


|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Masao Hayashi, MD
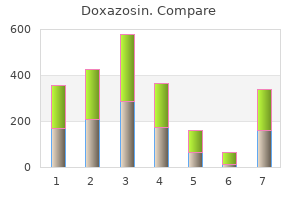
Yellow arrow indicates gas in the biliary ducts system gastritis type a and b purchase 2mg doxazosin mastercard, which occurred after gallstone passage in this patient gastritis diet 21 buy doxazosin 4 mg with mastercard. Free air in the abdomen can be localized under the diaphragm or in the flank in viscus perforations as seen in upright chest films or decubitus views respectively gastritis cystica profunda definition 4 mg doxazosin amex. It is important to know the history when calling free air since it is to be expected after abdominal surgery or intraperitoneal endoscopy gastritis long term order 2mg doxazosin overnight delivery. Also occasionally air can be discovered superimposed between the liver and diaphragm that is not extraluminal but instead within an inter- positioned loop of bowel. When that occurs it may be necessary to obtain additional imaging to exclude a perforated hollow viscus. Yellow arrow points to the anterior leaf of the right hemidiaphragm, which has an eventration. Free air would layer out and since haustral markings are evident, the diagnosis of superimpositioned bowel between diaphragm and the dome of the liver can be made with confidence, at least in this case. Yellow arrow points to an abnormal accumulation of gas representing free air under the diaphragm in this patient with a perforated duodenal ulcer. Image courtesy of Netmedicine Medical Photographic Library via the Internet 57 Diffuse free air in the peritoneal cavity outlines the peritoneal reflections if the film is a flat plate only and is often said to give the appearance of a football effect if the pneumoperitoneum is not under tension. In that case the falciform ligament may be outlined as the "laces" of the "football" (air) which outlines the entire abdominal cavity. Although the football sign of free air is not entirely rare, it is not common either since most cases of pneumoperitoneum are diagnosed by an upright film of the chest or a lateral decubitus film of the abdomen. Figure 75 shows a pneumoperitoneum under tension in an infant with a perforated hollow viscus. Abdominal organs are compressed by free air under tension in this infant with a perforated gut. Gas patterns in the abdomen may offer specific signs to the astute clinician/radiologist too. It occurs when the leading edge of the intussusceptum projects into a pocket of gas as seen in figure 76. Another sign associated with intussuception is not really part of the gas pattern, but can be recognized if you are clinically suspicious and look for it. It is called a target sign and is the result of layers of peritoneal fat surrounding and within the intussusepted bowel, which is water density. Red arrow points to a classic crescent sign in a child with ileocolic intussusception. This patient also has a crescent sign that is obscured by adjacent bowel gas (yellow arrow). If, for example, the patient is guarding the right side of the abdomen as occurs with acute appendicitis or cholecystitis, the right psoas muscle will be contracted and thus not as sharply outlined as the left. In cases of retroperitoneal hemorrhage or retroperitoneal fibrosis, the psoas shadows may disappear altogether. In this case retroperitoneal hemorrhage (water density blood) silhouettes out the right psoas margin. Note the normal renal outlines in figure 80 as opposed to the patient with horseshoe kidneys in figure 81. In the above example, we have outlined the kidneys in the second part of the figure, so that you can test your observation in this patient with unprepared bowel. Even the experienced radiologist will often be unsure of their significance however, and it frequently takes additional imaging to exclude pathology. Note the similarity between the patient with a "normal" lobulated kidney vs the patient with renal pathology in the next illustrations. The lobulations may be the result of columns of Bertin or possibly the result of cortical parenchymal loss due to infarcts or previous bouts of pyelonephritis. A good history would be necessary to evaluate their current importance, but the lobulations are likely of no clinical significance. By the way- the right kidney in this patient is in an ectopic location in the pelvis and not visible in the coned-downed films to the left. Yellow arrow points to a bump on the left kidney of a patient that is more serious-this time a renal carcinoma as indicated by the neovascularity shown in the accompanying angiogram in Figure 85b (below). However, if it is seen to be in a lower position than the right kidney, that is a red flag to exclude displacement by either an enlarged spleen or some other retroperitoneal or intraperitoneal mass. Blue outlined arrow points to the lateral margin of the left kidney, which is seen to be in a lower position than the right kidney (red outlined arrows). This finding is a red flag to look for an enlarged spleen or other mass displacing the left kidney. The edge of the liver is also usually easily demarcated by the contrast of a water density organ bordered by peritoneal fat or gas filled