




|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Abhinav Humar, M.D.
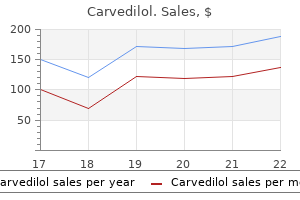
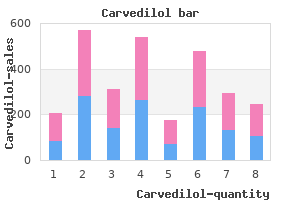
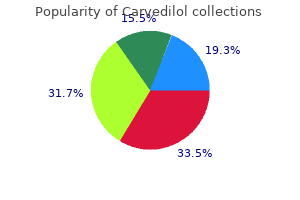
The intertrochanteric osteotomy must be accompanied by extension to achieve the same effect pulse pressure 41 buy carvedilol 25mg otc. The containment treatment must be continued until the femoral head has regrown heart attack history order carvedilol 12.5mg otc, i percentil 95 arteria uterina buy carvedilol 25 mg free shipping. Conservative treatment: abducting braces Abducting braces can be designed according to the following principles: braces with a hip strap and thigh sections held in an abducted position by hinges pulse pressure congestive heart failure buy generic carvedilol 12.5 mg on-line. While the abducting effect is achieved with the first two types, walking with these braces is only possible with flexed knees. With the Ponseti Foot Abduction Bar, on the other hand, walking is almost impossible. Surgical treatment: femoral or pelvic osteotomy the result produced with the abduction brace, namely improved containment, can essentially be achieved by surgical means. Advantages of conservative treatment no hospitalization required no operation risks Good containment is present if nothing spills out of the container 211 3. Even though one automatically tends to think that surgical treatment is more aggressive than conservative treatment, we do not share this view in this particular case. The negative psychological impact on a child resulting from a substantially handicapping 2-year brace treatment can, in our view, be much worse than that associated with a surgical treatment involving a 5-day hospital stay followed by 6 weeks of using crutches. In both cases the lateral section of the femoral head is contained in the acetabulum, while the Salter pelvic osteotomy additionally provides better coverage for the anterior section of the femoral head. This effect can be achieved on the femoral side by adding an extending component to the varization. The former is indicated if the pelvis is not elastic enough to allow sufficient movement of the acetabulum. In certain cases (particularly older children) an operation involving both the femur and pelvis may be advisable [14]. The Salter pelvic osteotomy results in increased pressure in the joint, since the acetabular roof is transferred not just laterally and anteriorly, but distally as well. The psoas muscle is primarily responsible for this increase in pressure, and this effect can be reduced by aponeurotic lengthening of the psoas tendon. It avoids the problems inherent in the intertrochanteric varus osteotomy, does not increase the intraarticular pessure (in contrast with the Salter osteotomy), but is technically more demanding. Improving containment by intertrochanteric osteotomy in a 6-year old boy with lateral calcification and subluxation. Improving containment by triple osteotomy in a 9-year old boy with lateral calcification and subluxation. Improving containment in a case of pronounced subluxation and deformation of the femoral head by concurrent triple osteotomy and intertrochanteric varization osteotomy in an 8-year old boy. Two particular studies on the abduction brace that should be taken very seriously produce a negative answer to this question [46, 49]. However, some studies have also found that abducting braces can be just as effective as surgical treatment [7, 13, 17]. The results were better than spontaneous progression primarily in children over 5 years, and only the anterolateral section of the femoral head was affected (Catterall group I) [11]. The additional relief provided after surgical treatment does not provide any further improvement in the result [6]. In the recently published, aforementioned prospective study, based on the lateral pillar classification only those patients who were over the age of 8 years at the time of onset with a hip in the lateral pillar B group or B/C border group had a better outcome with containment treatment than they did without it. Children who were less than 8 years of age at the time of onset and were not group C had favorable outcomes unrelated to treatment, whereas group C hips in children of all ages frequently had poor outcomes, whether or not they were treated [27]. As already mentioned, one can achieve essentially same result produced by the intertrochanteric osteotomy, in terms of containment, with the pelvic osteotomy according to Salter and the triple osteotomy. In recent years, because of the aforementioned