at the point where external jugular vein crosses posterior margin of sternocleidomastoid and is directed under its head toward sternal notch. With the probe visualizing the vessel transversely, slowly advance the needle and follow the tip of the needle by sliding the probe away from you. The ultrasound can be placed parallel to the vessel to view the guidewire, if desired. Indications: Obtain emergency access in children during life-threatening situations. This is very useful during cardiopulmonary arrest, shock, burns, and life-threatening status epilepticus. In practice, cannulation of the femoral vein should take place distal to the inguinal ligament. If the child is conscious, anesthetize the puncture site down to the periosteum with 1% lidocaine (optional in emergency situations). It is contraindicated in the presence of possible necrotizing enterocolitis or intestinal hypoperfusion. This avoids renal and mesenteric arteries near L1, possibly decreasing the incidence of thrombosis or ischemia. Identify the one large, thin-walled umbilical vein and two smaller, thick-walled arteries. Grasp the catheter 1 cm from its tip with toothless forceps and insert the catheter into the lumen of the artery. Aim the tip toward the feet and gently advance the catheter to the desired distance. Observe for complications: Blanching or cyanosis of lower extremities, perforation, thrombosis, embolism, or infection. Importantly, it courses behind the heart as it descends below the diaphragm posterior to the liver. Correct placement of the catheter will show the catheter tip passing up the descending aorta, appearing behind the liver and terminating adjacent to the diaphragm. Indications: Examination of spinal fluid for suspected infection, inflammatory disorder, or malignancy, instillation of intrathecal chemotherapy, or measurement of opening pressure. Complications: Local pain, infection, bleeding, spinal fluid leak, hematoma, spinal headache, and acquired epidermal spinal cord tumor (caused by implantation of epidermal material into the spinal canal if no stylet is used on skin entry). Locate the desired intervertebral space (either L3-4 or L4-5) by drawing an imaginary line between the top of the iliac crests. Preparation and draping should proceed from this point towards completion of the procedure. If resistance is met initially (you hit bone), withdraw needle to just under the skin surface and redirect the angle of the needle slightly. Send the first tube for culture and Gram stain, the second tube for measurement of glucose and protein levels, and the last tube for cell count and differential. Indications: Evacuation of a pneumothorax, hemothorax, chylothorax, large pleural effusion, or empyema for diagnostic or therapeutic purposes. Complications: Infection, bleeding, pneumothorax, hemothorax, pulmonary contusion or laceration, puncture of diaphragm, spleen, or liver, or bronchopleural fistula. The stopcock is used to stop air flow through the catheter when sufficient evacuation has been performed. It is advised not to completely evacuate chest prior to placement of chest tube to avoid pleural injury. Point of entry is the third to fifth intercostal space in the mid- to anterior axillary line, usually at the level of the nipple (avoid breast tissue). Starting inferiorly at the lower ribs, move the probe cephalad until the pleural effusion is visualized. Confirmation of the effusion space can be performed with the probe placed parallel inside the intercostal space to remove the obscuring effects of ribs. A variation of this process is to identify the site prior to preparation and draping. Attach syringe and stopcock device to remove fluid for diagnostic studies and therapeutic reasons (see Chapter 27 for evaluation of pleural fluid). Indications: Percutaneous removal of intraperitoneal fluid for diagnostic or therapeutic purposes. This view of the abdomen demonstrates ascites (black) with loops of bowel noted deeper. Care must be taken to ensure adequate distance between the bowel wall and abdominal wall prior to marking the site of paracentesis. Therefore, they are often easier to identify with the probe oriented transverse to the spine. If ultrasound is unavailable, insert needle in the midline, 2 cm 3 58 Part I Pediatric Acute Care below umbilicus. Indications: To obtain urine for urinalysis and sterile culture and to accurately monitor hydration status. Caution: Catheterization is contraindicated in pelvic fractures, known trauma to the urethra, or blood at the meatus. In girls, the urethral orifice may be difficult to visualize, but it is usually immediately anterior to the vaginal orifice. Complications: Infection (cellulitis), hematuria (usually microscopic), intestinal perforation. Indications: Evaluation of fluid for the diagnosis of disease, including infectious, inflammatory, and crystalline disease, and removal of fluid for