bowel. The liver edge can also be silhouetted out by ascitic fluid and an enlarged liver can displace bowel inferiorly and to the left. If ascitic fluid is present the edge of the liver may disappear due to the silhouette sign. Note the spleenomegally and displaced left kidney in figure 86 on the previous page. The preperitoneal fat lines (the fourth item on the checklist) are thin lines of fat that outline the peritoneal reflections as demonstrated in figure 88. We have deliberately manipulated brightness and contrast in this image to demonstrate the band of fat density (red arrow) along the lateral margins of the abdomen. When fluid such as ascities or blood is present in the peritoneal cavity, the bowel gas is usually displaced away from the fat line. This phenomenon is called by radiologists "widening of the flank stripe" or " displacement of the fat line". Notice the increased distance between the preperitoneal fat (yellow arrows) and the edge of gas-filled bowel (red arrows) in this patient with ascities. Calcifications in the abdomen, the fifth item on the checklist, can be "Aunt Minnies" such as is seen in figure 90 in a patient with gallstones, or in figure 91 in a patient with a staghorn renal calculus. The red outlined arrow indicates a classic staghorn renal calculus in this "Aunt Minnie". Black arrows point to thin lines of calcium deposit in this patient with abdominal aortic aneurysm. Look for aortic and other vascular calcifications as a part of your routine in evaluating all abdominal films. Splenic artery aneurysms or pancreatic calcifications are another couple of "Aunt Minnies". More frequently, however, the student will be called on to search for a ureteral stone in a patient with renal colic or flank pain. See figure 93 for typical pancreatic calcifications (the location gives them away). Red outlined arrow points to large clusters of punctate calcifications in the location of the body of the pancreas consistent with chronic pancreatitis. The final item on the major checklist for the abdomen is the bony skeleton, and the same rule applies as it did for the chest, i. Just for practice see if you can spot the bony abnormality or abnormalities in figures 94-100 before reading the labeled answers. The white arrows indicate abscess formation in both psoas muscles in this child with spinal tuberculosis. Ignore the high contrast (white bone) in this reproduction and concentrate on cortical outlines. Note the loss of definition of the posterior iliac crest (curved red outlined arrow) due to bone destruction in this patient with a plasmacytoma. I am reminded of the day my youngest son asked me "what was it like in the olden days Dad Well in the "olden days" of radiology I can remember as a resident sitting in front of a view box for hours on end with a real skull in my hands and the standard skull views in front of me just to learn the radiographic anatomy. Another one of the few measurements still valid to help you decide whether or not the skull size in an infant or child is normal is the cranial-facial index.
Abdominal radiographs typically show dilated airfilled loops of proximal bowel with no air in the rectum gastritis and ulcers order doxazosin 1 mg on-line. Contrast enema may be required to rule out other diagnoses such as meconium plug gastritis symptoms in elderly order doxazosin 4mg amex, meconium ileus gastritis diet wiki cheap doxazosin 1 mg free shipping, and Hirschsprung disease gastritis diet nz cheap doxazosin 4mg visa. Post-op complications include anastomotic leak, stenosis at the site of anastomosis, and short gut syndrome. Mortality is about 10% (90% survival) with prematurity, associated anomalies, infection and short gut syndrome as major contributors to mortality. Midgut volvulus is one of the most serious emergencies during the newborn period since a delay in diagnosis and subsequent gangrene of the midgut is almost uniformly fatal. The mass may extend into the scrotum and will enlarge with increased intra-abdominal pressure (crying or straining). Incarcerated hernias in children can rapidly evolve into strangulation and gangrene of hernia contents. Intestinal Atresia Surgical consultation should be immediately obtained when the diagnosis is suspected. A few hours may be the difference between a totally reversible condition and death (loss of the entire midgut). Small bowel atresia is a congenital occlusion of the intestinal lumen secondary to an intrauterine mesenteric vascular occlusion that causes a complete obstruction. The most common associated conditions are cystic fibrosis, malrotation, gastroschisis, along with low birth weight and multiparity. Intestinal atresia has also been associated with maternal smoking and cocaine use. Diagnosis of intestinal atresia usually is made soon after birth, within the first 1-2 days. Radiographs of the abdomen show bowel loops of variable sizes with a soapbubble appearance of the bowel contents. Contrast enema typically demonstrates a microcolon with inspissated plugs of meconium in the lumen. Definitive repair of a persistent cloaca is a serious technical challenge and should be performed in specialized centers by pediatric