disadvantages, there has been a clear trend away from the intertrochanteric osteotomy towards the triple osteotomy [38]. We ourselves use the latter as the standard containment procedure in children over 7 years of age. For younger patients we perform the intertrochanteric varus osteotomy or the Salter pelvic osteotomy. The latter is particularly useful if the femoral head epiphyseal plate is rather steep or if leg shortening is already present. The overgrowth of the greater trochanter and a Trendelenburg limp that persists for a prolonged period are observed more frequently after an intertrochanteric osteotomy than after pelvic osteotomies [42, 67]. The overall mobility of the hip prior to an osteotomy must be good since it is not improved as a result of the operation and because the femoral head will not be centered properly during the procedure if the hip is not sufficiently mobile. Nowadays, botulinum toxin injection and/or postoperative epidural anesthesia left in place after mobilization for several days are two very efficient ways of improving the range of motion. The inability to abduct properly, particularly after a varus osteotomy, involves the risk of a postoperative adduction contracture with further decentering of the hip. Consequently, the mobility should not be allowed to fall below a critical limit before the operation. Follow-up controls Irrespective of the treatment: Clinical check-ups every 3 months (particularly to examine mobility), possibly also ultrasound examination 213 3. Drug-induced improvement of femoral head circulation the drug iloprost appears to produce a positive effect on bone marrow edema and the vascularization of bone [2], although no controlled studies have yet demonstrated its efficacy in Legg-Calvй-Perthes disease. Treatment of the defect If the femoral head is deformed with a laterally protruding bump and hinge abduction in the older child (generally over 7 years), and if containment of the head is no longer possible, there are two treatment options: resection of the protruding bump, arthrodiastasis, intertrochanteric valgus osteotomy. We have had little and not particularly positive experience of the bump resection. Since the joint cartilage inevitably has to be resected along with the bump, it is not surprising that the condition of the joint is frequently not improved by this procedure. Distraction is applied and the hinge of the distractor is periodically opened to allow movement of the joint [47]. The intertrochanteric valgus osteotomy on the other hand is often an effective procedure [60] (. A questionnaire was sent to all 297 members of the society describing four cases of Legg-Calvй-Perthes disease with 2 x-rays each and a short description of the clinical situation. In both age groups there was one patient with a good range of motion and an x-ray classified Herring A or B, while the other patient had a poor range of motion and an xray classified as Herring C. The members were asked to choose from various treatment options or to describe any other therapy that they would advise in the clinical scenarios. The participants had an average of 20 years of experience in pediatric orthopaedics. There was a consensus, that no operation should be done in a young patient with a good range of motion, and that there should be no weight relief in older patients with a good range of motion. Conservative containment treatment (abduction splint, Petrie cast) and arthrodiastasis was suggested in only very few centers. There was a tendency operate on older patients with a poor range of motion, to provide surgical treatment only when there were subluxation or head at risk signs, and to perform pelvic osteotomies or a combination of pelvic and femoral osteotomies rather than femoral osteotomies alone. Age did not determine the indication for treatment and there was no agreement on the indications for physiotherapy. Treatment in the defect stage with intertrochanteric valgization osteotomy for severe hinge-abduction. Our therapeutic strategy for Legg-Calvй-Perthes disease Our therapeutic strategy for Legg-Calvй-Perthes disease is shown in Table 3. No weight-relieving devices, no abduction splints, crutches only for very severe pain, no total ban on sport! Adekile A, Gupta R, Yacoub F, Sinan T, Al-Bloushi M, Haider M (2001) Avascular necrosis of the hip in children with sickle cell disease and high Hb F: magnetic resonance imaging findings and influence of alpha-thalassemia trait. Aigner N, Petje G, Schneider W, Krasny C, Grill F, Landsiedl F (2002) Juvenile bone-marrow oedema of the acetabulum treated by