




|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Stephen Clyde Yang, M.D.

https://www.hopkinsmedicine.org/profiles/results/directory/profile/0007794/stephen-yang
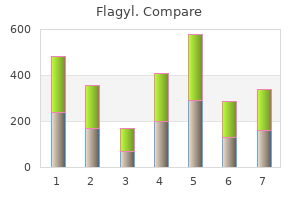
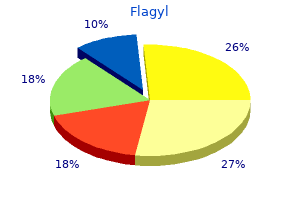
In controlled studies 15 antimicrobial drugs cheap flagyl 500 mg, ibutilide has terminated the arrhythmia in 5 to 88 minutes in approximately 44% of patients treated with 1 mg followed by either 0 antibiotics for breeding dogs 400mg flagyl for sale. When given over 10 minutes bacteria jokes buy 400 mg flagyl visa, it distributes rapidly in a multi-exponential fashion with the clinically relevant component having a half-life from 2 to 12 hours (mean = 6 hours) treatment for dogs cracked nose buy flagyl 400mg lowest price. The drug is mainly eliminated by oxidative hepatic metabolism and systemic clearance is rapid. Because formal drug interaction studies have not been performed, it is not possible to anticipate which enzymes are likely responsible for its elimination. The recommended dose for a patient over 60 kg is 1 mg; if the patient weighs less than 60 kg, 0. For patients whose arrhythmias have not converted by 10 minutes after completion of the first dose, a second dose of equal size can be administered. The risk of torsades de pointes is higher in patients who are female and/or who have reduced ventricular function or electrolyte disorders. Intravenous diltiazem is useful for the temporary control of rapid ventricular rate during atrial fibrillation and flutter. In controlled clinical trials, conversion to sinus rhythm is no more likely with diltiazem than with placebo. The usual dosages for calcium channel blockers for acute treatment are verapamil, 2. By directly slowing atrioventricular nodal conduction, adenosine is very effective for the acute conversion of paroxysmal supraventricular tachycardia caused by re-entry involving the atrioventricular node. Because of the fleeting and relatively selective action of adenosine on the atrioventricular node, it may be used as a diagnostic tool in patients with narrow or wide complex tachycardia. However, it is preferable to make the correct diagnosis before giving any drugs because of the risk of adverse effects. After rapid intravenous injection, the half-life of elimination has been estimated as 1. The drug is rapidly metabolized in the plasma and in cells to form inosine and adenosine monophosphate. Maximal pharmacologic effects are seen within 10 to 20 seconds when given into a central line. Adenosine should be injected intravenously into a proximal tubing site and flushed quickly with saline. An alternative regimen is an initial dose of 50 mug/kg incremented by 50 mug/kg until the paroxysmal supraventricular tachycardia is terminated or side effects become intolerable. Adenosine is contraindicated in patients with sick-sinus syndrome or second- or third-degree heart block unless the patient has a functioning artificial pacemaker. Because of the rapid clearance of adenosine, side effects such as facial flushing, dyspnea, or chest pressure persist less than 60 seconds. Other less frequent side effects include nausea, lightheadedness, headache, sweating, palpitations, hypotension, and blurred vision. Dipyridamole pretreatment increases the potency of adenosine, probably because it blocks its cellular uptake; carbamazepine may potentiate the actions of adenosine. Kuhlkamp V, Mewis C, Mermi J, et al: Suppression of sustained ventricular tachyarrhythmias: A comparison of d, l-sotalol with no antiarrhythmic drug treatment. In a randomized trial of 93 patients with an implantable defibrillator for ventricular fibrillation, d,l- sotalol significantly reduced recurrent ventricular tachycardia; there was no difference in mortality in the two groups. In Members of the Sicilian Gambit (eds): Antiarrhythmic Therapy: A Pathophysiologic Approach. Advances in diagnosing and treating hypertension have played a major role in the dramatic declines in coronary heart disease (-49%) and stroke (-58%) mortality that have occurred in the last 25 years. Adults aged 18 to 74 years with systolic blood pressure of 140 mm Hg or greater or diastolic of 90 mm Hg or greater or taking antihypertensive medication. The patient should be clearly informed that a single elevated reading does not constitute a diagnosis of hypertension but is a sign that further observation is required. Essential, primary, or idiopathic hypertension is systemic hypertension of unknown cause. The importance of identifying patients with secondary hypertension is that they can sometimes be cured by surgery or by specific medical treatment. Thus the morbidity and mortality of potentially ineffective empirical medical therapy can be avoided and the cumulative cost of medical treatment reduced. Both accelerated and malignant hypertension are associated with widespread degenerative