




|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Caricia Catalani DrPH, MPH

https://publichealth.berkeley.edu/people/caricia-catalani/
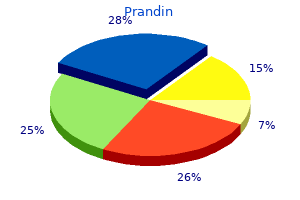
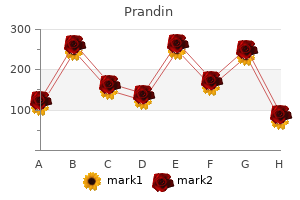
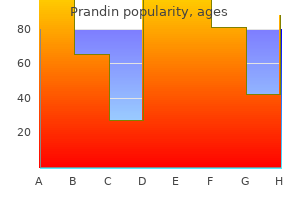
Caution against excess amounts of vitamin A diabetic cheesecake generic 0.5 mg prandin with visa, which can become toxic; fish with mercury exposure such as sharks diabetes 57 buy 1mg prandin with amex, swordfish gestational diabetes test values buy prandin 1 mg low cost, or even canned tuna; unpasteurized dairy products; and undercooked meats diabetes insipidus symptoms urine purchase prandin 0.5 mg. Recommend 30 minutes of moderate exercise or more on most days of the week unless contraindications exist diabetes mellitus risk factors generic prandin 1 mg without a prescription. Women initiating exercise during pregnancy should consider programs developed specifically for pregnant women diabetes mellitus type 2 gangrene buy prandin 2 mg without a prescription. After the first trimester, women should avoid exercise in the supine position, which can compress the inferior vena cava, resulting in dizziness and decreased placental blood flow. Contact sports or activities that risk abdominal trauma are unwise in all trimesters. Pregnant woman should avoid overheating, dehydration, and any exertion that causes notable fatigue or discomfort. Tobacco use accounts for a third of all low-birth-weight babies and many poor pregnancy outcomes, including placental Chapter 19 the Pregnant Woman 363 abruption and preterm labor. Fetal alcohol syndrome is the leading cause of preventable mental retardation in the United States. Ask about commonly abused prescription drugs, including narcotics, stimulants, benzodiazepines. Pursue universal screening of all pregnant women without regard to socioeconomic status. Maintain an updated list of shelters, counseling centers, hotline numbers and other trusted local referrals. Complete a thorough physical exam as much as she permits and document all injuries on a body diagram. As indicated, give tetanus and influenza vaccinations in the second or third trimester. The following vaccines are safe during pregnancy: pneumococcal, meningococcal, and hepatitis B. However, all women should have rubella titers drawn during pregnancy and be immunized after birth if nonimmune. Ask her to wear her gown with the opening in front to ease the examination of both breasts and the pregnant abdomen. Equipment Gynecologic speculum and lubrication: Because of vaginal wall relaxation during pregnancy, a larger-than-usual speculum may be needed. Sampling materials: the cervical brush may cause bleeding, so the Ayre wooden spatula or "broom" sampling device is preferred during pregnancy. Additional swabs may be needed to screen for sexually transmitted infections, group B strep, and wet mount preparations. Tape measure: Use a plastic or paper tape measure to assess the size of the uterus after 20 gestational weeks. Doppler fetal heart rate monitor and gel: Apply a "Doppler" or "Doptone" to the gravid belly to assess fetal heart rate after 10 weeks of gestation. Check for the mask of pregnancy, chloasma, or irregular brownish patches around the forehead and cheeks, across the bridge of the nose, or along the jaw. Nose, including nasal congestion Facial edema after 20 weeks in gestational hypertension Hair loss should not be attributed to pregnancy. Gingival enlargement common Significant enlargement is abnormal and should be investigated. Elevated respiratory rate in infection, pulmonary embolism, peripartum cardiomyopathy. Impulse may be higher than normal in the fourth intercostal space because of transverse and leftward rotation of the heart from the higher diaphragm. This may express colostrum from the nipples; investigate if abnormal bloody or purulent discharge. Irregular contractions after 12 weeks or after palpation during the third trimester Prior to 37 weeks, regular uterine contractions or bleeding are abnormal, suggesting preterm labor. Uterine contractility If woman is >20 weeks pregnant, measure fundal height with a tape measure from the top of the symphysis pubis to the top of the uterine fundus. After 20 weeks, measurement in centimeters should roughly equal the weeks of gestation. If fundal height is more than 4 cm higher than expected, consider multiple gestation, a large fetus, extra amniotic fluid, or uterine leiomyoma. If more than 4 cm lower, consider low level of amniotic fluid, missed abortion, transverse lie, growth retardation, or fetal anomaly. Place your finger gently in the os, and then sweep it around the surface of the cervix. With your internal fingers placed at either side of cervix, palmar surfaces upward, gently lift the uterus toward the abdominal hand. Capture the fundal portion of the uterus between your two hands and gently estimate size. Closed external os if nulliparous; os open to size of fingertip if multiparous Prior to 34 to 36 weeks, cervix should retain normal length of 3 cm. Palpate gently with the fingertips to determine what part of the fetus is in the upper pole of the uterine fundus. Note whether the hands diverge with downward pressure or stay together to learn if the presenting part of the fetus, head or buttocks, is descending into the pelvic inlet. Using one hand at a time, slide your fingers down each side of the fetal body until you reach the "cephalic prominence," that is, where the fetal brow or occiput juts out. Patient endorses fetal movement; denies contractions, vaginal bleeding, and leakage of fluids. On external exam, low transverse cesarean scar is evident; fundus is palpable just below umbilicus. On internal exam, cervix is open to fingertip at the external os but closed at the internal os; cervix is 3 cm long; uterus enlarged to size consistent with 18-week gestation. The "demographic imperative" is to maximize not only life span but also "health span" for older adults so that seniors maintain full function for as long as possible, enjoying rich and active lives in their homes and communities. Investigators distinguish "usual" aging, with its complex of diseases and impairments, from optimal aging. Optimal aging occurs in those people who escape debilitating disease entirely and maintain healthy lives late into their 80s and 90s. Studies of centenarians show that genes account for approximately 20% of the probability of living to 100, with healthy lifestyles accounting for approximately 20% to 30%. A well-lit room allows the older adult to see your facial expressions and gestures. Chairs with higher seating and a wide stool with a handrail leading up to the examining table help patients with quadriceps weakness. Listen to this process of life review to gain important insights and help patients as they work through painful feelings or recapture joys and accomplishments. Older patients may overestimate healthiness even when increasing disease and disability