iloprost. Barwood S, Baillieu C, Boyd R, Brereton K, Low J, Nattrass G, Graham H (2000) Analgesic effects of botulinum toxin A: a randomized, placebo-controlled clinical trial. Farsetti P, Tudisco C, Caterini R, Potenza V, Ippolito E (1995) the Herring lateral pillar classification for prognosis in Perthes disease. Gallistl S, Reitinger T, Linhart W, Muntean W (1999) the role of inherited thrombotic disorders in the etiology of Legg-Calve-Perthes disease. Ghanem I, Khalife R, Haddad F, Kharrat K, Dagher F (2005) Recurrent Legg-Calve-Perthes disease revisited: fake or reality? Hayek S, Kenet G, Lubetsky A, Rosenberg N, Gitel S, Wientroub S (1999) Does thrombophilia play an aetiological role in Legg-CalvePerthes disease? Joseph B, Srinivas G, Thomas R (1996) Management of Perthes disease of late onset in southern India.
Hyperbaric oxygen this treatment modality exposes patients to super-normal oxygen concentrations that cause vasoconstriction blood pressure negative feedback loop cheap 25 mg carvedilol fast delivery, increased arterial oxygen pressures arrhythmia upon exertion discount carvedilol 6.25mg line, stimulation of angiogenesis blood pressure goals chart discount 6.25 mg carvedilol free shipping, fibroblast proliferation and antibiotic synergy (Tibbles and Edelsberg hypertension 16070 order carvedilol 6.25mg overnight delivery, 1996). Hyperbaric oxygen is currently used in the treatment of osteoradionecrosis and carbon monoxide poisoning. Complications include barotrauma, seizures and worsening of congestive heart failure. Animal studies suggest a role in the treatment of chronic wounds and in improving graft and flap survival (Friedman et al. However, a lack of human data, technical sophistication and the complication profile of hyperbaric oxygen therapy limit its clinical application. It is important to inform patients that whenever an incision is made or the full thickness of the skin is injured, there will always be a scar. What is possible is to attempt to make the scar as inconspicuous as possible by obtaining a fine-line scar. This can be difficult to ensure for all patients, however, because several factors determine the final appearance of scars including the skin type and location on the body, the direction in which the wound runs, patient factors such as local and systemic disease, surgical technique, and the amount of tension placed on the closure. There are also unexplained differences between patients that sometimes make scarring different or problematic. Scars on the shoulder and sternum, for example, are frequently hypertrophic or wide compared with eyelid scars, which are commonly inconspicuous fine-line scars. Loss of skin elasticity with ageing produces wrinkling, which makes scars less conspicuous and less prone to widening. In younger individuals, especially growing children, wounds heal faster but the quality of the scar is not as high as in the elderly. Scars frequently appear red and wide and are prone to changes in shape and size as the body grows. Scalp scars in small children therefore need consideration when making incisions or facing closure of a wound. Wounds closed under tension generally lead to less aesthetically pleasing results. Elliptical excisional wounds also close with less pleasing results compared with simple incisional wounds because of the lack of normal tissue between the closed ends. They reflect the natural orientation of collagen fibres in the dermis and are otherwise known as relaxed skin tension lines. These are the same as wrinkle lines seen in older individuals and have a long axis perpendicular to the long axis of the underlying muscles. When a scar crosses the relaxed skin tension lines at a right angle, contraction leads to puckering and a more conspicuous scar. Other techniques employed to make scars less noticeable include hiding them at the junction of aesthetic units. This is a perceptive change that takes advantage of the fact that the eye expects a change in contour at these junctions. Good surgical technique with minimal trauma to skin edges, diligent debridement and ensuring no tension at closure are essential steps toward obtaining a fine-line scar. The latter point is the more significant because even if heavy-gauge sutures are used, prompt removal can prevent unsightly scarring. Different units suggest different time frames for the removal of sutures; however, in general, facial sutures can be removed after 35 days, and after up to 7 days in other areas of the body. Sutures should remain in place for over a week only really for wounds over joints. In many