




|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Harold Gee MD FRCOG
Grade 3 or 4 adverse events considered to be probably or possibly related to emtricitabine included leukopenia erectile dysfunction what age does it start order malegra fxt plus 160mg, anemia erectile dysfunction heart buy malegra fxt plus 160mg on-line, gastroenteritis erectile dysfunction testosterone cheap malegra fxt plus 160mg free shipping, and pancreatitis erectile dysfunction fertility treatment order malegra fxt plus 160mg without a prescription, all occurring at a frequency of less than 1% (annual incidence rate) [3]. If stored at room temperature, the oral solution is stable for up to 90 days, and any unused portion must be discarded after this time [1]. Since elimination of emtricitabine is primarily dependent on CrCl, dose adjustments in neonates should be similar to CrCl-based dose adjustments for adults. Increased risk in patients with liver disease; suspend or discontinue treatment if signs or symptoms occur even in the absence of marked transaminase elevations. Inflammatory response (immune reconstitution syndrome) to indolent or residual opportunistic infections may occur during initial phase of treatment [1]. Black Box Warning Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues alone or in combination with other antiretrovirals (in adults) [1]. Mean absolute bioavailability of emtricitabine is 93% and 75% for the capsules and the oral solution, respectively, and the relative bioavailability of the oral solution is approximately 80% of the capsules [1] [4]. Saez-Llorens X, Violari A, Ndiweni D et al: Long-term safety and efficacy results of once-daily emtricitabine-based highly active antiretroviral therapy regimens in human immunodeficiency virus-infected pediatric subjects. Mixture should be placed in a bottle and shaken for at least 2 minutes, left to stand for 60 minutes, and then shaken for an additional minute. Title Enalapril maleate Dose 291 Micormedex NeoFax Essentials 2014 Begin with 40 mcg/kg per dose (0. Bioavailability of oral dosage form is uncertain in neonates, but is significantly less than the 60% reported in adults. Hyperkalemia occurs primarily in patients receiving potassium-sparing diuretics or potassium supplements. Monitoring Frequent assessment of blood pressure, particularly after the first dose. Enalapril oral suspension (200 mL total) can be prepared by crushing ten 20-mg tablets and adding 50 mL of isotonic citrate buffer (Bicitra). Terminal Injection Site Compatibility 293 Micormedex NeoFax Essentials 2014 Amikacin, aminophylline, ampicillin, aztreonam, calcium gluconate, cefazolin, ceftazidime, chloramphenicol, cimetidine, clindamycin, dobutamine, dopamine, erythromycin lactobionate, esmolol, famotidine, fentanyl, gentamicin, heparin, hydrocortisone succinate, lidocaine, linezolid, magnesium sulfate, meropenem, metronidazole, morphine, nafcillin, nicardipine, nitroprusside, penicillin G, phenobarbital, piperacillin, piperacillin/tazobactam, potassium chloride, propofol, ranitidine, remifentanil, sulfamethoxazole/trimethoprim, tobramycin, and vancomycin. Contraindications/Precautions Use with extreme caution in patients with impaired renal function: oliguria and increased serum creatinine occur frequently. Beneficial effects are thought to be caused by a combination of afterload reduction and long-term inhibition of salt and water retention. Terminal Injection Site Compatibility Amikacin, aminophylline, ampicillin, aztreonam, calcium gluconate, cefazolin, ceftazidime, chloramphenicol, cimetidine, clindamycin, dobutamine, dopamine, erythromycin lactobionate, esmolol, famotidine, fentanyl, gentamicin, heparin, hydrocortisone succinate, lidocaine, linezolid, magnesium sulfate, meropenem, metronidazole, morphine, nafcillin, nicardipine, nitroprusside, penicillin G, phenobarbital, piperacillin, piperacillin/tazobactam, potassium chloride, propofol, ranitidine, remifentanil, sulfamethoxazole/trimethoprim, tobramycin, and vancomycin. Once enteral feeding is well established, Enfamil Human Milk Fortifier can be added. Dosage requirements to maintain target anti-factor Xa levels in preterm infants are quite variable, ranging from 0. Treatment outcomes (resolution or reduction of thrombus) were not different between groups. A third retrospective study (n=140) also revealed that less than half of the population achieved therapeutic anti-Xa levels following the initial dose with the current standard treatment guidelines. In a retrospective study, whole-milligram enoxaparin dosing using insulin syringes (undiluted 100 mg/mL; 1 mg enoxaparin = 0. The study included neonates, infants and children (n=514); 27% were infants less than 3 months of age (900 to 4700 g in weight). Five children (less than 1%) had a supra-therapeutic initial anti-Xa level without hemorrhagic consequences. Advantages over standard unfractionated heparin: (1) May be given subcutaneously, (2) More predictable pharmacokinetics, (3) Minimal monitoring, (4) Dosing every 12 hours, (5) Less frequent bleeding complications. One