are apparent. To reduce the risk of late recognition and delayed intervention, adopt more directed questions or health screening tools. Be sensitive to changes in presentation of myocardial infarction and thyroid disease. Recognize the symptom clusters typical of different geriatric syndromes, notable interacting clusters of symptoms, for example, falls, dizziness, depression, urinary incontinence, and functional impairment. Searching for the usual "unifying diagnosis" may pertain to fewer than 50% of older adults. Even elders with mild cognitive impairment, however, can provide sufficient history to reveal concurrent disorders. If impairments are more severe, confirm symptoms with family members or caregivers. By 2050, the older adult population will increase by 230%, and the minority older adult population by 510%. Cultural differences affect the epidemiology of illness and mental health, acculturation, the specific concerns of the elderly, the potential for misdiagnosis, and disparities in health outcomes. Review the components of self-awareness needed for cultural responsiveness, discussed in Chapter 3 (pp. Cultural values particularly affect decisions Chapter 20 the Older Adult 375 about the end of life. Elders, family, and even an extended community group may make these decisions with or for the older patient. You might say "Tell me about your typical day" or "Tell me about your day yesterday. Take a thorough medication history, including name, dose, frequency, and indication for each drug. Ask about use of over-thecounter medications, vitamin and nutrition supplements, and moodaltering drugs. Despite the prevalence of alcohol problems among the elderly, rates of detection and treatment are low. Pain and associated complaints account for 80% of clinician visits, usually for musculoskeletal complaints like back and joint pain. Older patients are less likely to report pain, leading to undue suffering, depression, social isolation, physical disability, and loss of function. Taking a diet history and using the Rapid Screen for Dietary Intake and the Nutrition Screening Checklist (p. The prevalence of this multifactorial syndrome related to declines in physiologic reserves, muscle mass, energy and exercise capacity is 4% to 22%. Ask about preferences relating to written "Do Not Resuscitate" orders specifying life support measures "if the heart or lungs were to stop or give out. The goal of palliative care is "to relieve suffering and improve the quality of life for patients with advanced illnesses and their families through specific knowledge and skills, including communication with patients and family members; management of pain and other symptoms; psychosocial, spiritual, and bereavement support; and coordination of an array of medical and social services. As the life span for older adults extends into the 80s, new issues for screening emerge. Consider life expectancy, time interval until benefit from screening accrues, and patient preference. Recommend regular aerobic exercise, resistance training to increase strength, and balance exercise like tai chi. Include the pneumococcal vaccine once after age 65, annual influenza vaccinations, Td boosters every 10 years, and the herpes zoster vaccine. Correct poor lighting, chairs at awkward heights, slippery or irregular surfaces, and environmental hazards. Cancer screening can be controversial because of limited evidence about adults older than age 70 to 80. American Geriatrics Society recommends checking for skin and oral cancers in high-risk patients. Chapter 20 the Older Adult 379 Dementia is "an acquired syndrome of decline in memory and at least one other cognitive domain such as language, visuospatial, or executive function sufficient to interfere with social or occupational functioning. Prominent features include: Normal alertness but short-term memory deficits and subtle language errors. The early stages of mild cognitive impairment may be detected only on neurocognitive testing. Investigate contributing factors such as medications, depression, metabolic abnormalities, or other medical and psychiatric conditions. Screen older patients for possible elder mistreatment, which includes abuse, neglect, exploitation, and abandonment. Prevalence is approximately 1% to 10% of the older population; however, many more cases may remain undetected. Techniques f Examination Techniques of Examination c e a n t n Assessment of the older adult departs from the traditional format of the history and physical examination. Enhanced interviewing, emphasis on daily function and key topics related to elder health, and functional assessment are especially important. The screening tool below is brief, has high inter-rater agreement, and can be used easily by office staff. It covers the three important domains of geriatric assessment: physical, cognitive, and psychosocial function. It addresses key sensory modalities and urinary incontinence, an often unreported problem that greatly affects social interactions and self-esteem in the elderly. If yes, then: Test each eye with Snellen chart while patient wears corrective lenses (if applicable). Positive Screen Yes to question and inability to read >20/40 on Snellen chart Leg mobility: Time the patient after instructing: "Rise from the chair. Inability to hear 1,000 or 2,000 Hz in both ears or either of these frequencies in one ear Unable to complete task in 15 seconds Yes to both questions Yes to the question or weight <100 lbs (continued) Chapter 20 the Older Adult 381 10-Minute Geriatric Screener (continued) Problem and Screening Measure Memory: Three-item recall Depression: Ask: "Do you often feel sad or depressed Screening for common problems in ambulatory elderly: clinical confirmation of a screening instrument. Each year approximately 35% to 40% of healthy community-dwelling older adults experience falls. Incidence rates in nursing homes and hospitals are almost three times higher, with related injuries in approximately 25%. Assess how the fall occurred, seeking details from any witnesses, and identify risk factors, medical comorbidities, functional status, and environmental risks. Couple your assessment with interventions for prevention, including gait and balance training and exercise to strengthen muscles, vitamin D supplementation, reduction of home hazards, discontinuation of psychotropic medication, and multifactorial assessment with targeted interventions. No Answers yes to any screening questions Does the person report a single fall in the past 12 months Obtain relevant medical history, physical examination, cognitive and functional assessment. Yes Reassess periodically Initiate multifactorial/multicomponent intervention to address identified risk(s) and prevent falls: 1. Provide education and information Source: Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. Measure in two positions: supine after the patient rests for up to 10 minutes, then within 2 to 3 minutes after standing up.