wounds, subcutaneous closure with steri-strips is usually sufficient to prevent dehiscence. A logical progression beginning with P rinci P l es of recons t r u ct iv e s u rgery 15 Free tissue transfer Regional tissue transfer Distant flaps Skin graft Primary closure Local tissue transfer figure 1. It is good practice to use the simplest option that meets the reconstructive requirement in the first instance because it leaves open the opportunity to try more involved treatments should this fail. There are, however, cases in which a specific technique higher up the ladder is more appropriate for a specific indication; under these circumstances, this can be employed directly. For example, local flaps for nasal defects may be preferable to grafts because of better aesthetic results. As mentioned above, the skin provides the aesthetic definition of the body and is also a major contributor to innate immunity, protecting our internal structures from environmental hazards. Maintaining the integrity of the skin is thus crucial for the preservation of health; lack of its maintenance invariably leads to significant morbidity and mortality through infection, heat loss, fluid imbalance and direct damage to internal structures. This practice is believed to date back to ancient Egyptian times, when it was used to treat the living and also to prepare mummies for burial. The decision regarding which technique is used depends on the characteristics of the defect being closed and other circumstances that may affect closure of the wound or the health of the patient as a whole. For example, insertion of skin staples is faster than suturing and is associated with a lower risk of infection and tissue reaction. Whichever technique is used to close a specific wound, the accurate approximation of skin edges without tension leads to minimal scarring. Subdermal wounds are closed in layers with careful suturing to produce a strong and secure closure. The aims of such closure are to eliminate dead space and to provide enough strength to enable wound healing while preventing dehiscence. The strength of closure required varies depending on the function of the particular body area being closed. For example, as the scalp is not particularly mobile or regularly subjected to tension, it does not require as secure a closure as the lower limb. To achieve the additional strength in the latter situation, one might decide to close the individual layers separately, whereas this may not be necessary for closing other types of wounds. Suturing techniques A key principle of suturing is ensuring the skin edges are everted. Everting the wound edges allows the dermal edges (which constitute 95% of the thickness of the skin) to come into contact and heal together. If the wound edges are not sufficiently everted, then the scar will widen and become depressed as the wound heals. Eversion may initially produce a slightly raised closure; however, as healing occurs and the wound spreads, the edge will flatten, leaving the best possible scar. The suturing technique used for individual wounds is important to achieve optimal healing. Simple interrupted sutures this is the most commonly used suturing technique, named because each suture is individually placed and tied. The needle is first introduced into the skin at a 90° angle and then advanced through the dermis and out via the opposite dermal and epidermal layers using a rotational wrist movement. The angle of introduction causes the suture to be wider at its base in the dermal layer than at its entry and exit points in the epidermis. When seen in cross-section, this gives the suture a triangular appearance and leads to eversion of the skin edges. The sutures are usually placed 12 mm from the edge of the wound and approximately 57 mm from each other. Simple interrupted sutures are particularly useful if there is concern about the cleanliness of a wound. If any part of the wound looks suspicious for infection, the relevant sutures can be removed without disrupting the entire closure. Simple continuous suture (over-and-over) this variation of the simple suture can be inserted rapidly. For a desirable result with this technique, the wound edges often need to be approximated to a degree before insertion. Mattress sutures Mattress sutures are useful when eversion of the wound edges may be difficult. Horizontal mattress sutures are frequently used in areas with thick glabrous skin, such as the hands and feet. Vertical mattress sutures are often used where simple sutures are unlikely to successfully produce sufficient eversion of the skin edges.