disadvantage is the inability to quickly and completely reverse its anticoagulant effects. Reported complications include major bleeding 300 Micormedex NeoFax Essentials 2014 or hematoma at the administration site, compartment syndrome, intracranial hemorrhage, and gastrointestinal hemorrhage. Black Box Warning Epidural or spinal hematomas, which may result in long-term or permanent paralysis, may occur in patients who are anticoagulated with low molecular weight heparins or heparinoids and are receiving neuraxial anesthesia or undergoing spinal puncture. Consider risks/benefits before neuraxial intervention in patients anticoagulated or to be anticoagulated for thromboprophylaxis. It is also much less likely to interfere with platelet function or cause osteoporosis. Bioavailability is almost 100% after subcutaneous administration, with peak activity 2. Obtain anti-factor Xa levels initially, weekly during hospitalization, and then every 3 to 4 weeks in stable patients. After attaining target levels, dosage adjustments will be necessary once or twice a month, perhaps more often in preterm infants and infants with hepatic or renal dysfunction. Patients undergoing concomitant neuraxial anesthesia or spinal puncture should be monitored frequently for neurological impairment indicating possible spinal or epidural hematoma [5] [6] [7] [8]. Undiluted enoxaparin (100 mg/mL) transferred to tuberculin syringes and stored under 301 Micormedex NeoFax Essentials 2014 refrigeration retained anti-Xa activity for 10 days. Enoxaparin Dilution A 20-mg/mL enoxaparin dilution (in preservative-free sterile water) was stable for 4 weeks in glass vials stored at room temperature. In another stability study, enoxaparin (20 mg/mL in 1-mL tuberculin syringes) diluted in 4% glucose retained greater than 99% of the baseline anti-Xa activity when stored under refrigeration (4 degrees C) for 31 days. At least 90% of the baseline anti-Xa activity was retained under these conditions [11]. Dix D, Andrew M, Marzinotto V, et al: the use of low molecular weight heparin in pediatric patients: a prospective cohort study. Fareed J, Hoppensteadt D, Walenga J, et al: Pharmacodynamic and pharmacokinetic properties of enoxaparin. Klinger G, Hellmann J, Daneman A: Severe aortic thrombosis in the neonate successful treatment with low-molecular-weight heparin: Two case reports and review of the literature. Monagle P, Chalmers E, Chan A, et al: Antithrombotic therapy in neonates and children: Antithrombotic and thrombolytic therapy, 8th Ed. Dosing Issues Several retrospective studies have suggested that higher initial doses are required to more quickly achieve therapeutic anti-Xa levels and reduce the number of dosage adjustments. Another retrospective study (n=150) found that only 41% of patients attained therapeutic antiXa levels with initial dosing consistent with current standard treatment guidelines. The following doses were required to achieve a therapeutic anti-Xa level (dose given every 12 hours): less than one month of age, 1. The following higher doses were required to achieve a therapeutic anti-Xa level (dose given every 12 hours): less than 2 months of age, 1. Contraindications/Precautions Contraindicated in presence of active major bleeding or in patients with thrombocytopenia associated with a positive in vitro test for anti-platelet antibody in the presence of enoxaparin. Major bleeding may occur even with anti-factor Xa levels in the therapeutic range. Reported complications include major bleeding or hematoma at the administration site, compartment syndrome, intracranial hemorrhage, and gastrointestinal hemorrhage. Pharmacology Enoxaparin is a low-molecular weight heparin that has considerably less activity against thrombin than does standard heparin. Bioavailability is almost 100% 305 Micormedex NeoFax Essentials 2014 after subcutaneous administration, with peak activity 2. Monitoring Measure anti-factor Xa concentrations 4 to 6 hours after a dose (therapeutic range, 0. Preterm infants are likely to require several dosage adjustments to achieve the target levels. Monitor patients with renal impairment closely during therapy (dose reduction necessary). Special Considerations/Preparation Available as 100-mg/mL concentration as 30 mg/0. Multidose vial available in 100-mg/mL concentration with 15 mg benzyl alcohol per 1 mL as a preservative. Undiluted enoxaparin (100 mg/mL) transferred to tuberculin syringes and stored under refrigeration retained anti-Xa activity for 10 days. The stability end-point was significant loss of anti-Xa activity; sterility and pyrogenicity tests were not performed [9]. A decrease of 10% (statistically significant) of the initial anti-Xa activity was noted when enoxaparin (20 mg/mL in 1 mL tuberculin syringes) was diluted with sterile water and stored under the same conditions. Stability of enoxaparin in commercially available 5% glucose solution was not tested in this study; however, the authors suggest that an increase in glucose concentration would not affect the stability of the dilution [10].