relief of pain and/or functional limitation. Apply the probe in transverse position in the midline of the lower abdomen, positioning it to locate the bladder. This is also useful in the case of patients with a urinary catheter as the catheter is usually visible. The puncture point should be at the posterior margin of the patella in both cases. Cellulitis characteristics on ultrasound (1) Increased edema, tissue may appear slightly darker, and will have distorted, indistinct margins. Abscess Characteristics (1) Dark fluid collection distinct from surrounding tissue (see. C, A black (anechoic) rounded structure is noted in the soft tissue, which is characteristic of a soft tissue abscess. Using hemostats, bluntly widen and undermine the incision to break up any septated or loculated fluid collections. For anterolateral thigh, needle should be at a 45-degree angle to the long axis of the thigh. Deep dermal: For bringing together deeper portions of wounds with dissolving sutures to allow improved approximation and closure of superficial surfaces. In general, bite wounds should not be sutured except in areas of high cosmetic importance (face). Wrap with an elastic bandage to hold molded splint onto extremity in position of function. Child presents with affected arm held at the side in pronation, with elbow slightly flexed. Support the elbow with one hand, and place your thumb laterally over the radial head at the elbow. Grasp the tip of the distal digit and apply longitudinal traction, with the joint typically slipping into place. Alternatively, grasp the distal phalanx and mildly hyperextend to accentuate the deformity while applying longitudinal traction. Splint extends from palmar crease of the hand to mid upper arm along the ulnar side of the forearm and the posterior aspect of the humerus.
Patients with sebaceous carcinoma present with tumors as nodules on the head and neck; most tumors occur on the eyelids menopause longer periods generic 1mg arimidex mastercard. Symptoms of ocular irritation are common and may be confused with blepharitis or chalazion breast cancer quotes and poems generic 1mg arimidex with amex. About 50% of affected patients with tumors larger than 1 cm die; distant metastases occur in viscera and bone women's health center statesville nc generic 1mg arimidex, and orbital invasion may be more common in tumors with pagetoid features menstruation twice in a month discount arimidex 1 mg with visa. Treatment for sebaceous carcinoma is surgical excision; Mohs micrographic surgery using frozen sections followed by rush paraffin sections may optimize local control and tissue conservation menstrual orange blood safe 1 mg arimidex. The role of radiation therapy as a primary treatment for sebaceous carcinoma is less clear womanlog pregnancy discount 1mg arimidex with amex, but improved technology may make this treatment an option when excision is contraindicated or refused. The role of radiation therapy in the management of dermatofibrosarcoma protuberans. Dermatofibrosarcoma protuberans of the head and neck: treatment with Mohs surgery using inverted horizontal paraffin sections. The lesion is characterized histologically by a predominantly radial growth phase with eventual proliferation of malignant cells into the dermis, as well as upward growth that may present as nodularity and ulceration, which denotes the onset of the vertical growth phase. The incidence of cutaneous melanoma continues to increase exponentially and is currently increasing at a rate of about 5% annually. The overall mortality rate per 100,000 persons continues to increase, but survival rates among patients with lower-staged tumors have increased, and the overall cure rates for melanoma exceed 90%. Both an increased incidence and a decreased mortality may be related to an increased awareness of cutaneous melanoma and its early detection and treatment. Although most cases of the disease are sporadic, some show familial patterns and may be associated with dysplastic nevus syndrome, which carries a 100-fold increased lifetime risk for the development of cutaneous melanoma. Other precursor lesions associated with an increased risk of cutaneous melanoma include large congenital nevi and the presence of more than 50 benign acquired nevi. A strong correlation with prior intermittent intense sun exposure exists, and active programs for prevention as well as early detection may ultimately help decrease the incidence. Melanoma of the head and neck can be separated into three general categories: (1) melanoma in situ (ie, lentigo maligna melanoma), (2) superficial spreading melanoma, and (3) nodular melanoma. The neoplasms can be black or variegated in color and are occasionally amelanotic. These tumors show no radial growth phase and are, by definition, invasive at the time of presentation. Lesions suspected to be nodular melanomas should be either biopsied with