Order carvedilol 6.25 mg amex. Cirrhosis of the Liver Nursing Care Management Symptoms NCLEX.
There can be significant variability in the relationship between different sites blood pressure medication recall 2015 purchase carvedilol 6.25 mg overnight delivery, and conversions should be done with caution heart attack headache purchase carvedilol 6.25mg on line. It is common for parents to report a subjective fever by palpation without measuring a temperature by thermometry arrhythmia vs afib symptoms generic 12.5mg carvedilol. Palpation by parents has a sensitivity and specificity of about 80% in children older than 3 months arteria umbilical unica pdf buy 12.5mg carvedilol with amex. In infants younger than 3 months, the positivepredictive value of a parent reporting a palpable fever is about 60%, with a negative-predictive value of 90%. For these younger infants, for whom identification of fever carries potentially greater clinical repercussions, parents seem to overestimate the presence of a fever, but they are more accurate when a child is afebrile. In infants who are younger than 3 months (when fever can be more significant clinically), a rectal temperature is the preferred method. Tympanic recordings are much less sensitive in this age group because the narrow, tortuous external canal can collapse, thereby resulting in readings obtained from the cooler canal rather than the warmer tympanic membrane. Hausfater P, Zhao Y, Defrenne S, et al: Cutaneous infrared thermometry for detecting febrile patients, Emerg Infect Dis 14:12551258, 2008. One study of newborns in a warm environment of 80 F found that rectal temperatures in bundled infants could be elevated to more than 38 C, which is the "febrile range. A clinical method that may help to distinguish disease-related fevers from possible environmental overheating is the "abdomen-toe" temperature differential. A foot as warm as the abdomen suggests an overly warm environment, whereas a foot that is cooler suggests fever with peripheral vasoconstriction. Long a doctrine of grandmothers, the suggested association between teething and temperature elevation may have some basis in fact. In one study of 46 healthy infants with rectal temperatures recorded for 20 days before the eruption of the first tooth, nearly half had a new temperature elevation of more than 37. Other studies have shown some statistical association with slight temperature increase. In any event, significantly elevated fever should not be ascribed simply to teething. Occult bacteremia refers to the finding of bacteria in the blood of patients, usually between the ages of 3 and 36 months, who are febrile without a clinically apparent focus of infection. This term should be distinguished from septicemia, which refers to the growth of bacteria in the blood of a child with the clinical picture of toxicity and shock. In trials done after the introduction of the Hib vaccine (1990) but before the introduction of the pneumococcal conjugate vaccine (2000), bacteremia rates for pneumococcus ranged from 1. Children who are incompletely immunized are at higher risk compared with the fully immunized. In the postpneumococcal conjugate vaccine era, rates of false-positive results (contaminants) now exceed true-positive rates. Wilkinson M, Bulloch B, Smith M: Prevalence of occult bacteremia in children ages 3 to 36 months presenting to the emergency department in the postpneumococcal conjugate vaccine era, Acad Emerg Med 16:220225, 2009. Waddle E, Jhaveri R: Outcomes of febrile children without localizing signs after pneumococcal conjugate vaccine, Arch Dis Child 94:144147, 2009. In the case of the conjugate pneumococcal vaccine, 7 vaccine serotypes and 2 cross-reactive serotypes composed the vaccine and accounted for about 80% of invasive pneumococcal disease. The overall incidence of invasive disease still remains well below the prevaccine level. This set of six items of observation and physical signs was designed at Yale to assist in detecting serious illness in febrile children who were younger than 24 months old. Normal (1 point), moderate impairment (3 points), and severe impairment (5 points) scores are given for quality of cry, reaction to parental stimulation, state of alertness, color, hydration, and response to social overtures. Scores of 10 or less correlate with a low likelihood of serious illness, primarily in infants older than 2 months. What is the proper way to evaluate and manage febrile illness in infants who are younger than 60 days? This remains a contentious issue even in the era of the conjugate pneumococcal vaccine. On average, up to 10% of febrile infants who are younger than 2 months have serious bacterial infections (bacteremia, meningitis, osteomyelitis, septic arthritis, urinary tract infection, or pneumonia). The incidence of bacterial meningitis, however, is thought to be declining, in part owing to lower rates in older infants because of vaccinations. Additionally, a well physical