Pharmacology 622 Micormedex NeoFax Essentials 2014 Inhibits synthesis of bacterial cell wall erectile dysfunction drugs boots malegra fxt plus 160mg cheap. Special Considerations/Preparation Available as powder injection in 250-mg young and have erectile dysfunction purchase malegra fxt plus 160 mg mastercard, 500-mg erectile dysfunction treatment brisbane discount malegra fxt plus 160mg on-line, 1-g erectile dysfunction doctors in arizona malegra fxt plus 160mg with mastercard, 2-g, and 10-g vials. Acyclovir, cefotaxime, cefoxitin, chloramphenicol, dopamine, famotidine, fluconazole, heparin, hydrocortisone succinate, magnesium sulfate, milrinone, morphine, potassium chloride, and zidovudine. Adverse Effects Interstitial nephritis associated with hematuria, albuminuria, and casts in urine. Reconstitute 250 mg vial with 5 mL of sterile water for injection to make a concentration of 50 mg/mL. Reconstituted solution is stable for 4 days at room temperature, 7 days refrigerated. Terminal Injection Site Incompatibility Amikacin, caffeine citrate, gentamicin, netilmicin, sodium bicarbonate, and tobramycin. Special Considerations/Preparation Available as a 50-mg/mL solution in 20 mL and 50 mL multidose vials. A 5-mg/mL dilution may be made by adding 1 mL of the 50-mg/mL solution to 9 mL of preservative-free normal saline. Acyclovir, amikacin, aminophylline, atropine, calcium chloride, chloramphenicol, erythromycin lactobionate, hyaluronidase, insulin, lidocaine, linezolid, neostigmine, and propofol. Cimetidine, fentanyl, hydrocortisone succinate, midazolam, morphine, pancuronium bromide, penicillin G, phenytoin, ranitidine, and vancomycin. Serum half-life is dosedependent (15 to 50 hours in adults) and unknown in neonates. Enhances metabolism of phenytoin, sodium valproate, and corticosteroids by microsomal enzyme induction. Phenobarbital sodium can be diluted to 10 mg/mL in normal saline prior to administration [3]. Oral:The intravenous formulation of phenobarbital, diluted to 10 mg/mL, has been used orally. Pharmacology 628 Micormedex NeoFax Essentials 2014 Phenobarbital limits the spread of seizure activity, possibly by increasing inhibitory neurotransmission. Phenobarbital sodium, diluted to 10 mg/mL in normal saline, was stable for 4 weeks under refrigeration [3]. To avoid alcohol content of the oral solution, an extemporaneous phenobarbital suspension can be compounded by crushing ten (10) 60-mg tablets (600 mg total) into a fine powder. Label "shake well before use"; suspension stable for 115 days at room temperature [4]. Terminal Injection Site Incompatibility 629 Micormedex NeoFax Essentials 2014 Fat emulsion. Based on abstinence scoring, weaning can be achieved by decreasing dose 20% every other day. Phenobarbital sodium can be diluted to 10 630 Micormedex NeoFax Essentials 2014 mg/mL in normal saline prior to administration [3]. Treatment of neonatal abstinence syndrome in nonopiate- or polydrug-exposed infants. Contraindications/Precautions Contraindicated in patients with manifest or latent porphyria, marked liver function impairment, or respiratory disease with dyspnea or obstruction. Pharmacology Phenobarbital limits the spread of seizure activity, possibly by increasing inhibitory neurotransmission. Primarily metabolized by liver, then excreted in the urine as p-hydroxyphenobarbital (no anticonvulsant activity). Irritating to veins - pH is approximately 10 and osmolality is approximately 15,000 mOsm/kg H2O. Monitoring Phenobarbital monotherapy will control seizures in 43% to 85% of affected neonates adding a second drug (phenytoin or lorazepam) is often needed. Drug accumulation may occur using recommended maintenance dose during the first two weeks of life. Altered (usually increased) serum concentrations may occur in patients also receiving phenytoin or valproate. In infants with neonatal abstinence syndrome, serum concentrations of 20 to 30 mcg/mL are associated with adequate symptom control. Special Considerations/Preparation Injectable solution available in concentrations of 60-, 65-, and 130-mg/mL, all containing 10% (100 mg/mL) alcohol and 