a deep 3-mm punch or excised with a 2-mm margin. Shave biopsy should not be performed because the precise measurement of the tumor depth will not be possible and valuable staging information will not be accurate. A careful search for ulceration, induration of surrounding tissue, satellite or intransit lesions, and regional adenopathy should be part of the initial examination. Nodular melanomas can become quite large and present significant surgical challenges, both in terms of achieving local control surgically and in reconstructing the defects after removal. Diagnosis the early clinical diagnosis of cutaneous melanoma requires a high index of suspicion based on family history, risk factors, and physical examination, which should include an examination for satellite lesions, the presence of ulceration, and regional nodes. To distinguish benign, pigmented lesions from high-risk lesions, the "A-B-C-D-E" approach to physical diagnosis is useful. This approach consists of observing five criteria: Asymmetric lesions Borders are irregular Color may vary with multiple shades from brown to red-black Diameter > 6 mm Evolving lesions that have shown growth or change A. A characteristically prolonged radial growth pattern is present and may last decades; approximately 0. These lesions are the least common form of melanoma and usually occur on the cheek, nose, or temple in elderly patients. These changes relate to melanoma thickness and ulceration (but not to the level of invasion) that is to be used in all but T1 categories. The number of metastatic lymph nodes and the delineation of clinically occult or microscopic nodes is used in the "N" category of the classification system. Macrometastases are defined as clinically, radiologically, or pathologically detectable nodes or as gross nodal extracapsular extensions. Micrometastases are detected with sentinel lymph node biopsy or elective node dissection. A new convention defines clinical and pathologic staging to incorporate the staging information gained from intraoperative lymph node mapping and sentinel node biopsy. The role of the initial evaluation after the initial diagnosis is related to the presumed stage of disease. Patients who have melanoma in situ or Stage I disease without ulceration or symptoms need no further examination. The role of the surgical margin size is particularly important for the head and neck, where conservation of normal structures and function is a high priority, particularly if the effect of larger margins is not manifested in the outcome. Sentinel lymph node biopsy or elective node dissection, as well as postoperative radiation therapy, other adjuvant treatment, or a combination of these therapies, should be considered. Radiation therapy-Radiation therapy can be used to treat lentigo maligna or in situ disease when surgery is not feasible. Radiation therapy also has been shown effective in decreasing locoregional recurrence postoperatively in patients with extracapsular spread or bulky nodal disease. Melanoma in situ can be excised using a Woods light with a 5-mm margin of clinically normal skin into subcutaneous fat. Mohs micrographic surgery may be beneficial for excising melanoma in situ in certain locations where tissue conservation is of great concern (eg, the eyelid or nose). A variety of multiagent protocols for advanced disease are currently in institutional trials. Primary cutaneous malignant melanoma and its precursor lesions: diagnostic and therapeutic overview. Dermatofibrosarcoma protuberans: treatment with Mohs surgery using inverted horizontal paraffin sections. It is also likely that abnormalities of mucus secretion, in which the olfactory cilia are immersed, could result in a loss of olfactory sensitivity. General Considerations the sense of smell determines the flavor and palatability of food and drink. Along with the trigeminal system, it serves as a monitor of inhaled chemicals, including dangerous substances such as natural gas and smoke, and odors common to everyday life. The loss of smell or a decreased ability to smell affects approximately 1% of people under age 60 and more than half of the population beyond this age. Abnormalities of olfaction include the following: (1) anosmia (absence of the sense of smell); (2) hyposmia (diminished olfactory sensitivity); (3) dysosmia (distorted sense of smell); (4) phantosmia (perception of an odorant when none is present); and (5) agnosia (inability to classify, contrast, or identify odor sensations verbally, even though the ability to distinguish between odorants may be normal). Disorders of the sense of smell are caused by conditions that interfere with the access of the odorant to the olfactory neuroepithelium (transport loss), injure the 232 B. The olfactory system is thus characterized by three important features: (1) the large family of receptor genes exhibits remarkable diversity allowing