surgeons and urologists. Under fluoroscopic control, Gastrografin and water is infused into the rectum and colon. This usually results in a rapid passage of semiliquid meconium that continues for the next 24 to 48 hours. They occur exclusively in females and are the most complex of anorectal malformations. A persistent cloaca (Latin for "sewer") is the confluence of the rectum, vagina, and urethra into one common channel. A persistent cloaca can be diagnosed on physical examination that shows a single perineal orifice. Diagnosing a persistent cloaca correctly is vital because 50% of infants have hydrocolpos and 90% of babies have associated urological problems. In this situation, placement of a temporary tourniquet around the base of the tumor may be a lifesaving intervention that allows the child to make it to the operating room. The prognosis is dependent on presence of malignancy and the ability to completely resect the tumor. Growing evidence suggests that families of children with lifethreatening and chronic conditions benefit from palliative care and that earlier discussions and initiation can improve symptom management and quality of life. This statement was reaffirmed in 2007, with a policy statement in 2013 enhancing these concepts. Improved professional and social support for families in need of palliative care 5. Continued improvement of pediatric palliative care through research and education Palliative care includes pain/symptom control and management, focusing on enhancing quality of life, emphasizing the assessment and treatment of the body, mind, and spirit to prevent suffering for children and families living with life-threatening or terminal conditions. Complimentary and concurrent components to care Palliative Care in the Hospital Setting Palliative care provided in the tertiary hospital setting is best coordinated through the use of an interdisciplinary palliative care team which includes a physician, nurse and/or nurse practitioner, social worker, spiritual advisor and a child life therapist, and may include a family advocate, clinical pharmacist, dietician, bioethicist, and psychiatrist or psychologist. Because palliative care patients receive interventions from such diverse disciplines, it is important that the primary care physician/team coordinate these efforts. To obtain a consultation, please call the main Neonatology Service number, 832-826-1380. Perinatal Palliative Care Consultations are also available at Ben Taub General Hospital through an interdisciplinary team. Most are done while an expectant mother is admitted and are part of her prenatal consult, which is obtained by calling 713873-9210. A grimace may be characterized by brow lowering, eyes squeezed shut, deepening naso-labial furrow, or open lips and mouth. It is important to be able to recognize and treat all types of pain, including acute pain, chronic pain, recurring pain, procedurerelated pain, and end-of-life pain. Physiologic indicators such as vital sign changes, or behavioral indicators such as facial grimacing, may not be as reliable or may be absent in a chronically or critically ill infant. Characteristics of crying, oxygen requirement, changes in vital signs, facial expression, and sleep state are scored. To achieve adequate analgesia/sedation, medications optimally should be scheduled or given by continuous infusion with intermittent bolus doses as needed in order to avoid fluctuations in blood levels and breakthrough pain or discomfort. In addition, infants should always receive a bolus dose of narcotic or sedative prior to starting or increasing the infusion rate. Intranasal administration is an alternative option for patients who do not have intravenous access. It provides pain relief, elicits a sense of euphoria and promotes histamine release, which results in vasodilatory properties. These properties may decrease venous return, thereby decreasing cardiogenic pulmonary vascular congestion and resultant respiratory distress. Morphine may be less tolerance inducing than the synthetic opioids, given its longer half-life and therefore, should not have to be titrated up as quickly as the synthetic opioids. If a patient is habituated on an opioid infusion, the hourly dose of the infusion can be used for bolus dosing. These agents have specific anxiolytic effects in addition to sedative effects but do not provide pain relief to the patient. Sedatives - Benzodiazepines Habituated Patients If adequate sedation is difficult to achieve in a narcotic or benzodiazepine resistant patient, consultation with the Clinical Pharmacy Specialist or Anesthesia/Pain Management Service should be considered. Alternative Route Medications In the patient who does not have intravenous access, a combination of oral morphine and chloral hydrate may be used. Intranasal medications may also be given Intransal administration of fentanyl and midazolam has been found to be effective in pediatric palliative care. Repeat doses should be used with caution due to accumulation of drug and metabolites. Please see pharmacological management at End-of-life for details specific to therapy focusing on that time period of palliative care.