67. Phenobarbital sodium, diluted to 10 mg/mL in normal saline, was stable for 4 weeks under 631 Micormedex NeoFax Essentials 2014 refrigeration [3]. Transfer suspension to 2-ounce amber plastic bottle and fill to final volume of 60 mL with Ora-Plus/Ora-Sweet mixture. Amikacin, aminophylline, caffeine citrate, calcium chloride, calcium gluconate, enalaprilat, fentanyl, fosphenytoin, heparin, ibuprofen lysine, linezolid, meropenem, methadone, morphine, propofol, and sodium bicarbonate. Hydralazine, hydrocortisone succinate, insulin, methadone, pancuronium, ranitidine, and vancomycin. Contraindications/Precautions Anaphylaxis, anaphylactic shock, and other acute hypersensitivity reactions, some severe and/or fatal, have been reported on initial exposure or re-exposure to palivizumab; permanently discontinue if a severe hypersensitivity reaction occurs. Adequate antibody titers are maintained in most infants for one month following a 15- 633 Micormedex NeoFax Essentials 2014 mg/kg dose. Adverse Effects In clinical trials, fever and rash occurred slightly more frequently in palivizumab recipients (27% and 12%, respectively) compared with those who received placebo (25% and 10%, respectively) [1]. The liquid solution should be stored refrigerated between 2 to 8 degrees C (36 to 46 degrees F). Do not administer to patients who have had a previous significant hypersensitivity reaction to palivizumab [1]. Adequate antibody titers are maintained in most infants for one month following a 15mg/kg dose. Palivizumab does not interfere with the response to other vaccines and as such, they can be administered concurrently. Wu S-Y, Bonaparte J, Pyati S: Palivizumab use in very premature infants in the neonatal intensive care unit. Product Information: Synagis(R) intramuscular injection, palivizumab intramuscular injection. Pharmacology Nondepolarizing muscle-relaxant that competitively antagonizes autonomic cholinergic receptors and also causes sympathetic stimulation. Product maintains full clinical potency for 6 months if kept at room temperature or 36 months when refrigerated. Aminophylline, caffeine citrate, cefazolin, cimetidine, dobutamine, dopamine, epinephrine, esmolol, fentanyl, fluconazole, gentamicin, heparin, hydrocortisone succinate, isoproterenol, lorazepam, midazolam, milrinone, morphine, nitroglycerin, nitroprusside, propofol, ranitidine, trimethoprim-sulfamethoxazole, and vancomycin. Proposed desirable effects are improved oxygenation/ ventilation, reduced barotrauma, and reduced fluctuations in cerebral blood flow. Factors affecting duration of neuromuscular blockade: Potentiation: Acidosis, hypothermia, neuromuscular disease, hepatic disease, renal failure, cardiovascular disease, younger age, aminoglycosides, hypermagnesemia, and hypokalemia. Tachycardia and blood pressure changes (both hypotension and hypertension) occur frequently. Special Considerations/Preparation Available in concentrations of 1 mg/mL (10-mL vials) and 2 mg/mL (2-mL and 5-mL vials). Possibly because of its direct vasodilating action on cerebral blood vessels, papaverine increases cerebral blood flow and decreases cerebral vascular resistance in healthy subjects; oxygen consumption is unaltered. Papaverine is metabolized in the liver and excreted in the urine in an inactive form. Chronic hepatitis, as evidenced by an increase in serum bilirubin and serum glutamic transaminase, has been reported in three adults following long-term papaverine therapy. Pharmacology Papaverine directly relaxes the tonus of various smooth muscle, especially when it has been spasmodically contracted. It relaxes the smooth musculature of the larger blood vessels, especially coronary, systemic peripheral and pulmonary arteries. During administration, the muscle cell is not paralyzed and still responds to drugs and other stimuli causing contraction. Special Considerations/Preparation Supplied as 30-mg/mL solution for injection in 2-mL preservative-free vials and 10-mL multiple dose vials containing 0.
Buy 160 mg malegra fxt plus with visa. ERECTILE DYSFUNCTION TREATMENT DR YOGIS CLINIC CHANDIGARH INDIA +9212222222.