response to a variety of smells, (2) the receptor proteins exhibit exquisite specificity allowing for odor discrimination, and (3) odor associations are well kept in memory long after the incident that formed the association is forgotten. Etiology Many patients experience olfactory dysfunction due to one or more of the following causes: obstructive nasal and sinus disease, post-upper respiratory infection, cranial trauma, and congenital causes. Aging, exposure to toxins, and idiopathic causes also account for the loss of smell. Nasal obstruction at this area or above it caused by severe mucosal swelling, tumors, nasal polyps, or bony deformities can result in hyposmia or anosmia. In addition, patients often report a loss of sense of smell during an upper respiratory infection; generally, this loss is due to airway obstruction secondary to mucosal swelling. Olfactory ability should improve or return altogether with relief of the obstruction. The degree of olfactory loss is generally associated with two things: the severity of the trauma and the site of cranial trauma. Total anosmia is more likely to occur with occipital traumas; however, frontal blows most frequently cause olfactory loss. Other endocrine disorders can affect smell perception, including Cushing syndrome, hypothyroidism, and diabetes mellitus. Perhaps the most well-known type of congenital anosmia is Kallmann syndrome, an X-linked disorder. The receptor genes are present at more than 25 different human chromosomal locations. Olfactory receptor proteins are G protein-coupled receptors characterized by the presence of seven alpha-helical transmembrane domains. Each olfactory neuron expresses only one, or at most, a few receptor genes, providing the molecular D. Olfactory sensitivity tends to drop sharply in the sixth and seventh decades of life. Anatomically, cellular elements associated with olfaction decrease with age, as does olfactory bulb volume (found at the base of the frontal cortex). In these patients, the most likely mechanism is damage to the olfactory bulb or central olfactory cortex, which results in the loss of olfactory detection and recognition ability. However, because of the widespread degeneration of the olfactory neuroepithelium and intercalation of respiratory epithelium in the olfactory area of adults with no apparent olfactory dysfunction, biopsy material must be interpreted cautiously. Formalin exposure is an example of a toxicity that accumulates over a period of years. Most agents that cause olfactory loss are either gases or aerosols that enter the nose with the respiratory air stream. Patients with depression and schizophrenia may have olfactory losses as part of their illnesses. Although depressed patients do have some altered gustatory ability, the ability to identify odorants is usually normal; when it is not, the olfactory complaints most likely stem from a problem in the central nervous system. It may be that the same chemicals that cause symptoms of depression affect the neural connections between the limbic system and the hypothalamus. Unilateral anosmia is rarely a complaint; it can be recognized only by separately testing smell in each nasal cavity. Anosmic patients usually complain of loss of the sense of taste, even though their taste thresholds may be within normal limits. In actuality, they are complaining of a loss of flavor detection, which is mainly an olfactory function. Step 1: Determining qualitative sensations- the first step in the sensory evaluation is to determine the degree to which qualitative sensations are present. Scratch-and-sniff card-A scratch-and-sniff card that contains three odors to test gross olfaction is commercially available. This test utilizes 40 forced-choice items that feature microencapsulated scratch-and-sniff odors. For example, one of the items reads, "This odor smells most like (a) chocolate, (b) banana, (c) onion, or (d) fruit punch. The presence of serous otitis media suggests the presence of a nasopharyngeal mass or inflammation. A careful nasal examination for nasal mass, clot, polyps, and nasal membrane inflammation is critical. When available, anterior rhinoscopy should be supplemented with endoscopic examination of the nasal cavity and nasopharynx. The presence of telecanthus on the ocular exam may suggest a sinus mass or inflammation. Nasopharyngeal masses protruding into the oral cavity or purulent drainage within the oropharynx may be seen during the oral examination. It is an accurate quantitative determination of the relative degree of olfactory deficit. The average score for total anosmics is slightly higher than that expected on the basis of chance alone because of the inclusion of some odorants that act by trigeminal stimulation. Step 2: Determining the detection threshold- After the physician determines the degree to which qualitative sensations are present, the second step in