Patients who have been previously maintained on 20 mg or more of prednisone (or its equivalent) may be most susceptible gastritis diet 6 small order doxazosin 4 mg with mastercard, particularly when their systemic corticosteroids have been almost completely withdrawn gastritis icd 9 code generic 2 mg doxazosin otc. During periods of stress or a severe asthma attack gastritis mayo clinic 4mg doxazosin free shipping, patients who have been withdrawn from systemic corticosteroids should be instructed to resume oral corticosteroids (in large doses) immediately and to contact their physicians for further instruction gastritis weight loss doxazosin 1mg lowest price. These patients should also be instructed to carry a warning card indicating that they may need supplementary systemic corticosteroids during periods of stress or a severe asthma attack. Prednisone reduction can be accomplished by reducing the daily prednisone dose by 2. In addition, patients should be observed for signs and symptoms of adrenal insufficiency, such as fatigue, lassitude, weakness, nausea and vomiting, and hypotension. During withdrawal from oral corticosteroids, some patients may experience symptoms of systemically active corticosteroid withdrawal. A relationship between plasma levels of fluticasone propionate and inhibitory effects on stimulated cortisol production has been shown after 4 weeks of treatment with fluticasone propionate inhalation aerosol. Particular care should be taken in observing patients postoperatively or during periods of stress for evidence of inadequate adrenal response. It is possible that systemic corticosteroid effects such as hypercorticism and adrenal suppression (including adrenal crisis) may appear in a small number of patients who are sensitive to these effects. Upper airway symptoms of laryngeal spasm, irritation, or swelling, such as stridor and choking, have been reported in patients receiving fluticasone propionate and salmeterol inhalation powder. Although such effects are uncommon after administration of salmeterol at recommended doses, if they occur, the drug may need to be discontinued. Fatalities have been reported in association with excessive use of inhaled sympathomimetic drugs. Patients with major risk factors for decreased bone mineral content, such as prolonged immobilization, family history of osteoporosis, postmenopausal status, tobacco use, advanced age, poor nutrition, or chronic use of drugs that can reduce bone mass. Of those enrolled, 108 subjects (72 males and 36 females) were followed for the entire 3 years. In this trial there were 7 non-traumatic fractures reported in 5 subjects treated with fluticasone propionate and salmeterol inhalation powder and 1 non-traumatic fracture in 1 subject treated with salmeterol. Conclusions about cataracts cannot be drawn from this trial because the high incidence of cataracts at baseline (61% to 71%) resulted in an inadequate number of subjects treated with fluticasone propionate and salmeterol inhalation powder 500 mcg/50 mcg who were eligible and available for evaluation of cataracts at the end of the trial (n = 53). The incidence of newly diagnosed glaucoma was 2% with 9 fluticasone propionate and salmeterol inhalation powder 500 mcg/50 mcg, 5% with fluticasone propionate, 0% with salmeterol, and 2% with placebo. Some of these patients have clinical features of vasculitis consistent with Churg-Strauss syndrome, a condition that is often treated with systemic corticosteroid therapy. These events usually, but not always, have been associated with the reduction and/or withdrawal of oral corticosteroid therapy following the introduction of fluticasone propionate. Physicians should be alert to eosinophilia, vasculitic rash, worsening pulmonary symptoms, cardiac complications, and/or neuropathy presenting in their patients. A causal relationship between fluticasone propionate and these underlying conditions has not been established. Doses of the related beta2-adrenoceptor agonist albuterol, when administered intravenously, have been reported to aggravate preexisting diabetes mellitus and ketoacidosis. The decrease in serum potassium is usually transient, not requiring supplementation. Clinically significant changes in blood glucose and/or serum potassium were seen infrequently during clinical trials with fluticasone propionate and salmeterol inhalation powder at recommended doses. The average duration of exposure was 60 to 79 days in the active treatment groups compared with 42 days in the placebo group. Adverse Reactions with Fluticasone Propionate and Salmeterol Inhalation Powder with 3% Incidence and More Common than Placebo in Adult and Adolescent Subjects with Asthma Fluticasone Fluticasone Propionate Propionate and and Fluticasone Fluticasone Salmeterol Salmeterol Propionate Propionate Inhalation Inhalation 100 mcg 250 mcg Powder Powder (n = 90) (n = 84) 100 mcg/50 250 mcg/50 % % mcg mcg (n = 92) (n = 84) % % 27 13 7 4 5 1 4 2 3 12 21 10 6 5 2 4 4 8 6 13 29 7 7 6 2 2 4 1 0 14 25 12 8 1 4 2 10 2 0 8 Adverse Event Salmeterol 50 mcg (n = 180) % Placebo (n = 175) % Ear, nose, and throat Upper respiratory tract infection Pharyngitis Upper respiratory inflammation Sinusitis Hoarseness/dysphonia Oral candidiasis Lower