Most skin infections transmit through contact with infected individuals or articles ymca diabetes prevention program nyc prandin 0.5mg with amex. Another study carried out in 1996 to determine the prevalence of skin diseases among school children in rural Ethiopia diabetes xpert cheap 1 mg prandin visa, showed that 80 diabetes type 2 causes buy prandin 1mg low price. It is formed by an ordered arrangement of cells called keratinocytes diabetes mellitus type 2 home remedies order 1 mg prandin amex, the basic function of which is to synthesize keratin diabetes beauty treatments cheap prandin 2 mg visa, a filamentous protein that serves a protective function diabetes prevention program 2002 nejm order prandin 0.5mg without prescription. The dermis is the middle layer, composed of collagen, tough and resilient part of the skin lies on the subcutaneous tissue which is principally composed of lobules of fat cells. Although there is a considerable regional variation in their relative thickness: the epidermis is thickest on the palms and soles and very thin on the eyelids. The amount of fat is generous on the abdomen and buttock compared with the nose and sternum. Cells of the epidermis Keratinocyte - produces keratin which forms the outer most skin layer covered by thin lipids to give the skin protective capacity from water and heat loss, penetration of microbial agents, and other trauma by physical mechanisms. In this way, the skin is very crucial part of the immune system because of the large surface area that it spans. Protection: it protects the body from many environmentally unfavorable factors; such as, thermal, chemical, ultra violet radiation and different disease-causing microorganisms. It also protects from unnecessary entry and egress of fluids into and from the body. The skin is a peripheral thermoregulatory organ through sweating, vasodilation, and shivering. Immunologic: the skin is an end organ for many immunologically mediated disorders as well as a tool for immunologic research. The skin can be viewed as a peripheral arm of the immune system involved in normal homeostasis and host defense. Synthetic function: the skin synthesizes vitamin D, different hormones, melanin, and other substances. It begins by taking history, physical examination, and laboratory investigations when needed. A proper skin examination should be performed in good light; preferably in daylight. While describing skin lesions, the following features should be identified: Sites involved and distribution: - if lesions are affecting both sides of the body symmetrically, it probably could have an endogenous origin. Primary lesions Macule: flat lesion due to a localized color change only; the surface is normal (size <1cm) Patch: similar to a macule but the size (> 1cm) Nodule: any elevated lesion (> 1cm diameter) which has a round surface. Fissure: linear split in the epidermis or dermis at an orifice (angle of the mouth or anus), over a joint or along a skin crease. Surface features Normal/ smooth: the surface is not different from the surrounding skin and feels smooth Scaly: dry/flaky surface due to abnormal stratum corneum with accumulation of or increased shedding of keratinocytes. Friable: surface bleeds easily after minor trauma Crust: dried serum, pus or blood Excoriation: localized damage to the skin due to scratching. Lichenification: thickening of the epidermis with increased skin markings due to persistent scratching. Umblicated; surface contains a round depression in the centre, characteristics of molluscum contagiosum or herpes simplex. Purpose of the Module the ultimate purpose of this training module is to produce competent Health Officers who can correctly identify and effectively manage common dermatologic problems both in clinical and community settings. Direction for Using the Satellite Module this satellite module can be used in the basic training of Health Center team particularly health officers who are in the training and service programs. In order to make maximum use of the satellite module, the health officer should follow the following directions. Use listed references and suggested reading materials to supplement your understanding of the problem. For total and comprehensive understanding of the causes (etiology/pathogenesis) and prevention of common skin diseases, the Health Officer Students are advised to refer to the core module. Significance and Brief Description of the Problem See the part under unit 2 section 2. Learning Objectives At the end of reading this module, the health officer student will be able to: 1. Identify and describe the clinical manifestations and complications of skin problems. Describe the principles and methods of treatment for the commonly encountered skin diseases. Select the appropriate treatment for a patient presented with a skin complaint in Ethiopia. Identify and manage or refer timely, diseases when needed a patient with skin 12 3. Discuss the functions of skin in terms of a) Protection b) Thermoregulation c) Immunologic function d) Synthesis e) Others 2. What do you understand by the term skin failure (exfoliative dermatitis or erythroderma) A two year old child presented with itchy, faintly papular eczematous lesions on both cheeks, forehead and neck. Generalized dryness of the skin and lesions on the lateral aspects of the extremities were also seen. Skin colored papules and nodules with shining surfaces and umblicated top were noted on a four year old child. A six year old child presented with high fever, pain, and diffusely swollen left leg of two day duration. On examination of the limb; erythematous, grossly swollen, hot, and tenderness elicited with left side inguinal lymphadenopathy which was also tender. Bacterial infection of the skin (pyodermas) Bacterial skin infection is one of the commonly encountered problems in the tropics. When the normal protective functions of the skin are altered by trauma (scratching and excoriation), pre existing and/or coexisting skin diseases like, eczema, scabies or venous or lymphatic insufficiency, pathogenic organisms get access to the skin to establish infection. Two main clinical forms are recognized: non-bullous impetigo (or impetigo contagiosa) and bullous impetigo. Impetigo presents as either a primary pyodermal of intact skin or a secondary infection due to preexisting skin disease or traumatized skin. Impetigo rarely progresses to systemic infection, although post streptococcal glomerulonephritis may occur as a rare systemic complication. However, children younger than 6 years have a higher