Magnolia hypoleuca (Magnolia). Malegra FXT Plus.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96224
New diagnostic techniques such as the urine D-arabinitol/L-arabinitol ratio impotence related to diabetes discount malegra fxt plus 160 mg mastercard,10 erectile dysfunction heart attack order 160mg malegra fxt plus overnight delivery,11 serum D-arabinitol/ creatinine ratio impotence emedicine buy 160 mg malegra fxt plus with mastercard,12 impotence kit discount 160mg malegra fxt plus mastercard,13 Candida mannan antigen and anti-mannan antibody,14,15 (1,3)-beta-D-glucan assay,16,17 T2 biosystems for Candida18 and real-time polymerase chain reaction19,20 are promising diagnostic alternatives under development for early diagnosis of invasive candidiasis. As noted above, candidemia can result in dissemination of infection to any organ site. There are no pediatric data to guide decisions on when to perform additional diagnostic testing to evaluate for a deep-seated focus. However, among children with persistent candidemia, further investigation for dissemination should strongly be considered. Additional diagnostics to consider in this clinical scenario would include, but not be limited to , an echocardiogram, abdominal ultrasound to evaluate the kidney, liver and spleen, a lumbar puncture and an eye exam (strong, low). Prevention Recommendations Preventing Exposure Candida organisms are common commensals on mucosal surfaces in healthy individuals; no measures are available to reduce exposure to these fungi except by reducing exposure to unneeded antibiotics that may predispose a patient to Candida colonization. Treatment Recommendations Treating Disease Oropharyngeal Candidiasis Early, uncomplicated infection can be effectively treated with topical therapy using clotrimazole troches or oral nystatin suspension for 7 to 14 days (strong, high). Resistance to clotrimazole can develop because of previous exposure to clotrimazole or to other azole drugs; resistance correlates with refractory mucosal candidiasis. Itraconazole capsules and oral solution should not be used interchangeably because, at the same dose, drug exposure is greater with the oral solution than with capsules, and absorption of the capsule formulation varies. In most patients, symptoms should resolve within days after the start of effective therapy. Oral fluconazole for 14 to 21 days is highly effective for treatment of Candida esophagitis and is considered first line therapy (strong. For fluconazole-refractory disease, itraconazole solution, posaconazole, voriconazole, amphotericin B, or an echinocandin are alternatives. An echinocandin is recommended for severely ill children with candidiasis because of the fungicidal nature of these agents, as well as the lack of adverse events (strong, high). Fluconazole is a reasonable alternative for patients who are less critically ill and who have no recent azole exposure. Despite this recommendation, clinicians should be aware of the increasing frequency of C. For patients already receiving fluconazole or voriconazole who are clinically improving despite C. For many of these clinical scenarios, amphotericin B is an effective but less attractive alternative given concerns for therapy-related toxicity (weak, moderate). Amphotericin B lipid formulations may be preferable to conventional amphotericin B deoxycholate given their improved side effect profile (see Monitoring and Adverse Events section below), especially in children at high risk of nephrotoxicity due to preexisting renal disease or use of other nephrotoxic drugs (weak, moderate). If a child is initiated on an intravenous antifungal agent, such as an echinocandin or an amphotericin B formulation, step-down therapy to an oral agent such as fluconazole when the patient is clinically improved to complete the course can be considered (strong, moderate). Species identification is preferred when stepping down to fluconazole because of intrinsic or acquired drug resistance among certain Candida spp. Therefore, it is reasonable to conclude that a central venous catheter should be removed when feasible. Daily fluconazole dosing for invasive candidiasis requires higher doses of fluconazole (12 mg/kg/day) than are used for mucocutaneous disease (6 mg/kg/day), with many experts suggesting a loading dose of fluconazole 25 mg/kg for children. Because of more rapid clearance in children, fluconazole administered to children at 12 mg/kg/day provides exposure similar to standard 400-mg daily dosing in adults. Dosing of fluconazole for invasive candidiasis in children and adolescents should generally not exceed 600 mg/day. This dosing contrasts with the once daily dosing of itraconazole used in adult patients. Administrating itraconazole oral solution on an empty stomach improves absorption (in contrast to the capsule formulation, which is best administered under fed conditions), and monitoring itraconazole serum concentrations, like most azole antifungals, is key in management (generally itraconazole trough levels should be >0. In adult patients, itraconazole is recommended to be loaded at 200 mg twice daily for 2 days, followed by itraconazole 200 mg daily starting on the third day. There is now considerable experience with voriconazole in children, including for treatment of esophageal candidiasis and