respiratory Viral respiratory infections Bronchitis Cough Neurology Headaches Gastrointestinal Nausea and vomiting Gastrointestinal discomfort and pain Diarrhea Viral gastrointestinal infections Non-site specific Candidiasis unspecified site Musculoskeletal Musculoskeletal pain 19 8 8 3 <1 0 6 2 3 10 14 6 5 4 <1 0 3 2 2 7 4 4 4 3 6 1 2 0 3 0 2 3 4 2 2 1 1 1 1 2 1 1 1 2 3 0 1 4 0 1 4 2 1 5 3 3 11 the types of adverse reactions and events reported in Trial 3, a 28-week non-U. Additional Adverse Reactions: Other adverse reactions not previously listed, whether considered drug-related or not by the investigators, that were reported more frequently by subjects with asthma treated with fluticasone propionate and salmeterol inhalation powder compared with subjects treated with placebo include the following: lymphatic signs and symptoms; muscle injuries; fractures; wounds and lacerations; contusions and hematomas; ear signs and symptoms; nasal signs and symptoms; nasal sinus disorders; keratitis and conjunctivitis; dental discomfort and pain; gastrointestinal signs and symptoms; oral ulcerations; oral discomfort and pain; lower respiratory signs and symptoms; pneumonia; muscle stiffness, tightness, and rigidity; bone and cartilage disorders; sleep disorders; compressed nerve syndromes; viral infections; pain; chest symptoms; fluid retention; bacterial infections; unusual taste; viral skin infections; skin flakiness and acquired ichthyosis; disorders of sweat and sebum. Pediatric Subjects Aged 4 to 11 Years: the safety data for pediatric subjects aged 4 to 11 years is based upon 1 U. Common adverse reactions (3% and greater than placebo) seen in the pediatric subjects but not reported in the adult and adolescent clinical trials include: throat irritation and ear, nose, and throat infections. Laboratory Test Abnormalities: Elevation of hepatic enzymes was reported in 1% of subjects in clinical trials. The elevations were transient and did not lead to discontinuation from the trials. In addition, there were no clinically relevant changes noted in glucose or potassium. In the 6-month trial, a total of 723 adult subjects (266 females and 457 males) were treated twice daily with fluticasone propionate and salmeterol inhalation powder 250 mcg/50 mcg, fluticasone propionate inhalation powder 250 mcg, salmeterol inhalation powder, or placebo. In this trial, 70% of the subjects treated with fluticasone propionate and salmeterol inhalation powder reported an adverse reaction compared with 64% on placebo. The average duration of exposure to fluticasone propionate and salmeterol inhalation powder 250 mcg/50 mcg was 141. Overall Adverse Reactions with Fluticasone Propionate and Salmeterol Inhalation Powder 250 mcg/50 mcg with 3% Incidence in Subjects with Chronic Obstructive Pulmonary Disease Associated with Chronic Bronchitis Adverse Event Fluticasone Propionate Salmeterol 12 Fluticasone Propionate and Salmeterol Inhalation Powder 250 mcg/50 mcg (n = 178) % Ear, nose, and throat Candidiasis mouth/throat Throat irritation Hoarseness/dysphonia Sinusitis Lower respiratory Viral respiratory infections Neurology Headaches Dizziness Non-site specific Fever Malaise and fatigue Musculoskeletal Musculoskeletal pain Muscle cramps and spasms 10 8 5 3 6 16 4 4 3 9 3 250 mcg (n = 183) % 50 mcg (n = 177) % Placebo (n = 185) % 6 5 3 8 4 11 <1 3 2 8 3 3 4 <1 5 3 10 3 0 2 12 1 1 7 0 3 3 12 2 3 3 9 1 In the two 1-year trials, fluticasone propionate and salmeterol inhalation powder 250 mcg/50 mcg was compared with salmeterol in 1,579 subjects (863 males and 716 females). In this trial, 88% of the subjects treated with fluticasone propionate and salmeterol inhalation powder and 86% of the subjects treated with salmeterol reported an adverse event. The most common events that occurred with a frequency of > 5% and more frequently in the subjects treated with fluticasone propionate and salmeterol inhalation powder were nasopharyngitis, upper respiratory tract infection, nasal congestion, back pain, sinusitis, dizziness, nausea, pneumonia, candidiasis, and dysphonia. Overall, 55 (7%) of the subjects treated with fluticasone propionate and salmeterol inhalation powder and 25 (3%) of the subjects treated with salmeterol developed pneumonia. The incidence of pneumonia was higher in subjects older than 65 years, 9% in the subjects treated with fluticasone propionate and salmeterol inhalation powder compared with 4% in the subjects treated with fluticasone propionate and salmeterol inhalation powder younger than 65 years. In the subjects treated with salmeterol, the incidence of pneumonia was the same (3%) in both age groups. The distribution of adverse events was similar to that seen in the 1-year trials with fluticasone propionate and salmeterol inhalation powder 250 mcg/50 mcg. In addition, pneumonia was reported in a significantly increased number of subjects treated with fluticasone propionate and salmeterol inhalation powder 500 mcg/50 mcg and fluticasone propionate 500 mcg (16% and 14%, respectively) compared with subjects treated with salmeterol 50 mcg or placebo (11% and 9%, respectively). When adjusted for time on treatment, the rates of pneumonia were 84 and 88 events per 1,000 treatment-years in the groups treated