incidence of impetigo than adults. Bullous impetigo is most common in neonates and infants Causative agents It is caused by Staphylococcus aureus. The non-bullous form is usually caused by group A streptococcus, in some geographical areas Staphylococcus aureus or by both organisms together. Clinical features Non-bullous impetigo: the characteristic lesion is a fragile vesicle or pustule that readily ruptures and becomes a honey-yellow, adherent, crusted papule or plaque and with minimal or no surrounding redness and usually occurs on hands and face. Bullous impetigo: the characteristic lesion is a vesicle that develops into a superficial flaccid bulla on intact skin, with minimal or no surrounding redness. The roof of the bulla ruptures, often leaving a peripheral collarette of scale if removed; it reveals a moist red base. Management Local management for small lesions: - Wash with betadine solution or saline. Potassium permanganate 1 in 1000 solution soaking twice a day until the pus exudates dry up. Topical antibiotics can be used, such as 2% mupirocin, Gentamycine, Fucidic acid can be used but costly. Systemic treatment: - for impetigo contagiosa, a single dose of benzathin penicillin coupled with local care. The underlining skin conditions such as eczemas, scabies, fungal infection, or pediculosis should be treated. When impetigo is neglected it becomes ecthyma, a superficial infection which involves the upper dermis which may heal forming a scar. However, fungi and virus can also A furuncle is an acute, deep-seated, red, hot, tender nodule or abscess that evolves around the hair follicle and is caused by staphylococcus aureus. A carbuncle is a deeper infection comprised of interconnecting abscesses usually arising in several adjacent hair follicles. Furuncle and carbuncle are common in obese, diabetic patients and immunosuppressive conditions. Cellulitis and Erysipelas Cellulitis is bacterial infection and inflammation of loose connective tissue (dermis subcutaneous tissue) Erysipelas is a bacterial infection of the dermis and upper subcutaneous tissue; characterized by a well-defined, raised edge reflecting the more superficial (dermal) involvement Etiology the most common etiologic agent is group A hemolytic streptococcus. Classical erysipelas starts abruptly and systemic symptoms may be acute and severe, but the response to treatment is more rapid. In erysipelas, the edge of the lesion is well demarcated and raised, but in cellulitis it is diffuse. In erysipelas, blisters are common and severe cellulitis may also show bullae or necrosis of epidermis and can rarely progress to fasciitis or myositis. A skin break, usually a wound even if superficial, an ulcer, or an inflammatory lesion including interdigital fungal or bacterial infection, may be identified as a portal of entry. Erysipelas may occur on the face or extremities and usually accompanied by malaise and fever. Complications Without effective treatment, complications are common - fasciitis, myositis, subcutaneous abscesses, and septicemia. Crystalline penicillin or procaine penicillin is the first line therapy and oral Ampicillin or Amoxicillin may be used for mild infection and after the acute phase resolves. Erythrasma Erythrasma is a chronic superficial infection of the intertriginous areas of the skin. It is caused by over growth of Corynebacterium minutissimum, which usually is present as a normal flora of the skin. It occurs most commonly in the groins, axillae and the intergluteal and submammary flexures, or between the toes. In the groins, it affects the area of one or both thighs in contact with the scrotum. It is difficult to differentiate erythrasma of the toe clefts from Tinea pedis or Candida infection. Since most patients have both Candida and erythrasma, it may worsen if only one condition is treated. The duration of therapy varies, but 2 weeks is usually sufficient for topical fucidin and erythromycin. In these cases, the usual approach adopted is to give long-term antiseptic soaps, such as povidone-iodine and to use drying agents, such as powders, in the affected areas. Superficial fungal infection of the skin Superficial fungal infections of the skin are one of the most common dermatologic conditions seen in clinical practice. However, making the correct diagnosis can be difficult, because these infections can have an atypical presentation or be confused with similar-appearing conditions. Superficial fungal infections can be divided into three broad categories: dermatophytic infections, Pityriasis versicolor and cutaneous candidasis 3. Dermatophytes Specifically Trichophyton, Epidermophyton and Microsporum species, are responsible for most superficial fungal infections. Dividing infections into the body region most often affected can help in identification of the problem. Tinea Capitis Tinea capitis is a dermatophytic infection of the head and scalp, usually found in infants, children, and young adolescents. Around puberty, sebum production by sebaceous glands becomes active, and as a result, it tends to disappear. Commonest presentation is scaly patches on the scalp with variable degree of hair loss and generalized scaling that resembles seborrhic dermatitis may occur on the scalp. An unusual scaling reaction known as favus may give the scalp a waxy or doughy appearance with thick crusted areas. Griseofulvin in a dose of 10-20 mg per kg for six weeks to 8weeks is the first-line treatment of Tinea capitis. Ketoconazole 2-4mg per kg for ten days, itraconazole and terbinafine (Lamisil) are good alternatives. Topical treatment can be added to decrease the transmission and accelerate resolution. Tinea corporis Tinea corporis is dermatophytosis of the glabrous skin of the trunk and extremities. Lesions are round, scaly patches that have a well defined, enlarging border and a relatively clear central portion. Itching is variable and not diagnostic Tinea corporis can assume a giant size (Tinea incognito) when steroids are applied for cosmetic reasons or as a result of miss diagnosis. Tinea pedis Tinea pedis is fungal infection of the feet and is usually related to sweating and warmth, and use of occlusive footwear. The infection often presents as white, macerated areas in the 3rd or 4th toe webs. It may also present with a classic pattern on the dorsal surface of the foot or as chronic dry, scaly hyperkeratosis of the soles and heels. Treatment Topical anti fungal creams or ointments applied regularly for 4 - 6 wks. Once-weekly dosing with fluconazole is another option, especially in noncompliant patients.