the sensory evaluation is to establish a detection threshold for the odorant phenylethyl alcohol. Sensitivity for each side of the nose is determined with a detection threshold for phenyl-ethyl methyl ethyl carbinol. Nasal resistance can also be measured with anterior rhinomanometry for each side of the nose. The perversion of the sense of smell may occur as a phase in the recovery process. The receptor cells are present but are hypoplastic, lack cilia, and do not project above the surrounding supporting cells. Occasionally, pituitary adenomas, craniopharyngiomas, suprasellar meningiomas, and aneurysms of the anterior part of the circle of Willis extend forward and damage olfactory structures. These tumors and hamartomas also may induce seizures with olfactory hallucinations, indicating involvement of the uncus of the temporal lobe. Dysosmia, a subjective distortion of olfactory perception, may occur with intranasal disease that partially impairs smell or may represent a phase in the recovery from a neurogenic anosmia. Most dysosmic disorders consist of disagreeable or foul odors, and they may be accompanied by distortions of taste. Differential Diagnosis At the present time, there are no psychophysical methods to differentiate sensory from neural olfactory loss. Head trauma is a more common cause of anosmia in children and young adults, and viral infections are more common causes of anosmia in older adults. Parainfluenza virus type 3 appears to be especially detrimental to human olfaction.
A significant portion of posterior or extensive lesions may also be approached in this manner but may ultimately require an atticotomy or mastoidectomy womens health hotline buy discount arimidex 1mg line. In contrast to acquired cholesteatoma pregnancy recipes arimidex 1 mg without a prescription, congenital lesions result in minimal inflammatory reactions or adhesions between the matrix and the middle ear mucosa pregnancy in weeks order arimidex 1mg on-line. A clear plane can be easily developed between the cholesteatoma and the surrounding mucosa of the middle ear or ossicles pregnancy pillow trusted arimidex 1mg, especially if prior surgeries have not been performed women's health zambia generic 1mg arimidex amex. Evidence of bony erosion in the mastoid on preoperative imaging studies are contraindications to attempted removal via an extended tympanotomy pregnancy 4 weeks 2 days arimidex 1mg with mastercard. A speech reception threshold worse than 30 dB has been defined as an indication for surgery. Classification Historically, congenital malformations of the ear have been divided into major and minor types with the latter limited to the middle ear alone. Children with multisystem syndromes may be at a considerably higher anesthetic risk if there is involvement of the upper airway, heart, lungs, or kidneys. For children in overall good health, the indications, timing, and ideal method of surgical correction remain a source of controversy. The patient should be assessed for a delay in speech acquisition and the presence of cognitive and learning delays. Deferring surgery until at least the age of 5 is associated with a decreased incidence of otitis media, improved patient cooperation, and more sophisticated audiometric testing. Surgery for unilateral disease in the setting of a normal contralateral ear either can be performed at the age of 5 or delayed until the patient is able to participate fully in the decision-making progress. Delaying surgery remains a source of controversy since the beneficial effects of binaural hearing on speech and development are continually being discovered. Finally, amplification with hearing aids, as a transition or an alternative to surgery, should be offered to the patient and family. In addition to this low incidence, other factors make accurate preoperative diagnosis difficult. With the exception of malleus-incus fusion, hypoplasia of the malleus, and middle ear aplasia, the otoscopic examination is unremarkable. Furthermore, audiometric evaluation demonstrates a similarly moderate-to-severe conductive hearing loss that is fixed over time with most anomalies. These factors mandate a high index of suspicion to ensure both an accurate diagnosis and appropriate management. A general examination of the patient is performed to evaluate the overall health and to search for any findings suggestive of a syndrome. Otoscopic examination of patients with anomalies of the malleus or combined ossicular anomalies may demonstrate loss of the tympanic membrane landmarks. Hypoplasia or aplasia of the malleus results from a failure of embryogenesis between weeks 7 and 25. Given the common pharyngeal arch origin, hypoplasia of the malleus is often associated with hypoplasia of the incus. An ossicular replacement prosthesis can be placed at the time of middle ear exploration in these cases. The term "malleus bar" has been used