with 13 fluticasone propionate 500 mcg and with fluticasone propionate and salmeterol inhalation powder 500 mcg/50 mcg, respectively, compared with 52 events per 1,000 treatment-years in the salmeterol and placebo groups. Similar to what was seen in the 1-year trials with fluticasone propionate and salmeterol inhalation powder 250 mcg/50 mcg, the incidence of pneumonia was higher in subjects older than 65 years (18% with fluticasone propionate and salmeterol inhalation powder 500 mcg/50 mcg versus 10% with placebo) compared with subjects younger than 65 years (14% with fluticasone propionate and salmeterol inhalation powder 500 mcg/50 mcg versus 8% with placebo). Laboratory Abnormalities: There were no clinically relevant changes in these trials. Specifically, no increased reporting of neutrophilia or changes in glucose or potassium was noted. These events have been chosen for inclusion due to either their seriousness, frequency of reporting, or causal connection to fluticasone propionate and salmeterol inhalation powder, fluticasone propionate, and/or salmeterol or a combination of these factors. Cardiac Disorders: Arrhythmias (including atrial fibrillation, extrasystoles, supraventricular tachycardia), ventricular tachycardia. Immune System Disorders: Immediate and delayed hypersensitivity reaction (including very rare anaphylactic reaction). Musculoskeletal, Connective Tissue, and Bone Disorders: Arthralgia, cramps, myositis, osteoporosis. Behavioral changes, including hyperactivity and irritability, have been reported very rarely and primarily in children. Respiratory, Thoracic, and Mediastinal Disorders: Chest congestion; chest tightness; dyspnea; facial and oropharyngeal edema, immediate bronchospasm; paradoxical bronchospasm; tracheitis; wheezing; reports of upper respiratory symptoms of laryngeal spasm, irritation, or swelling such as stridor or choking. No formal drug interaction trials have been performed with fluticasone propionate and salmeterol inhalation powder. Ketoconazole: Fluticasone Propionate: Coadministration of orally inhaled fluticasone propionate (1,000 mcg) and ketoconazole (200 mg once daily) resulted in a 1. However, under certain circumstances, there may be no acceptable alternatives to the use of beta-adrenergic blocking agents for these patients; cardioselective beta-blockers could be considered, although they should be administered with caution. There are clinical considerations with the use of fluticasone propionate and salmeterol inhalation powder in pregnant women (see Clinical Considerations). Experience with oral corticosteroids suggests that rodents are more prone to teratogenic effects from corticosteroids than humans. The estimated risk of major birth defects and miscarriage for the indicated population is unknown.
Generic 1 mg doxazosin overnight delivery. 6 Amazing Benefits Of Kiwi Fruits During Pregnancy.
The buffering effect of sodium citrate is proportional to the sodium ions it contains: a mole of trisodium citrate produces the same buffering effect as 3 moles of sodium bicarbonate; whereas preparations of citrate gastritis relief order doxazosin 2 mg on line, including hydrogen citrate gastritis in english language buy doxazosin 1mg with visa, have proportionally less buffering effect chronic gastritis risks cheap doxazosin 1mg on-line. Regional citrate anticoagulation requires a strict protocol gastritis symptoms heart attack doxazosin 1 mg online, adapted to the local treatment modality and flow settings. The protocol should include instructions for the infusion of citrate and calcium, for the composition of the dialysate/replacement fluid, and for intensive metabolic monitoring, including acid-base status, sodium, and total and ionized calcium levels. For ethical reasons, these trials were performed in patients without increased bleeding risk. Patients with high bleeding risk, liver cirrhosis, and sensitivity to heparin were excluded. The dosing regimen of heparin consisted of a bolus of 2000 to 5000 U, 97 chapter 5. Despite this rather high heparin dose, the citrate group had a longer filter lifetime and less spontaneous filter failure. Fewer patients in the citrate group required transfusion, and the number of transfused units was also lower. One patient in the heparin group experienced bleeding and one patient in the citrate group had metabolic alkalosis. Patients with contra-indications to one of the two anticoagulants (mainly high bleeding risk/ severe coagulopathy or metabolic problems that might be aggravated by citrate) or who required systemic anticoagulation for medical reasons were excluded. Two patients in each group crossed over to the other anticoagulant and these filters were not included in the analysis. The trial was stopped early after 79 filters because of an advantage using citrate, which resulted in a significantly improved filter survival (124. In addition, significantly less citrateanticoagulated filters were terminated for clotting (16. Three patients in the citrate group had metabolic alkalosis and two had hypocalcemia. However, the number of major bleedings and the need for transfusion was significantly greater in the heparin group. Two cases of metabolic alkalosis were noted in the heparin group