changes in the walls of resistance vessels. As a group, these people manifest increased cardiac output, a more rapid heart rate, and higher left ventricular ejection fractions than either the normotensive population or the population of patients with stable hypertension. Blacks have a higher prevalence of hypertension than whites (38% versus 29%), and men have a higher overall prevalence of hypertension than women (33% versus 27%). Hypertension is more common in men than in women up to approximately age 50; after that age, hypertension is more common in women. The prevalence of isolated systolic hypertension increases sharply with age: less than 5% in those younger than 50 years but up to 22% in those 80 years and older. The recent search for genes that contribute to the development of essential hypertension has found that the disorder is polygenic in origin. However, with several exceptions (such as angiotensinogen and alpha-adducin), the particular genes involved are still being sought. Hypertension, in concert with other cardiovascular risk factors, leads to atherosclerosis (see Chapter 39) and other forms of vascular pathology by damaging the endothelium. If hypertension is accompanied by hyperlipidemia, as it is in more than 40% of the U. Non-atherosclerotic hypertension-induced vascular damage can lead to stroke and end-stage renal disease, and increased afterload related to systemic hypertension is a leading cause of congestive heart failure. Furthermore, data from the Framingham Heart Study show two-fold and three-fold increases in the risk of congestive heart failure in hypertensive (stages 1 and 2) men and women, respectively, when compared with normotensive persons in the population. Results are based on the average of three blood pressure measurements with systolic blood pressure of 140 mm Hg or less and/or diastolic blood pressure of 90 mm Hg or less. A mercury sphygmomanometer is preferred; acceptable alternatives include a recently calibrated aneroid manometer or a validated electronic device attached to an arm cuff. Two or three measurements should be taken at each visit, and at least 2 minutes should be Figure 55-2 Pathophysiologic factors most frequently implicated in the development of hypertension. Falsely elevated readings can be obtained when the bladder is too short, and the error is magnified if the cuff is also too narrow. The diastolic reading is taken at the level when sounds disappear (Korotkoff phase V). A careful, complete history should be obtained and a physical examination performed in all patients before antihypertensive therapy is started. Discussion of family history should include mention of familial diseases associated with secondary hypertension, including familial renal disease, polycystic kidney disease (see Chapter 115), medullary thyroid cancer (see Chapter 265), pheochromocytoma (see Chapter 241), and hyperparathyroidism (see Chapter 264). All current medications should be considered, in particular, agents that may exacerbate existing hypertension or antagonize or adversely interact with drug therapy (see Table 55-3). The physical examination should include height; weight; funduscopic examination; verification of hypertension in the contralateral arm; a careful examination of the neck, abdomen, and extremities for bruits; neurologic assessment; and if coarctation of the aorta is suspected (see Chapter 57), blood pressure measurement in the leg. Criteria for both treatment and prognosis are affected by the presence of target organ disease. Pre-treatment laboratory tests can be restricted to those generally performed as part of a routine medical checkup evaluation: complete blood count; urinalysis; serum potassium, sodium, and creatinine levels; fasting blood glucose; low- and high-density lipoprotein cholesterol levels; and a 12-lead electrocardiogram. These tests help assess the presence and severity of target organ disease and other cardiovascular risk factors and can be used as a baseline for monitoring the effects of antihypertensive treatment. Serial electrocardiograms and echocardiograms (see Chapters 42 and 43) may help assess the effects of hypertension and antihypertensive treatment on the heart, but their clinical utility in managing an individual patient is unclear. Consensus guidelines stratify hypertensive patients into risk groups for therapeutic decisions (Table 55-5) (Table Not Available). For those with stage 2 or stage 3 hypertension, immediate drug therapy is warranted. Risk group B includes patients with hypertension who do not have clinical cardiovascular disease or target organ damage but who do have one or more of the major cardiovascular risk factors other than diabetes mellitus. If multiple risk factors are present, immediate drug therapy should be considered. Lifestyle modification and management of reversible risk factors should accompany drug treatment.