The essence of success in the use of this suture is to take the finest possible bite during the passage of the needle through the cuticular layer of skin diabetes blood sugar ranges discount prandin 0.5 mg. The bite should be so fine that the needle can be seen through the cuticular layer diabetes symptoms during pregnancy buy generic prandin 2 mg on-line. Failure to take a fine enough bite leads to the raw edges of the wound being grossly everted to the exterior and results in secondary healing diabetes type 2 and fatigue buy generic prandin 0.5 mg on-line. This suture closes the wound in an everted fashion and provides deep closure support diabetic diet 2012 prandin 2mg without prescription. The suture is slightly more everted than the vertical mattress suture but this technique serves well for hand surgery where cosmesis is not as important and buried and deep sutures are contraindicated because of the foreign body effect diabetes prevention 8 week plan cheap prandin 2 mg online. Apical suture - Simple interrupted sutures cannot be used towards the triangulated end of a flap for they interfere with the circulation to the tip diabetes prevention tips in hindi safe prandin 2mg. The apical suture draws the tip into place, taking a bite through the deeper layer of the dermis of the tip, thus avoiding compromise of circulation. When the remaining sutures are inserted, it is best to take fine bites on the flap side towards the tip. Intradermal subcuticular "pull out" sutures - When an injury is necessarily closed under some tension because of tissue loss or there is a desire to avoid prominent suture marks, the most advantageous method of repair is the intradermal subcuticular pull out suture. Either nylon or fine monofilament material may be used and the free ends taped securely to the skin. This suture may be left in for two or three weeks to hold the edges together until the reparative process, delayed by tension, takes over; yet it will not cause ugly scarring that would inevitably accompany conventional skin sutures if left in place for that length of time. To obtain a straight scar, it is necessary that as the needle passes just beneath the dermis that its exit at the wound edge is oriented ever so slightly backwards with each bite. Criteria - Before placing sutures into a wound or operative site, one must consider a number of factors which will determine the kind of material to be used. The physician must consider the tensile strength of the material to insure that it is strong enough to hold the edges together without breaking. Knot security must be considered because some materials are predisposed to unraveling. Absorbable sutures - Absorbable sutures are those which are placed for deep closure and not to be removed. It is a braided synthetic polymer which is less reactive and better able to resist infection from invading bacteria. It is excellent for knot security and holds half of its tensile strength for 25 days. Its primary application is for deep closures of superficial and deep fascia and ligature of small bleeders. It has the greatest tensile strength and wound security and is thus preferred for deep support for prolonged periods. It is manufactured from sheep intestines and can be used plain or treated with chromic salts (chromic oxide) to retard absorption. It has less tensile strength and wound security when compared to the synthetics and causes more tissue reaction. Nonabsorbable sutures - these suture materials are used primarily for external closures where the sutures will be removed. It also causes the least skin irritation and it is at least as good at resisting infection as nylon. Like nylon, it has poor knot security because of its memory and is somewhat more difficult to work with than other nonabsorbable materials. These include silk, cotton, braided nylon (Nurulon), and multifilament dacron (Mersilene). Historically silk has been the mainstay for wound closures but with the advent of the newer synthetics it has fallen from favor. These materials have excellent workability and knot security but have a higher propensity for tissue reactivity and infection. Earlier removal of these sutures will minimize the adverse effects and make use of these materials preferred where maximal control and precision are required. Needle types - There are a bewildering number and types of suture needles, but for use in minor surgery we can concern ourselves with a limited number and types. For the majority of minor wound sutures we can further restrict our use to the cutting needle. This needle has a sharp edge on the convex portion of the needle which allows for ease of insertion into either the deep or superficial tissue because it cuts slightly as it goes. The tapered needle is more like a standard sewing needle that has been curved and essentially punctures the tissue. It is slightly more difficult to work with this needle because more pressure is required to insert the needle and this frequently leads to bent or broken needles. For minor wound care the 3/8 or 1/2 circle are used with suturing material "wedged" or attached to the shank of the needle. Suture needle and wedged material are size designated by a number code followed by a zero. The size of the needle and material (diameter or caliber) becomes smaller as prefix number becomes larger. Wound Taping - Increasingly, physicians are utilizing wound tape for suture repair. The wound tension is more evenly distributed and for obvious reasons there are no lingering suture scars. Compared to standard suturing methods, wound taping is preferred for infection resistance. They are not recommended for wounds that have considerable tension, irregular shaped wounds or concave surfaces. They are not recommended for areas where moisture or oily skin would interfere with the adhesive quality of the tape. Factors such as the location of the wound, the type of wound and the specific goals to be accomplished with the dressing are to be considered when selecting a dressing. Because the head & face are so vascular and resistant to infection, a physician frequently may leave the repaired wound undressed. There have been clinical trials that indicate that simple uncomplicated wounds heal as well and without complication regardless of the application or non-application of a dressing. A great number of wounds can be best served with the application of a simple Band-Aid or two. A dressing performs numerous functions and depending on the presentation, a dressing is designated by the function performed. Wound protection - One of the main functions of a dressing is to protect the wound from further trauma and external contamination. Studies have shown that sutured wounds are vulnerable to bacterial infection up to 72 hours post application. If protection is foremost in the mind of the physician, it is best to initially apply a non-adherent covering such as a Telfa pad over the wound and then apply a measured and cut gauze sponge over the Telfa. These two dressings are anchored in places with sufficient skin tape to insure stability. This dressing is thick enough to provide protection from bacterial invasion and inadvertent accidental trauma. Pressure - Regardless of whether the wound was traumatically introduced or electively performed, there is frequently the formation