candidemia. Conversion to oral voriconazole should be at 9 mg/kg orally every 12 hours (strong, moderate). Effective absorption of the oral suspension strongly requires taking the medication with food, ideally a high-fat meal; taking posaconazole on an empty stomach will result in approximately one-fourth of the absorption as in the fed state. The tablet formulation has better absorption given its delayed release in the small intestine, but absorption will still be slightly increased with food. There is potential for overdosing if this tablet formulation is dosed inappropriately. Similarly, in adult patients the extended-release tablet is dosed as posaconazole 300 mg twice daily on the first day, then 300 mg once daily starting on the second day. In adult patients, the maximum amount of posaconazole oral suspension given is 800 mg per day (given its excretion), and that dosage has been given as posaconazole 400 mg twice daily or 200 mg four times a day in severely ill patients because of findings of a marginal increase in exposure with more frequent dosing. Dosing in adult patients is loading with isavuconazole 200 mg (equivalent to isavuconazonium sulfate 372 mg) every 8 hours for 2 days (6 doses), followed by isavuconazole 200 mg once daily for maintenance dosing. Echinocandins Data from studies using echinocandins (caspofungin, micafungin, and anidulafungin) are now sufficient to recommend these agents as alternatives to fluconazole for esophageal candidiasis, and as first-line therapy for invasive candidiasis (strong, high). The recommended dose of micafungin for children aged 2 years to 17 years is 2 to 4 mg/kg daily, but neonates require doses of micafungin 10 mg/kg daily (strong, moderate). In children who have azotemia or hyperkalemia, or who are receiving high doses of amphotericin B. Decisions on which lipid amphotericin B preparation to use should, therefore, largely focus on side effects and costs. The standard dosage of these preparations is 5 mg/kg/day, in contrast to the 1 mg/kg/day of amphotericin B-D. The advantage of the lipid preparations is the ability to safely deliver a greater overall dose of the parent AmB drug. Despite in vitro concentration-dependent killing, a clinical trial comparing L-AmB at doses of 3 mg/kg/ day and 10 mg/kg/day found no efficacy benefit for the higher dose and only greater toxicity. There are reports of using higher dosing in very difficult infections where amphotericin B is the first-line therapy. Amphotericin B has a long terminal half-life and, coupled with the concentration-dependent killing, the agent is best used as single daily doses. If the overall amphotericin B exposure needs to be decreased due to toxicity, it is best to increase the dosing interval. Combination antifungal therapy Data in adults are limited on use of combination antifungal therapy for invasive candidal infections; combination amphotericin B and fluconazole resulted in more rapid clearance of Candida from the bloodstream but no difference in mortality. Overall there are insufficient data to support routine use of combination therapy in children with invasive candidiasis (weak, low). These interactions can result in decreased plasma concentration of the azole because of increased metabolism induced by the coadministered drug, or development of unexpected toxicity from the coadministered drug because of increased plasma concentrations secondary to azole-induced alterations in hepatic metabolism. Skin rash and pruritus can occur with all azoles; rare cases of Stevens-Johnson syndrome and alopecia have been reported with fluconazole therapy. All azole drugs are associated with asymptomatic increases in transaminases (1% to 13% of patients). Hematologic abnormalities have been reported with itraconazole, including thrombocytopenia and leukopenia. Of the azoles, ketoconazole is associated with the highest frequency of side effects. Its use has been associated with endocrinologic abnormalities related to steroid metabolism, including adrenal insufficiency and gynecomastia, hemolytic anemia, and transaminitis. Dose-related, reversible visual changes, such as photophobia and blurry vision, have been reported in approximately 30% of patients receiving voriconazole. Voriconazole is a tri-fluorinated agent with up to 16% fluoride and after prolonged exposure can result in excess fluoride accumulation in the recipient. Patients will often present with non-specific bone pain and have periosteal reaction seen on radiographs. Adverse effects of amphotericin B are primarily nephrotoxicity, defined by substantial azotemia from glomerular damage, and can be accompanied by hypokalemia from tubular damage. Infusion-related fevers, chills, nausea, and vomiting occur less frequently in children than in adults. Onset of the febrile reactions occurs usually within 1 to 3 hours after the infusion is started; the reactions typically last for <1 hour and tend to decrease in frequency over time. Pre-treatment with acetaminophen or diphenhydramine may alleviate febrile reactions. Idiosyncratic reactions, such as hypotension, arrhythmias, and allergic reactions, including anaphylaxis, occur less frequently. Hepatic toxicity, thrombophlebitis, anemia, and rarely neurotoxicity (manifested as confusion or delirium, hearing loss, blurred vision, or seizures) also can occur.