appearance does not rule out the presence of bacterial disease because up to 65% of febrile infants with serious bacterial infection may appear well on initial examination. In the past, combinations of clinical and laboratory criteria were developed to identify patients who might be at "low risk" for serious bacterial infection and might be managed as outpatients. One laboratory approach to the outpatient management of the febrile infant (29 to 60 days; temperature! How should older infants and toddlers (3 to 36 months old) with fever and no apparent source be managed? Previously, much of the evaluation that centered on febrile children in this age group dealt with identifying possible occult bacteremia with the intent of using empiric antibiotic treatment to lessen the chance of dissemination to focal complications (particularly meningitis). The most common cause of serious bacterial infection in children with fever without a source is an occult urinary tract infection. Most pediatric infectious disease experts no longer recommend a complete blood count and/or blood culture or any laboratory tests (other than urinalysis and urine culture in certain settings) in the evaluation of a well-appearing febrile infant older than 90 days who has received Hib and pneumococcal vaccines because of the low risk for bacteremia and meningitis. Mahajan P, Stanley R: Fever in the toddler-aged child: old concerns replaced with new ones, Clin Pediatr Emerg Med 9:221227, 2008. Although some clinicians believe that chest radiographs should be performed for all febrile infants who are younger than 2 to 3 months, others reserve this study for infants who have respiratory symptoms or signs, including cough, tachypnea, irregular breathing, retractions, rales, wheezing, or decreased breath sounds. In a study of infants younger than 8 weeks who were admitted with fever, 31% of patients with respiratory manifestations had an abnormal chest radiograph, compared with only 1% of asymptomatic infants. Leukocytosis (>20,000/mL) in febrile (>39 C) patients younger than 5 years increases the likelihood of an "occult pneumonia. Bacterial growth is evident in most cultures of infected blood within 48 hours or earlier. A study from Australia of neonatal blood cultures found that the median time for positivity for group B streptococcus was 9 hours, that for Escherichia coli was 11 hours, and that for coagulase-negative staphylococci was 29 hours. Although 36 to 48 hours is generally sufficient time to isolate common bacteria present in the bloodstream, fastidious organisms may take longer to grow. Therefore, when one suspects anaerobes, fungi, or other organisms with special growth requirements, a longer time should be allowed before concluding that a culture is negative. In these patients, the most significant concern is serious systemic bacterial infection, particularly meningococcemia. Another study found that five physical findings, if any were present, increased the likelihood of invasive disease: ill appearance, nuchal rigidity, purpuric skin hemorrhages, universal distribution, and skin hemorrhages larger than 2 mm. Important features of the evaluation are as follows: n History: Elicit information about exposures, travel, animal contacts, and immunizations. The three major categories for pediatric patients are infections, collagen-vascular diseases. A large number of cases have no identifiable cause, and the fever resolves without explanation. As a general rule, in children younger than 6 years, the most common causes involve respiratory or genitourinary tract infections, localized infections (abscess, osteomyelitis), juvenile rheumatoid arthritis, and, infrequently, leukemia. Adolescents, on the other hand, are more likely to have tuberculosis, inflammatory bowel disease, another autoimmune process, or, infrequently, lymphoma. A complete and detailed history is key, with particular attention to possible exposures, including animals, unpasteurized milk (Yersinia or Campylobacter), uncooked poultry, ticks, pica, or dirt ingestion (possible Toxocara or Toxoplasma), rabbits (Tularemia), mosquitoes, stagnant water, and reptiles (Salmonella). After performing a thorough physical examination, one should avoid indiscriminately ordering a large battery of tests. Laboratory studies should subsequently be directed as much as possible toward the most likely diagnostic possibilities. Predictable periodic fever is a cardinal feature of a small number of autoinflammatory disorders, which are thought to be due to primary dysregulation of the innate immune system and may involve mutated proteins. New York City Pediatric Surveillance of Disease Consortium, Pediatr Infect Dis J 20:511517, 2001. In another study conducted in Africa, treatment with nevirapine administered intrapartum to the mother (200 mg at the onset of labor) and postnatally to the infant (2 mg/kg at 72 hours of life or time of discharge) resulted in a 47% decrease in the rate of transmission.