when this bridge connects to the posterior tympanic wall. This anomaly is thought to result from a failure of the resorption and remodeling that occurs during the final stages of stapes development and accounts for up to 20% of all ossicular anomalies. Several crural anomalies have been described, including thin, absent, fused, and angled crura. Laser resection followed by stapes prosthesis replacement is effective in symptomatic crural lesions and columella stapes. The incomplete absorption of mesenchyme may result in bony bridges between the facial canal and either the head or crus of the stapes that result in a symptomatic conductive hearing loss. Equally effective is laser removal of a bony bar that spans the pyramidal eminence and stapes neck in cases of ossified stapedius tendon. Ossicular replacement techniques used for patients with acquired erosion of the incus secondary to chronic otitis media are, similarly, effective for patients with these congenital lesions. Complete agenesis of the ossicles occurs in conjunction with multisystem syndromes (eg, DiGeorge syndrome) and is not amenable to reconstruction. Furthermore, the handle of the malleus is typically fixed to the atretic plate and posterior canal wall. This placement, in combination with the atresia of the external auditory canal, results in a maximal conductive loss. Many management strategies have been proposed for appropriate surgical candidates. The incus-malleus complex may be removed and replaced with a partial ossicular replacement prosthesis. Alternatively, a combination of laser and a drill may be used to enlarge the canal and free the ossicular mass from the atretic plate and canal wall. Finally, the ossicular mass may be disarticulated from the stapes, remodeled, and used for reconstruction. All three ossicles may be fused either as a single mass or at specific articulation points (the malleus handle, the incus long process, or the stapes head). Although the treatment of complete ossicular fusion is limited secondary to fusion to the oval window, lesions involving fusion at single articulation points are amenable to reconstruction with a prosthesis. One third of all anomalies of the stapes are associated with anomalies of the long process of the incus. The incudostapedial joint forms during week 8 of fetal development as the incus precursor migrates to articulate with the future stapedial ring. The fibrous union of this joint results in a conductive hearing loss of approximately 30 dB and may be transmitted in an autosomal dominant fashion. Treatment options include incus removal and prosthesis replacement, stapedectomy, or cartilage interposition. The stapes requires the longest period of embryologic development and therefore has the greatest potential for malformation. In addition, the stapes is derived from both branchial arch and otic capsule precursors, adding to the complexity of the development of this ossicle. Congenital stapes footplate fixation is the most common isolated ossicular anomaly and is thought to result from ossification of a portion of cartilage in the annulus of the oval window. However, outcomes have been mixed, with postoperative cerebrospinal fluid otorrhea and decreased hearing (30%) reported as known complications. Although aplasia of the stapes is rare, multiple forms of hypoplasia that include small or absent crura and small, blob-like stapes have been described. The surgical options include total stapedectomy in cases with a fixed footplate, or replacement with a stapes prosthesis in cases of a mobile footplate. In contrast, isolated hyperplasia of the stapes is often an incidental finding that does not require therapy. Congenital absence of the oval window: radiologic diagnosis and associated anomalies. Failure of the normal association between the primordial oval window niche (the otic capsule) and the developing stapes footplate between the fifth and sixth weeks of development results in aplasia of the oval window and is most commonly associated with anterior displacement of the tympanic segment of the facial nerve. Radiographic imaging may also be used to confirm the presence of normal inner ear structures, determine the anatomy of the facial nerve, and detect any associated ossicular anomalies. Options include hearing aids, vestibulotomy with prosthesis insertion, fenestration and piston insertion above the aberrant facial nerve, or fenestration of the horizontal semicircular canal. Furthermore, the facial nerve and the inner ear are at considerable risk for injury during these surgical approaches. More commonly, the round window position and size may vary without functional consequence. During week 11 of fetal development, a condensation of connective tissue forms at the future site of the round window. This develops into a cartilage ring that prevents ossification of the round window niche. Failure of the development