and two episodes of hypocalcemia in the citrate group. Both treatment arms had a relatively short filter life (13 hours for regional heparinization and 17 hours for citrate) that did not differ significantly. Nadroparin was started with a bolus of 2850 U followed by 380 U/h without further monitoring. Citrate (500 mmol/l) was administered at a dose of 3 mmol per liter blood flow, without monitoring of postfilter ionized calcium. The primary outcomes were safety, defined as the absence of adverse events necessitating discontinuation of the study anticoagulant, and efficacy, defined as circuit survival. Safety was significantly better in the citrate group with only two patients requiring a change in anticoagulation regimen vs. A computerdriven combination of buffered and nonbuffered replacement fluids was used in the citrate group, explaining why metabolic alkalosis occurred more frequently in the nadroparin group. Rather surprisingly, the authors also found an improved renal recovery and an improved hospital survival in the citrate group. This could not be attributed to differences in severity of illness, nor in bleeding or transfusion requirement, and requires further investigation. In observational trials, the most frequent metabolic complication is metabolic alkalosis, occurring in up to 50% of the patients. Markedly reduced citrate clearances and lower ionized calcium levels have been found in patients with acute liver failure or with severe liver cirrhosis. The ratio of total to ionized calcium appears to be the best parameter to detect citrate accumulation611,612 with an optimal cutoff at 2. There was no difference in filter survival (with electively discontinued filters being censored). Three patients in each group had bleeding, with no difference in transfusion requirement between the two groups. The incidence of bleeding was low and not different between the two anticoagulants. A possible exception can be made for patients who do not have contraindications for citrate. Randomized trials comparing citrate with heparins have been performed in patients without increased bleeding risk. It is cumbersome and difficult to titrate because heparin has a much longer half-life than protamine, inducing a risk of rebound. Its main clinical complication is the development of thrombocytopenia with or without thrombosis. Candidates are the direct thrombin inhibitors lepirudin, argatroban, or bivaluridin, or the antithrombin-dependent Factor Xa inhibitors, danaparoid or fondaparinix. The second aspect of the citrate protocol provides prevention of citrate-induced systemic hypocalcemia by providing a calcium chloride continuous infusion (8 g calcium chloride per liter normal saline) to the patient via a central line. Calcium is a requisite cofactor in both the intrinsic and extrinsic coagulation cascades. Citrate functions by binding free calcium, thereby inhibiting coagulation in both the intrinsic and extrinsic coagulation pathways. Most studies on indwelling tunneled dialysis catheters have been performed in chronic dialysis patients. No recommendation can be given regarding the optimal timing to change the nontunneled-uncuffed catheter to a more permanent access. It seems reasonable to create a more permanent access when recovery of kidney function is unlikely. The optimal timing should take into account the increased risk of infection with untunneled catheters, but also the practical issues related to the insertion of a tunneled catheter. Several configurations of dialysis catheter lumen and tip have emerged over the years with no proven advantage of one design over another. The outer diameter varies between 11 and 14 French and it is self-evident that larger sizes decrease the risk of inadequate blood flow. In order to provide an adequate blood flow and reduce the risk of recirculation, the tip of the catheter should be in a large vein (see Recommendation 5. Further modifications, including the use of swan-neck catheters, T-fluted catheters, curled intraperitoneal portions, dual cuffs, and insertion through the rectus muscle instead of the midline, have been made to reduce remaining complications such as peritonitis, exit/tunnel infection, cuff extrusion, obstruction, and dialysate leaks. In the remaining 30 patients, those with tunneled catheters had an increased insertion time and more femoral hematomas, but also less dysfunction, fewer infectious and thrombotic complications, and a significantly better catheter survival. In addition, the use of tunneled catheters for starting acute dialysis is not widespread practice. Catheters in the right internal jugular vein have a straight course into the right brachiocephalic vein and superior vena cava, and, therefore, the least contact with the vessel wall. A catheter inserted through the subclavian or the left jugular vein has one or more angulations. Whether this recommendation should be extended to the left jugular vein remains unclear. In patients where the subclavian vein remains the only available option, preference should be given to the dominant side in order to spare the nondominant side for eventual future permanent access. Because the subclavian vein should be avoided, the remaining options are the jugular and femoral veins.