or accumulation of serous fluid or blood into the wound site. In cases such as these, the physician must be aware of the possibility of a hematoma or a seratoma formation. Should this be a possibility, the physician should select a dressing that applies sufficient downward pressure to insure that these formations are at least minimized. This dressing does not differ dramatically from the previously described dressing, except that rather than cutting the overlying gauze sponge to fit, it is better to take a 4 X 4 gauze sponge and fold it so that it packs up on top of the wound. If anchored securely to the underlying nonadherent Telfa pad, it will create sufficient pressure to discourage hematoma/seratoma formation. Immobilization - Most commonly, the wounds occurring at the joints of the body frequently present the physician with an additional problem of dressing. Repair of wounds at joint spaces often need to be immobilized to prevent disruption of the healing process or accidental suture tearing. During flexion of that joint tremendous tension is applied to the extensor surface and risk of re injury is high. Immobilization can be achieved by splinting, as would be applicable with the digits, reinforcing tapes to anchor the dressing of the extensor surface, or if necessary, a temporary cast to insure complete immobilization. This is rarely necessary but an option to be considered if the wound site and wound extent dictate. Absorption of exudates - Complicated wounds or wounds with potential for infection are likely to exude freely and copiously. Additionally, there are those wounds where formation of hematomas or seratoma cannot be avoided. The physician must take these factors into consideration when selecting a dressing. One option is to add several layers of gauze sponge over the Telfa pad to soak up the exudate. In those cases where a hematoma or a seratoma is unavoidable, the physician should consider the use of a Penrose drain. This technique employs the use of a small section of surgical rubber or a small square of a surgical glove that can be rolled into the shape of a tube and inserted into the inferior most aspect of a wound during closure. Gauze sponges are placed under and over the exposed portion as it projects out from the suture site. The gauze sponges will soak up the exudate that is accumulating in the wound site and the Penrose acts as a conduit for its exit. The Penrose drain can be removed after two or three days or whenever there is no further risk of exudate accumulation. Debridement - There are those rare occasions where debridement with a dressing is to be considered. Though painful to the patient, when the gauze sponge is removed, fresh bleeding will occur and copious amounts of foreign matter can be removed from the wound site as it adheres to the dressing. The physician should exercise this option only if there is no other way to adequately remove the foreign material. Comfort and Appearance - the physician must keep in mind that the dressing s/he places on a patient is his or her signature. The physician should at all times keep in mind the needs of his patient when applying a dressing. The patient, with the exception of a child, does not want attention drawn to their injury or operation. Keep in mind that the patient will not remain in a static position once they leave your office and the physician should consider the use and abuse that the dressing will receive. The dressing should be secure enough to perform the necessary task but not so tight as to restrict normal movement or compromise blood flow. Insure that the outer most edges of the dressing, the taped edges, are uniform and squared with each other. Occlusive Wound Dressing - In recent years the traditional "bandage" type wound dressing has given way to the newer occlusive dressing. Because of the conflict between orthodox teachings to keep a wound dry, the occlusive dressing, which is essentially a "moist wound healing," has not completely caught on. Current literature suggests that the occlusive dressing is superior for both acute and chronic wounds (Arch. There are four types of occlusive dressings; all designed to keep a wound moist and prevent crust formation. Examples of these dressings include Op-Site, Tegaderm, Bioclusive, Uniflex, Oproflex, Ensure-It, Thin Film Wound Dressing, and Blister Film. Initially, this poses no problem, since these dressings only stick to dry, unwounded tissue. However, once epithelialization begins, the potential is real for stripping away newly grown skin by the untimely removal of the dressing. Foams - Examples of foam dressings include Synthaderm and Epilock, both made of nonadherent polyurethane material that is taped in place over the wound. Hydrocolloids - A partial list of hydrocolloids includes Duoderm, Comfeel, and Ulcer Dressing. In all of them, a water-impermeable polyurethane outer covering is separated from the wound by a hydrocolloid material whose composition varies with the particular dressing. Eventually, the accumulation of wound fluid causes a gradual separation of the dressing from the wound, which is the only time a new dressing should be applied. Patients must be warned of the rather malodorous characteristic of the yellow-brown draining fluid under some of these dressings, or else they will discontinue therapy for fear of infection. Hydrogels - the prototype of this kind of dressing is Vigilon, a polyethylene oxide membrane. Generally, only the inner, thin covering is removed to allow contact of the polyethylene with the wound. Presentation a) Type of wound (1) Blunt wounds are characterized by nonviable tissue, edema, and irregular wound edges. Damage to deeper structures calls for referral to an emergency department, general surgeon, or plastic surgeon. Abrasions are usually shallow, typically involving the epidermis and perhaps the dermis, they may contain foreign bodies and are likely to be contaminated. Time of exposure to pathogens determines treatment in some cases, although repairs made up to six hours after injury are usually considered ideal. But in fact, studies of hand lacerations have shown little correlation between incidence of infection and treatment delays of as long as 18 hours. Injury assessment a) History (1) Ask how the injury or injuries were inflicted, whether contaminants and foreign bodies may have been introduced into wounds, and how long the wound has been exposed to air and bacteria. Assess bleeding at the skin surface and deep within the wound where pressure or clotting may have stopped hemorrhage.