of this ring results in bony obliteration of the primordial niche. Round window aplasia is often associated with stapes ankylosis and a 40-dB conductive hearing loss. When stapedectomy is unsuccessful in reversing this hearing loss, the absence of the round window may be diagnosed in retrospect. Attempts at surgical fenestration have met with poor results and carry a significant risk of sensorineural hearing loss. Non-syndromic cases of round window anomalies are rare, with fewer than 10 reports described Otitis Media Philip D. There is no absolute time period, but, in general, disease that persists for more than 3 months should be considered as chronic. Otitis media associated with cholesteatoma is considered separately in Chapter 50, Cholesteatoma. The normal physiologic functions of the eustachian tube are to (1) maintain the gaseous pressure within the middle ear cleft at a level that approximates atmospheric pressure; (2) prevent reflux of the contents of the nasopharynx into the middle ear; and (3) clear secretions from the middle ear by both mucociliary transport and a "pump action" of the eustachian tube. Both anatomic and functional obstruction of the eustachian tube results in the failure of normal regulation of the middle ear pressure. Anatomic obstruction is most commonly caused by inflammation of the eustachian tube mucosa or extrinsic compression by tumor or large adenoids. Functional obstruction usually occurs as a result of either the failure of the normal muscular mechanism of eustachian tube opening, as seen in cleft palate, or insufficient stiffness of the cartilaginous portion of the eustachian tube, often seen in infants and young children. The more acute angle of the eustachian tube seen in children, compared with adults, may also result in the impaired function of the eustachian tube opening. If the eustachian tube is abnormally patent or short, its normal protective function against the reflux of nasopharyngeal contents is lost. The protective mechanism of breast-feeding has not been clearly demonstrated, but is likely to be related to antibacterial and immunologic benefits conferred by breast milk. Passive smoking results in inflammation of the mucosa of the middle ear cleft as well as impaired mucociliary clearance, which lead to an increased susceptibility to infection. These genetic variations may be related to anatomic and physiologic variations in the eustachian tube. Because the tensor veli palatini muscle lacks its normal insertion into the soft palate, it is unable to open the eustachian tube properly on swallowing. Inflammation of the middle ear mucosa results in an effusion, which cannot be cleared via the obstructed eustachian tube. This effusion provides a favorable medium for proliferation of bacterial pathogens, which reach the middle ear via the eustachian tube, resulting in suppuration. Less frequently identified pathogens include group A streptococci, Staphylococcus aureus, and gram-negative organisms such as Pseudomonas aeruginosa. This finding may occur for a variety of reasons, including (1) antibiotic therapy before tympanocentesis; (2) nonbacterial pathogens (eg, viruses, chlamydia, and mycoplasma); and (3) pathogens that do not proliferate in classic culture conditions (eg, mycobacteria and anaerobic bacteria). Adenoidectomy also has a demonstrable effect, though more modest than that seen with tympanostomy tubes. Otitis externa also presents with otalgia and otorrhea and may be the primary diagnosis, or it may be secondary to the infected discharge from the middle ear. If otalgia is the primary complaint, then referred pain should be considered, particularly when otoscopy reveals a normal tympanic membrane. The common sites of origin of referred otalgia are the teeth and temporomandibular joints. In adults, malignant neoplasms of the pharynx and larynx may present with otalgia as the only symptom. In neonates and infants with a high fever and systemic upset, the possibility of meningitis should be considered. The use of antibiotics is probably beneficial, but there is a trade-off between benefits and side effects. There is no difference demonstrated in recurrence rates or the development of complications among different antibiotics. Older children usually complain of earache, whereas infants become irritable and pull at the affected ear. A high fever is often present and may be associated with systemic symptoms of infection, such as anorexia, vomiting, and diarrhea. Otoscopy classically shows a thickened hyperemic tympanic membrane, which is immobile on pneumatic otoscopy. Further progression of the infective process may lead to the spontaneous rupture of the tympanic membrane, resulting in otorrhea. At this stage, it is often not possible to visualize the tympanic membrane because of the discharge in the ear canal.
Order 1 mg arimidex amex. Women in Business Expo | Day 7.
References