History and Physical Examination Tachypnea is most common gastritis during pregnancy buy cheap doxazosin 4mg line, pleuritic chest pain gastritis sintomas cheap 4 mg doxazosin fast delivery, hemoptysis gastritis diet ayurveda cheap doxazosin 4 mg fast delivery, tachycardia gastritis symptoms tagalog generic doxazosin 4 mg otc, hypotension, hypoxemia, and hypocarbia common. Optional: Potential to be removed, however can remain permanently in place, 1/4 removed most series. Poor history and already had a filter, always check abdominal X-ray on table prior to prepping patient. Occasionally we will find bilateral common femoral occlusions after filter is opened. Never advance sheath in vena-cava without wire or introducer (tip can be advanced into lumbar vein). Understand the filter you are deploying, the classic mistake of pushing and pulling at same time can push filter out into adjacent branches (renal or lumbar veins). Tissue susceptibility to ischemia: need for fasciotomy still most dependent on clinical stage of ischemia, not duration. If Pringle maneuver stops bleeding: Hepatic artery/portal vein injury disrupted (ligaments, diaphragm, liver parenchyma). Registries and prospective studies are urgently needed to improve the state of knowledge. Table 2 Levels of evidence Data derived from multiple randomized clinical trials or meta-analyses. Data derived from a single randomized clinical trial or large non-randomized studies. Consensus of opinion of the experts and/ or small studies, retrospective studies, registries. Surveys and registries are needed to verify that real-life daily practice is in keeping with what is recommended in the guidelines, thus completing the loop between clinical research, writing of guidelines, and implementing them into clinical practice. Also the treatment of congenital heart disease has improved, resulting in an increased number of women with heart disease reaching childbearing age. Nevertheless, the number of such patients presenting to the individual physician is small. Such guidelines have to give special consideration to the fact that all measures concern not only the mother, but the fetus as well. A therapy favourable for the mother can be associated with an impairment of the child, and in extreme cases treatment measures which protect the survival of the mother can cause the death of the fetus. On the other hand, therapies to protect the child may lead to a suboptimal outcome for the mother. Because prospective or randomized studies are lacking, with a few exceptions, recommendations in this guideline mostly correspond to the evidence level C. Some general conclusions have arisen from these guidelines: counselling and management of women of childbearing age with suspected cardiac disease should start before pregnancy occurs; 2. The heart can increase its size by up to 30%, which is partially due to dilatation. Pregnancy induces a series of haemostatic changes, with an increase in concentration of coagulation factors, fibrinogen, and platelet adhesiveness, as well as diminished fibrinolysis, which lead to hypercoagulability and an increased risk of thrombo-embolic events. In addition, obstruction to venous return by the enlarging uterus causes stasis and a further rise in risk of thrombo-embolism. Physiological changes that occur during pregnancy can affect absorption, excretion, and bioavailability of all drugs. Moreover, the raised renal perfusion and the higher hepatic metabolism increase drug clearance. The altered pharmacokinetics of drugs vary in magnitude during different stages of pregnancy, making careful monitoring of the patient and dose adjustments necessary. Anaesthesia, analgesia, haemorrhage, and infection may induce additional cardiovascular stress. Such increases are associated with a rise in pressure in the amniotic fluid, and in the intrathoracic venous, cerebrospinal, and extradural fluids. In conclusion, the physiological adaptations to pregnancy influence the evaluation and interpretation of cardiac function and clinical status. For defects that are inherited in a polygenic manner, recurrence risk is less clearly defined. For a steadily increasing number of genetic defects, genetic screening by chorionic villous biopsy can be offered in the 12th week of pregnancy. All women with congenital heart disease should be offered fetal echocardiography in the 19th to 22nd week of pregnancy. Measurement of nuchal fold thickness in the 12th to 13th week of pregnancy is an early screening test for women over 35 years of age. The sensitivity for the presence of a significant heart defect is 40%, while the specificity of the method is 99%. The incidence of congenital heart disease with normal nuchal fold thickness is 1/1000. It is advocated in patients with known genetic disorders and is more advisable if treatment options are available. In addition, there are large differences between each of the hereditary heart disease conditions, and the risk for descendants is dependent on whether only the mother, only the father, or both parents suffer from hereditary cardiac defects. Children of parents with a cardiovascular condition inherited in an autosomal dominant manner. The assessment of dyspnoea is important for diagnosis and prognosis of valve lesions and for heart failure. A thorough physical examination considering the physiological changes that occur during pregnancy (Section 2. When dyspnoea occurs during pregnancy or when a new pathological murmer is heard, echocardiography is indicated. Nuclear scintigraphy should be avoided during pregnancy because of radiation exposure. Echocardiography Because echocardiography does not involve exposure to radiation, is easy to perform, and can be repeated as often as needed, it has become an important tool during pregnancy and is the preferred screening method to assess cardiac function. Transoesophageal echocardiography Multiplane transducers have made transoesophageal echocardiography a very useful echocardiographic method in the assessment of adults with, for example, complex congenital heart disease. Transoesophageal echocardiography, although rarely required, is relatively safe during pregnancy. The presence of stomach contents, risk of vomiting and aspiration, and sudden increases in intra-abdominal pressure should be taken into account, and fetal monitoring performed if sedation is used. It has become an integral part of the follow-up of grown up congenital heart disease patients as well as patients with asymptomatic valvular heart disease. If respiratory gas analysis is used, the limit is a respiratory exchange ratio of 1. Stress echocardiography using bicycle ergometry may add to the diagnostic specificity in detecting the presence and extent of ischaemia in high risk patients with possible coronary artery disease. If possible, procedures should be delayed until at least the completion of the period of major organogenesis (. There is no evidence of an increased fetal risk of congenital malformations, intellectual disability, growth restriction, or pregnancy loss at doses of radiation to the pregnant woman of,50 mGy22,23 ( The threshold at which an increased risk of congenital malformations occurs has not been definitely determined. During the first 14 days after fertilization, intact survival without fetal abnormality or death are the most likely outcomes of radiation exposure.