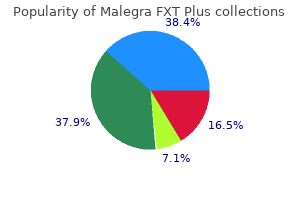
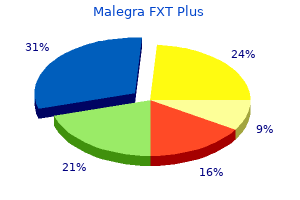
For the factorial trial (P005/1019) erectile dysfunction diabetes reversible order 160mg malegra fxt plus with amex, both ertugliflozin/sitagliptin treatment arms erectile dysfunction doctor san jose order malegra fxt plus 160mg without a prescription. For the sixth trial (P003/1013) effective erectile dysfunction treatment discount 160mg malegra fxt plus with mastercard, noninferiority with glimepiride was only achieved for the ertugliflozin 15 mg treatment arm erectile dysfunction age 16 order 160 mg malegra fxt plus fast delivery. Durability of Response For six of the seven trials, the primary endpoint was assessed at 26 weeks. These trials allowed subjects to participate in a 26- to 78-week site- and subject-blind long-term treatment period (Phase B). Therefore, following treatment discontinuation, persistence of the antihyperglycemic effects of these study medications would not be expected. Cambon requested additional analyses from the Applicant and conducted several sensitivity analyses of the primary efficacy endpoint (data not shown). Please refer to his Statistical Review for detailed discussion of the sensitivity analyses performed to support the findings of the primary efficacy analysis. Cambon also performed subgroup analyses (based on the following intrinsic factors: sex, race, age, and geographic region) of a pool of four Phase 3 trials. The pooled subgroup analyses (dated September 16, 2017) yielded similar results to those conducted by Dr. The clinical relevance of these nominal changes is uncertain, but it does suggest that the 15 mg dose of ertugliflozin offers a benefit for some patients above what would be seen with the 5 mg dose. All seven Phase 3 clinical trials included a 26- to 52-week double-blind treatment period. This trial also includes three 18-week sub-studies that evaluate the efficacy of ertugliflozin in subjects receiving background insulin with or without metformin, background sulfonylurea monotherapy, and background metformin plus a sulfonylurea. Since these antihyperglycemic agents are commonly used as combination therapy for patients with T2D, the findings from these sub-studies may help to determine the potential benefit and risks associated with ertugliflozin used in combination with these medications. The results of this ongoing trial will provide important safety information on the effects of ertugliflozin on bone that may be relevant when considering the use of this product in special populations. Further, a significant number of patients with T2D do not achieve adequate glycemic control despite the availability of numerous therapeutic options (Table 42), and nonadherence or intolerance to the prescribed treatment regimen is common. Six of these trials evaluated the effects of ertugliflozin (5 and 15 mg) as monotherapy and in combination with metformin (1500 mg/day) and/or a sitagliptin (100 mg). The Applicant intends to include all seven efficacy trials in Section 14 of product labeling. For Trial P002/1013, a 52-week active-comparator trial, only the ertugliflozin 15 mg treatment arm was noninferior to the glimepiride arm (mean daily dose 3 mg). Additionally, for the moderate renal impairment trial (P001/1016), the HbA1c reductions from baseline to Week 26 were not significantly different between once daily placebo and ertugliflozin 5 mg or 15 mg. Therefore, ertugliflozin-containing products should not be recommended for patients with moderate to severe renal impairment. In these trials, the efficacy of ertugliflozin (5 and 15 mg) was evaluated in a factorial study in which ertugliflozin and/or sitagliptin were administered as add-on combination therapy with metformin (Trial P005/1019), as add-on combination therapy with metformin plus sitagliptin (Trial P006/1015), and as initial combination therapy with sitagliptin (Trial P017/1047). For the factorial trial, ertugliflozin 5 mg or 15 mg used in combination with sitagliptin 100 mg provided statistically significant improvement in HbA1c compared to the individual components at Week 26. The other two trials also provided supportive evidence of added efficacy with combination therapy. In these trials, the efficacy of ertugliflozin (5 and 15 mg) was evaluated only as add-on combination therapy with background metformin (Trials P007/1017 and P002/1013, P006/1015, P007/1017), and a factorial trial was not conducted/submitted. Other relevant safety events of interest included: hypoglycemia, pancreatitis, hepatic events, hypersensitivity, malignancy, and venous thromboembolic events. Additionally, clinical study reports and analysis