If S1 sounds split at apex diabetes medications glyburide side effects discount 1mg prandin overnight delivery, consider an S4 diabetes mellitus hypertension generic prandin 0.5 mg mastercard, an aortic ejection sound diabetes test blood sugar level purchase prandin 2 mg fast delivery, an early systolic click managing diabetes in children buy 0.5 mg prandin with visa, right bundle branch block diabetes symptoms 0f cheap prandin 1mg amex, and premature ventricular contractions diabetes insipidus vs prandin 1mg sale. S1 S2 Chapter 9 the Cardiovascular System 163 Table 9-3 Variations in the Second Heart Sound-S2 During Inspiration and Expiration Physiologic Splitting A2 P2 S1 S2 S1 S2 Heard in the 2nd or 3rd left interspace: the pulmonic component of S2 is usually too faint to be heard at the apex or aortic area, where S2 is single and derived from aortic valve closure alone. Pathologic Splitting S1 S2 S1 S2 Wide splitting of S2 persists throughout respiration; arises from delayed closure of the pulmonic valve. Fixed Splitting S1 S2 S1 S2 Does not vary with respiration, as in atrial septal defect, right ventricular failure. Closure of the aortic valve is abnormally delayed, so A2 follows P2 on expiration, as in left bundle branch block. More on A2 and P2 Increased Intensity of A2, 2nd Right Interspace (where only A2 can usually be heard) occurs in systemic hypertension because of the increased ejection pressure. It also occurs when the aortic root is dilated, probably because the aortic valve is then closer to the chest wall. Decreased or Absent A2, 2nd Right Interspace is noted in calcific aortic stenosis because of immobility of the valve. When a split S2 is heard widely, even at the apex and the right base, P2 is accentuated. Decreased or Absent P2 is most commonly due to the increased anteroposterior diameter of the chest associated with aging. Also ask about any discharge from the nipples, change in breast contour, dimpling, swelling, or puckering of the skin over the breasts. Breast masses show marked variation in etiology, from fibroadenomas and cysts seen in younger women, to abscess or mastitis, to primary breast cancer. All breast masses warrant careful evaluation, and definitive diagnostic measures should be pursued. Adequacies and inadequacies of breast examinations by physicians in mass screenings. Although 70% of affected women have no known predisposing factors, selected risk factors are well established. Use the Breast Cancer Risk Assessment Tool of the National Cancer Institute. See also Table 10-1, Breast Cancer in Women: Factors That Increase Relative Risk, p. The American Cancer Society recommendations, listed below, vary slightly from those of the U. For women at increased risk, many clinicians advise initiating screening mammography between ages 30 and 40, then every 2 to 3 years until 50 years of age. Palpate a rectangular area extending from the clavicle to the inframammary fold, and from the midsternal line to the posterior axillary line and well into the axilla for the tail of Spence. If present, note location, size, shape, consistency, delimitation, tenderness, and mobility. Physiologic nodularity Infection, premenstrual tenderness Cyst, fibroadenoma, cancer Use vertical strip pattern (currently the best validated technique) or a circular or wedge pattern. For the lateral portion of the breast, ask the patient to roll onto the opposite hip, place her hand on her forehead, but keep shoulders pressed against the bed or examining table. For the medial portion of the breast, ask the patient to lie with her shoulders flat against the bed or examining table, place her hand at her neck, and lift up her elbow until it is even with her shoulder. Palpate the axillary nodes, including the central, pectoral, lateral, and subscapular groups. Use the finger pads of the three middle fingers on your left hand to feel for lumps in the right breast. You can also use a circular or wedge pattern, but be sure to use the same pattern every time. Check the entire breast area, and remember how your breast feels from month to month. Repeat the examination on your left breast, using the finger pads of the right hand. While standing in front of a mirror with your hands pressing firmly down on your hips, look at your breasts for any changes of size, shape, contour, or dimpling, or redness or scaliness of the nipple or breast skin. Examine each underarm while sitting up or standing and with your arm only slightly raised so you can easily feel in this area. Raising your arm straight up tightens the tissue in this area and makes it harder to examine. Recording Your Findings Recording the Physical Examination- Breasts and Axillae "Breasts symmetric and smooth, without masses. Cancer Dimpling Retracted nipple Skin Dimpling Abnormal Contours Look for any variation in the normal convexity of each breast, and compare one side with the other. The nipple may deviate, or point in a different direction, typically toward the underlying cancer. Steady, aching Usually more severe Usually more precisely localized over the involved structure than visceral pain Referred pain-occurs in more distant sites innervated at approximately the same spinal levels as the disordered structure. Pain of duodenal or pancreatic origin may be referred to the back; pain from the biliary tree-to the right shoulder or right posterior chest. Pain from pleurisy or acute myocardial infarction may be referred to the upper abdomen. Related symptoms include bloating, nausea, upper abdominal fullness, and heartburn. Possibilities include: Bloating from excessive gas, especially with frequent belching, abdominal distention, or flatus, the passage of gas by rectum Nausea and vomiting Unpleasant abdominal fullness after normal meals or early satiety, the inability to eat a full meal Heartburn Consider diabetic gastroparesis, anticholinergic drugs, gastric outlet obstruction, gastric cancer. Bladder infection Also, consider bladder stones, foreign bodies, tumors, and acute prostatitis. Assess any: Prostatitis, urethritis Polyuria, a significant increase in 24-hour urine volume Nocturia, urinary frequency at night Urinary incontinence, involuntary loss of urine: Diabetes mellitus, diabetes insipidus Bladder obstruction See Table 11-2, Urinary Incontinence, pp. Stress incontinence (poor urethral sphincter tone) Urge incontinence (detrusor overactivity) Overflow incontinence (anatomic obstruction, impaired neural innervation to bladder) From coughing, sneezing, lifting From urge to void From bladder fullness with leaking but incomplete emptying Health Promotion d Counseling: Health Promotion and Counseling: l o u s g Evidence and Recommendations Evidence and Recommendations i e e o d t n Important Topics for Health Promotion and Counseling Screening for alcohol abuse Risk factors for hepatitis A, B, and C Screening for colon cancer Alcohol Abuse. Focus on detection, counseling, and, for significant impairment, specific treatment recommendations. Brief Chapter 11 the Abdomen 185 counseling interventions have been shown to reduce alcohol consumption by 13% to 34% over 6 to 12 months. Hepatitis A vaccine is recommended for children after age 1 and groups at risk: travelers to endemic areas; food handlers; military personnel; caretakers of children; Native Americans and Alaska Natives; selected health care, sanitation, and laboratory workers; homosexual men; and injection drug users. Hepatitis B: Transmission occurs during contact with infected body fluids, such as blood, semen, saliva, and vaginal secretions. Infection increases risk of fulminant hepatitis, chronic infection, and subsequent cirrhosis and hepatocellular carcinoma. Hepatitis B vaccine is recommended for infants at birth and groups at risk: all young adults not previously immunized, injection drug users and their sexual partners, people at risk for sexually transmitted infections, travelers to endemic areas, recipients of blood products as in hemodialysis, and health care workers with frequent exposure to blood products. Hepatitis C: Hepatitis