Symptoms of hypertensive crisis include headache antibiotic resistance united states generic flagyl 500mg without prescription, malaise virus respiratory order flagyl 500 mg without a prescription, dizziness 700 bacteria in breast milk buy generic flagyl 400mg on-line, blurred vision antibiotics mrsa cheap flagyl 500mg with visa, chest pain, palpitations, and shortness of breath. Clinical and laboratory signs of hypertensive crisis include funduscopic changes (arteriolar narrowing, arteriovenous nicking, hemorrhage, exudates, papilledema); changes related to renal insufficiency; microangiopathic hemolytic anemia; signs of left ventricular dysfunction (S4 and S3 gallops, jugular venous distention, cardiomegaly, tachycardia, pulmonary edema); and evidence of increased intracranial pressure (confusion, somnolence, stupor, neurologic deficits, seizures). Patients with hypertensive emergencies may have stroke, subarachnoid hemorrhage, intracranial hemorrhage, aortic dissection, left ventricular failure, or myocardial ischemia. Chest radiography, electrocardiography, complete blood cell count with blood smear, and renal profiles and urinalysis should be performed. If by history, physical examination, or laboratory data the patient has evidence of ongoing (new or worsening) target organ damage, the patient should be considered to be having a medical emergency. However, after initiating maintenance therapy or adjusting existing therapeutic regimens, early follow-up is essential to ensure the efficacy of and compliance with prescribed therapy. Captopril and conventional treatment did not differ in efficacy in preventing cardiovascular morbidity and mortality. Detailed recommendations for diagnosis and pharmacologic and non-pharmacologic treatment of systemic hypertension. A meta-analysis of randomized trials of antihypertensive therapy showing greater short-term benefit in elderly than younger patients. A meta-analysis of 18 long-term randomized trials of antihypertensive drugs including 48,220 individuals treated for an average of 5 years showed significant treatment-related reductions in stroke, coronary heart disease, congestive heart failure, and total and cardiovascular mortality. Placebo-controlled trial demonstrating that treating isolated systolic hypertension with the intermediate-acting calcium channel blocker nitrendipine as the beginning drug reduced total and non-fatal stroke by 42% and 44%, respectively, after only 2 years of follow-up. The study was stopped early because of this large benefit; other cardiovascular end points showed improvement, which in many cases did not attain statistical significance, perhaps because of the abbreviated follow-up period. Alpert Pulmonary hypertension is defined as pressure within the pulmonary arterial system elevated above the normal range. These entities lead to changes in pulmonary circulatory function that elevate pulmonary pressure. For example, exercise-induced increases in cardiac output result in moderate elevations in pulmonary arterial pressure. Moreover, increased resistance in any of the various vascular zones of the pulmonary circulation can lead to pulmonary hypertension. For example, increased pulmonary arteriolar resistance in a patient with congenital heart disease causes severe, chronic pulmonary hypertension. Therefore, normal mean pulmonary arterial pressure is only 12 to 15 mm Hg (Table 56-1). This compares with a pressure drop of approximately 90 mm Hg across the systemic circulation. The distensibility and low vascular resistance of the pulmonary circulation are the result of the thin muscular medial layer of the pulmonary arterioles. The lower resistance and hence pressure within the pulmonary circuit, compared with its systemic counterpart, are reflected in the right ventricle, which is less than half as thick as the left ventricle. This relationship is expressed in the following formula: Pulmonary hypertension develops when flow or resistance to flow across the pulmonary vascular bed increases. As already noted, a variety of physiologic and pathophysiologic mechanisms can lead to such increases in pulmonary pressures. This fall in vascular resistance is due in part to arteriolar vasodilation and in part to opening or recruitment of previously closed microvessels. Another "physiologic" cause of pulmonary hypertension is hypoxia, which is associated with ascent from sea level. The pulmonary hypertension of altitude results from hypoxic arteriolar vasoconstriction. Other factors that may affect pulmonary pressures are blood viscosity, intrathoracic pressure, and endogenous vasoactive substances. Therefore, marked increases in the number of red blood cells per cubic milliliter of blood produce elevations in blood viscosity that can cause pulmonary hypertension. Another factor that can increase pulmonary arterial pressure is elevation in intrathoracic pressure, which is directly transmitted