All labour wards should have local guidelines for the management of severe preeclampsia and eclampsia pulse pressure nhs purchase carvedilol 6.25mg otc. General anaesthesia may be particularly hazardous in some patients blood pressure ranges for males purchase carvedilol 6.25mg fast delivery, and additional precautions should be taken to prevent hypertensive peaks during intubation and extubation arteria gallery carvedilol 25 mg fast delivery. Management of severe preeclampsia blood pressure and alcohol 25mg carvedilol for sale, throughout the peripartum period, should be directed towards: 1. A number of different methods of controlling blood pressure prior to delivery have been described. The care with which blood pressure is monitored and regulated is probably of more importance to maternal and fetal welfare than the precise method of control. The majority of patients will already be receiving oral methyldopa from the obstetrician. This has the dual therapeutic advantages of providing both vasodilatation and analgesia in preeclampsia, provided that no coagulation defect is present. Platelet count should be >100 Ґ 109 l1, and the prothrombin time and partial thromboplastin time normal. E Eclampsia and severe preeclampsia 160 Medical disorders and anaesthetic problems 3. This should take place synchronously, preferably using plasma protein fraction or a colloid. Prevention of vasoconstriction and restoration of blood volume has the additional benefit of improving renal function and uteroplacental blood flow. Patients with impaired conscious levels are particularly at risk, and this has, in part, influenced the decrease in the use of heavy sedation. For Caesarean section, there has been a move towards spinal anaesthesia as the technique of choice, because of the improvement in quality of anaesthesia and onset time (Sharwood-Smith et al 1999). Some feel that epidural anaesthesia permits an incremental technique; this carries less risk of the sudden haemodynamic changes that are produced by spinal anaesthesia (Howell 1998). In the very severe case, or if regional anaesthesia is contraindicated, general anaesthesia may be required, but carries additional risks. A careful technique should aim to modulate the hypertensive peaks provoked by intubation and extubation, and to prevent sudden uncontrolled reductions in blood pressure. It has been suggested that drugs that will help modify the hypertensive response to intubation should be given before induction. As yet, there appears to be no technique that guarantees protection in every patient. The following drugs have been used: a) Lidocaine 1 mg kg1 iv, prior to induction, to reduce haemodynamic responses. It prevented intracranial hypertension during tracheal suction in comatose head injury patients (Donegan & Bedford 1980). Magnesium therapy should be initiated without delay to prevent recurrence of fits (Brodie & Malinow 1999). If a convulsion is not associated with hypertension and either oedema or proteinuria, or if the history and signs are atypical, then other causes must be eliminated. If an eclamptic patient remains unconscious 46 h postpartum, neurosurgical advice should be sought. It has been suggested that the combination of diffuse white matter oedema and basal cisternal effacement is an indication for intracranial pressure monitoring (Richards et al 1986). In the severe case, intensive monitoring and treatment should continue for 2472 h. Anthony J, Rush R 1998 A randomised controlled trial of intravenous magnesium sulphate versus placebo. Department of Health 1998 Report on Confidential Enquiries into Maternal Deaths in the United Kingdom 19941996. The Eclampsia Trial Collaborative Group 1995 Which anticonvulsant for women with eclampsia? Howell P 1998 Spinal anaesthesia in severe preeclampsia: time for reappraisal, or time for caution. Schindler M, Gatt S, Isert P et al 1990 Thrombocytopenia and platelet functional defects in pre-eclampsia: implications for regional anaesthesia. Sharwood-Smith G, Clark V,Watson E 