C, now the most common form, is spread by blood exposure and is associated with injection drug use. If average risk at age 50 (high-risk conditions absent), offer the screening options listed. Full colonoscopy or air contrast barium enema detects 80% to 95% of colorectal cancers. Rebound tenderness from peritoneal inflammation; pain is greater when you withdraw your hand than when you press down. Periumbilical mass with expansile pulsations 3 cm in diameter in abdominal aortic aneurysm. Map areas of tympany and dullness with patient supine, then lying on side (see below). Ascitic fluid usually shifts to dependent side, changing the margin of dullness (see below) Tympany Tympany Dullness Shifting dullness Check for a fluid wave. Place your stiffened and straightened fingers on the abdomen, briefly jab them toward the structure, and try to touch its surface. Perform a rectal examination and, in women, a pelvic examination (see Chapters 14 and 15). Pain from irritation of the psoas muscle suggests an inflamed appendix (a positive psoas sign). Right hypogastric pain in a positive obturator sign, suggesting irritation of the obturator muscle by an inflamed appendix. Hook your thumb under the right costal margin at edge of rectus muscle, and ask patient to take a deep breath. Recording Your Findings Recording Your Findings c dn u n n s Recording the Physical Examination-The Abdomen "Abdomen is protuberant with active bowel sounds. It is firm and boardlike, with increased tenderness, guarding, and rebound in the right midquadrant. Transient increases in intra-abdominal pressure raise bladder pressure to levels exceeding urethral resistance. In women, weakness of the pelvic floor with inadequate muscular support of the bladder and proximal urethra and a change in the angle between the bladder and the urethra from childbirth, surgery, and local conditions affecting the internal urethral sphincter, such as postmenopausal atrophy of the mucosa and urethral infection In men, prostatic surgery Decreased cortical inhibition of detrusor contractions, as in stroke, brain tumor, dementia, and lesions of the spinal cord above the sacral level Hyperexcitability of sensory pathways, as in bladder infection, tumor, and fecal impaction Deconditioning of voiding reflexes, caused by frequent voluntary voiding at low bladder volumes Obstruction of the bladder outlet, as by benign prostatic hyperplasia or tumor Weakness of detrusor muscle associated with peripheral nerve disease at the sacral level Impaired bladder sensation that interrupts the reflex arc, as in diabetic neuropathy Urge Incontinence: Detrusor contractions are stronger than normal and overcome normal urethral resistance. Overflow Incontinence: Detrusor contractions are insufficient to overcome urethral resistance. Bladder is typically large, even after an effort to void, leading to continuous dribbling. Chapter 11 the Abdomen 197 Table 11-2 Problem Urinary Incontinence (continued) Mechanisms Functional Incontinence: Inability to get to the toilet in time because of impaired health or environmental conditions Problems in mobility from weakness, arthritis, poor vision, other conditions; environmental factors such as unfamiliar setting, distant bathroom facilities, bed rails, physical restraints Sedatives, tranquilizers, anticholinergics, sympathetic blockers, potent diuretics Incontinence Secondary to Medications: Drugs may contribute to any type of incontinence listed. Is there intermittent claudication, exercise-induced pain that is absent at rest, makes the patient stop exertion, and abates within about 10 minutes Ask "Have you ever had any pain or cramping in your legs when you walk or exercise The American College of Cardiology and the American Heart Association recommend diagnostic studies for renal artery disease, usually beginning with ultrasound, in patients with hypertension before age 30 years; severe hypertension (see p. Symptoms arise from these conditions rather than directly from atherosclerotic changes in the renal artery. Because symptoms are rare, and screening is now shown to reduce mortality by approximately 40%, the U. Preventive Services Task Force recommends one-time screening by ultrasound in men between 65 and 75 years of age with a history of "ever smoking," defined as more than 100 cigarettes in a lifetime. Persisting pallor of palm indicates occlusion of the released artery or its distal branches. Note time required for (1) return of pinkness (normally 10 seconds) and (2) filling of veins on feet and ankles (normally about 15 seconds). Recording Your Findings Recording the Physical Examination-The Peripheral Vascular System "Extremities are warm and without edema. Thin, shiny, atrophic skin; hair loss over foot and toes; thickened, ridged nails. Stasis dermatitis, possible thickening of skin, and narrowing of leg as scarring develops. Decreased pulses, trophic changes, pallor of foot on elevation, dusky rubor on dependency. Edema, pigmentation, stasis dermatitis, and possibly cyanosis of feet on dependency. Chronic Venous Insufficiency Neuropathic Ulcer Located on pressure points in areas with diminished sensation, as in diabetic neuropathy. Place blood pressure cuffs on both arms and ankles as illustrated, then apply ultrasound gel over brachial, dorsalis pedis, and posterior tibial arteries. Measure systolic pressures in ankles Use vascular Doppler to locate dorsalis pedis pulse Inflate cuff 20 mm Hg above last audible pulse Deflate cuff slowly and record pressure at which pulse becomes audible Obtain 2 measures in each ankle and record the average as the dorsalis pedis pressure in that leg Repeat above steps for posterior tibial arteries 5. Inquire about sores or growths on the penis and any pain or swelling in the scrotum. Ask about practices of oral and anal sex and any related sore throat, oral itching or pain, diarrhea, or rectal bleeding. Encourage men, especially those between 15 and 35 years of age, to perform monthly testicular self-examinations. Testicular cancer strikes men ages 15 to 34, especially those with a positive family history or cyptorchidism (see p. Testicular carcinoma Orchitis, torsion of the spermatic cord, strangulated inguinal hernia Lumps Tenderness Epididymis Spermatic cord and adjacent areas Epididymitis, cyst Varicocele if multiple tortuous veins; cystic structure may be a hydrocele See Table 13-4, Abnormalities of the Epididymis and Spermatic Cord, p. Palpate external inguinal ring through scrotal skin and ask patient to strain down. Cup the testicle between your thumbs and forefingers with both hands and roll it gently between the thumbs and fingers. This is a soft, tubelike structure at the back of the testicle that collects and carries sperm, not an abnormal lump. The lump may just be an infection, but if it is cancer, it will spread unless stopped by treatment. Recording Your Findings Recording Your Findings c dn u n n s Recording the Physical Examination-Male Genitalia and Hernias "Circumcised male. A groove extends from the actual urethral meatus to its normal location on the tip of the glans. Scrotal Edema Pitting edema may make the scrotal skin taut; seen in heart failure or nephrotic syndrome.
Order prandin 2 mg overnight delivery. Insulin Pumps in Type 2 Diabetes by Jothydev Kesavadev.
References