to the pulmonary vasculature. Dysfunctional pulmonary vascular endothelium plays an important role in the pathophysiology of pulmonary hypertension. Normal endothelium releases growth factors and cytokines that regulate vascular smooth muscle tone, proliferation, and migration. Dysfunctional endothelium leads to vasoconstriction and intravascular thrombus formation. A variety of pulmonary vascular endothelial abnormalities have been demonstrated in patients with pulmonary hypertension, including impaired endothelium-dependent vasodilatation, decreased elaboration of vasodilating nitric oxide and prostacyclin, elevated circulating levels of the potent vasoconstrictor endothelin, and increased levels of various clotting factors such as fibrinopeptide A, Factor Vlllc, von Willebrand factor, and plasminogen activator inhibitor. Pulmonary hypertension can be divided into three classes based on the location of the abnormal increase in pulmonary vascular resistance: precapillary, passive, and reactive. Patients with increased pulmonary arteriolar and/or arterial resistance are classified as having precapillary pulmonary hypertension. Pulmonary arterial pressure is increased, but pulmonary capillary wedge and pulmonary venous pressures are normal. The gradient between the mean pulmonary arterial pressure and the pulmonary capillary or pulmonary venous pressures is greater than 12 mm Hg. Examples include hypoxic pulmonary hypertension (increased arteriolar resistance) and pulmonary embolism (increased arterial resistance) (see Chapter 84). Individuals with increased pulmonary venous pressure secondarily causing pulmonary arterial hypertension are said to exhibit passive pulmonary hypertension because the increase in pulmonary arterial pressure occurs passively-without active pulmonary arterial vasoconstriction. The gradient between the mean pulmonary arterial pressure and the pulmonary capillary or pulmonary venous pressures is less than or equal to 12 mm Hg. The third form of pulmonary arterial hypertension is termed reactive and contains elements of both precapillary and passive pulmonary hypertension. Reactive pulmonary hypertensive patients have elevated pulmonary venous pressure as well as pulmonary arteriolar vasoconstriction. Patients with reactive pulmonary arterial hypertension usually have long-standing mitral stenosis. Increased resistance to blood flow through the pulmonary arterial circulation can be the result of large pulmonary emboli or loss of pulmonary arterial cross-sectional area from various disease entities. Increased pulmonary arteriolar resistance is commonly the result of hypoxia and/or acidosis, which cause pulmonary arteriolar vasoconstriction. Patients with congenital heart disease with left-to-right shunts can develop markedly increased pulmonary arteriolar vascular resistance through a pathophysiologic process that begins as vasoconstriction and ends with obliteration and loss of pulmonary microvessels. Primary pulmonary hypertension is the result of abnormal increases in pulmonary arteriolar tone. The resultant pulmonary hypertension in these patients leads to thickening of the intimal and medial layers of the pulmonary arterioles, which, in turn, further 275 exacerbates the degree of pulmonary hypertension. A vicious spiral is thereby engendered in which ever-increasing levels of pulmonary arterial hypertension lead to further arteriolar thickening, which leads to worsening pulmonary hypertension. This pathophysiologic sequence is also seen in patients with congenital heart disease who develop pulmonary vascular disease and pulmonary hypertension. Increased pulmonary venous pressure and vascular resistance are other causes of pulmonary hypertension: increased pulmonary venous pressure leads to augmented pulmonary capillary and pulmonary arterial diastolic pressure. Pulmonary arterial systolic and mean pressure must increase in this setting to maintain forward cardiac output. Disease entities that increase pulmonary venous pressure and resistance to blood flow include pulmonary venous thrombosis. Individuals with more severe pulmonary hypertension usually complain of dyspnea on exertion secondary to exercise-induced decreases in cardiac output and increases in pulmonary arterial pressure. Other symptoms can include easy fatigability, exertional chest discomfort and/or syncope, cough, hemoptysis, and, rarely, hoarseness secondary to compression of the left recurrent laryngeal nerve by a dilated left pulmonary artery. Doppler studies predict with considerable accuracy the level of pulmonary arterial systolic and mean pressures. Note the marked enlargement of the main pulmonary arteries (+) and the dearth of peripheral pulmonary arteries ("pruning"). A number of radionuclide diagnostic studies are useful in patients with known or suspected pulmonary hypertension.
Discount 400mg flagyl with amex. Antimicrobial Activity ASTM 2149.