datasets were reviewed for safety. Review of the Safety Database Overall Exposure the safety database was comprised of all subjects randomized and treated. Overall, 4,859 subjects were randomized and treated, of which 1,716 received ertugliflozin 5 mg, 1,693 ertugliflozin 15 mg and 1,450 non-ertugliflozin therapy. In the Type C Meeting Written Responses (dated December 28, 2015), the Applicant was informed that full safety data for these ongoing Phase 3 trials. The following exposures were provided in the Application: 3409 subjects were randomized to ertugliflozin, of which 3128 were exposed for 25 week, 2575 for 50 weeks, and 371 for 78 weeks. Categorization of Adverse Events the integrated analyses were conducted primarily using the data from subjects randomized and treated. Safety analyses were performed by the Applicant on all data regardless of rescue (unless specified otherwise) for the blinded treatment periods. Additionally, since obvious trends suggestive of a dose-response were often not apparent, tabular summaries for many of the safety analyses are sorted and presented by the prevalence of events in the combined ertugliflozin treatment arms. Routine Clinical Tests Blood and urine samples were obtained at baseline and typically at scheduled visits during and at the end of the treatment/early termination for evaluation of standard safety laboratory panels (chemistry, hematology, and urinalysis). Blood specimens for evaluation of lipid and glycemic parameters were collected under fasted conditions. Vital signs (including orthostatic changes in blood pressure and pulse rate), typically assessed at scheduled clinic visits, were evaluated based on changes from baseline. Ertugliflozin 15 mg arm: Subject 0100604: a 79-year-old Caucasian female who participated in Trial P001/1016. The subject denied chest pain in the preceding months, but reported frequent palpitations. Blood pressure measurements during treatment exposure, did not reveal hypotension/orthostasis. Relevant prior and concomitant medications included sitagliptin, gliclazide, amlodipine, atorvastatin, hydrochloro-thiazide/valsartan, nebivolol, nitroglycerin 5. Whether it could have been a contributing factor in this at-risk subject is uncertain. Relevant prior and concomitant medications included the use of simvastatin, lisinopril, furosemide, aspirin, cilostazol, metformin, and glimepiride. Due to the presence of comorbidities, including peripheral vascular disease, concomitant loop diuretic use, and a reported Hgb concentration of 14. However, in the Placebo Pool, no subjects had Hct concentrations 65% (considered a critical value). For the cases occurring following at least a six-month of treatment exposure, malignancy was reported in 0. Based on my review of all the malignancy data (including premalignant conditions; Table 31), there did not appear to be any obvious trends or imbalances in the types of malignancies between treatment arms, and no new safety signals were identified. However, these data were limited in terms of assessing causal associations or tumor promoting properties for individual malignancies. Similarly, the abdominal ultrasound showed an enlarged pancreatic head along with gallstones. A cholecystectomy and two liver biopsies were performed on Day 245, and the subject was discharged on Day 246. The liver biopsy results showed a morphological and immunological profile consistent with adenocarcinoma of the liver (samples were positive for carcinoembryonic antigen, caudal type homeobox 2, keratin 18, keratin 17, and had isolated positive cells for keratin 20). Subject 0502213: a 47-year-old white male with T2D for approximately 11 years was randomized to the ertugliflozin15 mg/sitagliptin 100 mg. On Day 108 he was hospitalized for abdominal bloating/discomfort with nausea and vomiting, and discharged on this same day. On Day 115 he was readmitted with abdominal pain and obstructive jaundice (scleral icterus and abdominal tenderness). The subject did not have a history of alcohol abuse, chronic pancreatitis, or liver cirrhosis, and prior medication use was not relevant. The subject was scheduled to be transferred to another facility for further evaluation and management as well as surgical intervention as needed. An endoscopic ultrasound showed a round hypoechoic and heterogeneous mass (50x40 mm in diameter) in the pancreatic head, and fine needle biopsy confirmed adenocarcinoma. The subject underwent a rendezvous procedure (Day 123) with stenting of the common bile duct from liver to intestine. The subject was discharged on Day 125, with plans for follow-up discussion regarding therapeutic options.
References