1999 Regional anaesthesia for caesarean section in severe preeclampsia: spinal anaesthesia is the preferred choice. Umo-Etuk J, Lumley J, Holdcroft A 1996 Critically ill parturient women and admission to intensive care. Many different subtypes have been identified, each showing a wide spectrum of effects, from mild to severe. There have been recent advances in understanding of the genetic and molecular abnormalities of the variants (Pope 1991), and a new classification has recently been proposed (Beighton et al 1998). Detailed descriptions of each type are beyond the scope of this book; however, for further information, several references may be consulted (Pope et al 1988, Anstey et al 1991, Pope 1991). The clinical picture is one of multiple skin, connective tissue, and musculoskeletal abnormalities. Anaesthesia may be required for joint dislocations, vascular or visceral rupture, and surgery may be complicated by abnormal haemorrhage. The whole group is characterised by a hyperextensible and sometimes fragile, soft skin, hypermobile joints, and a tendency to bruise and bleed without definite coagulation abnormalities. Pregnancy carries a 25% mortality, and the complications of surgery can be disastrous. The commonest causes were arterial aneurysms (50%), arterial rupture (38%), and carotidocavernous fistula (24%). A variety of haemostatic defects were reported in a study of 51 patients (Anstey et al 1991). Although the majority gave a history of bruising, or a bleeding tendency, only 17. The remainder had either mild abnormalities of doubtful significance, or no abnormality at all. Thus, the bleeding and bruising that occurs must be related to structural abnormalities in the collagen and blood vessels, rather than coagulation defects. Even in the absence of subluxation, overall hypermobility of the cervical spine was seen in ten patients. Displacement of the cannula from a vein, and consequent venous extravasation, may remain undetected. Elective repair of an aortic aneurysm was complicated by acute myocardial ischaemia and ventricular tachycardia 163 Anaesthetic problems 1. Spontaneous perforation of a viscus, particularly the colon, may be the first event leading to the diagnosis (Sparkman 1984). Perforation of the superior vena cava occurred during digital angiography (Driscoll et al 1984). In type I disease (3050% of cases), they were associated mainly with tissue laxity, and included vaginal lacerations, abdominal herniae, ante- and postpartum haemorrhage, joint subluxations, and bruising, but none of these complications was associated with death. Spontaneous pulmonary artery rupture caused exsanguination during the seventh month of pregnancy (Pearl & Spicer 1981). Intrapartum deaths have resulted from aortic, uterine, and vena caval rupture (Rudd et al 1983). Death occurred secondary to a postpartum haemorrhage in a patient with normal coagulation tests (Dolan et al 1980). Widespread bleeding from fragile vessels and a ruptured splenic artery aneurysm were found at exploratory laparotomy. Postpartum deaths have resulted from spontaneous rupture of the aorta on day 1 (Rudd et al 1983), day 5 (Snyder et al 1983), and at an unspecified time (Barabas 1972), and renal artery rupture on day 6 (Peaceman & Cruikshank 1987). Reduced depth and duration of anaesthesia probably results from the looseness of the connective tissue. If the condition is suspected and time permits, genetic advice should be obtained to assess the type and severity. Particular care should be taken to avoid tissue trauma or jaw dislocation when tracheal or nasogastric tubes are inserted. During artificial ventilation, low airway pressures should be used to reduce the risk of a pneumothorax. If conduction defects are present, the temporary insertion of a pacemaker should be considered. If this is declined, delivery by elective Caesarean section at 32 weeks has been recommended (Lurie et al 1998), and close observation for signs of vascular or bowel rupture maintained in the postpartum period.
References