Measurement of Respiratory Muscle Strength Respiratory muscle strength can be assessed by measuring with a manometer the maximum airway pressures developed during inspiration from a low lung volume and expiration from a high lung volume antibiotic 875mg 125mg discount flagyl 250 mg on-line. Healthy adults have a maximum inspiratory pressure greater than 100 cm H2 O and a maximum expiratory pressure greater than 150 cm H2 O antimicrobial medicines generic flagyl 400 mg otc. A maximum inspiratory pressure that is less negative than - 30 cm H2 O suggests the need for ventilatory support 3m antimicrobial mask flagyl 200 mg visa, whereas a value that is more negative than - 30 cm H2 O antibiotic medical definition 200mg flagyl free shipping, especially if it can be sustained for 3-5 seconds, correlates with successful weaning from mechanical ventilation. Measurement of the Work of Breathing As noted earlier, the work of breathing is the product of the transpulmonary pressure (the difference between airway and pleural pressure) multiplied by the tidal volume (the V T). Although pleural pressure is impractical to measure and varies regionally, it can be approximated by measuring pressure in the esophagus with a balloon. Changes in this pressure can be used to compute the work of breathing in spontaneously breathing and mechanically ventilated patients. Central cyanosis reflects the presence of 3 g/dL or more of reduced, that is, deoxygenated, hemoglobin. However, the blue discoloration of tissues caused by deoxygenated hemoglobin also may be caused by dyshemoglobins such as sulfhemoglobin. Furthermore, clinicians vary in their ability to detect cyanosis when it actually occurs. Arterial Blood Gas Analysis the systemic arterial O2 tension (Pa O2) obtained by arterial blood gas analysis is the standard for assessing the adequacy of arterial oxygenation. The normal Pa O2 at sea level is approximately 488 Figure 92-4 Normal oxyhemoglobin dissociation curve showing the relationship between the systemic arterial O2 saturation (Sa O 2), tension (Pa O 2), and content (Ca O 2). However, the Pa O2 is inversely correlated with age, as expressed in the following equation: However, Equation 6 does not correct for the effects of barometric pressure. This difference, the P (A - a) O2, increases to 30 mm Hg with age and increases further with respiratory disease. The word hypoxemia is used to describe a Pa O2 of less than normal; hypoxemic respiratory failure, also called failure of arterial oxygenation, exists when the Pa O2 is below 50-60 mm Hg. Even if the Pa O2 of a patient with hypoxemic respiratory failure is normalized by the administration of supplemental O2, O2 exchange in the lungs may remain abnormal. It can be calculated with the equation: where Q this the cardiac output, and C c O2, Ca O2, and Cv O2 are the O2 contents of end-capillary, arterial, and mixed venous blood, respectively. A simpler but less precise way of estimating Q S/Q this to divide the P (A - a) O2 by 20. Measurement of Systemic Arterial Saturation the saturation of hemoglobin by O2 in systemic arterial blood (Sa O2) is related to the Pa O2 by the O2 hemoglobin dissociation curve. Hemoglobin is almost 100% saturated at a Pa O2 of 100 mm Hg, and its saturation cannot be significantly increased by increasing the Pa O2. The Sa O2 will increase somewhat, signifying that less O2 is available to the tissues at a given Pa O2, if the O2 hemoglobin dissociation curve is shifted to the left by alkalosis or hypothermia. Conversely, the Sa O2 will decrease, signifying O2 release to the tissues, if the curve is shifted to the right by acidosis and hyperthermia. In many arterial blood gas analyses, the Sa O2 is estimated from the Pa O2 using an ideal, unshifted O2 hemoglobin dissociation curve. Nevertheless, the Sa O2 can also be measured with co-oximeters that record the absorbency of light passing through a dilute solution of hemoglobin. Co-oximeters use several wavelengths of light and can determine not only the percentages of oxygenated hemoglobin and reduced hemoglobin but also the percentages of carboxyhemoglobin, methemoglobin, and sulfhemoglobin. The pulse oximeter records the absorbency of light passing through a pulsatile tissue bed such as a fingertip (see Chapter 91). The absorption characteristics of oxgenated hemoglobin and reduced hemoglobin are different at the two wavelengths of light used. Pulse oximetry accurately measures Sa O2 values above 80% in persons with adequate peripheral arterial flow. This technique is particularly helpful in patients who are hemodynamically stable and in whom a non-shifted O2 hemoglobin dissociation curve allows good correlation between Sa O2 and Pa O2. The Sa O2 measured by pulse oximetry does not account for hemoglobin that is saturated by substances other than O2, such as carbon monoxide; because of this, the Sa O2 is falsely elevated in patients with carbon monoxide poisoning. Nevertheless, the accuracy, ease, and low expense of pulse oximetry make it a useful substitute for analysis of Pa O2 in many situations. For example, the presence of normal skin color and warmth suggest an adequate peripheral flow of oxygenated blood in some circumstances. Such adequacy is also suggested by normal capillary refill, in which skin color returns to baseline 2-3 seconds after the skin is blanched. Nevertheless, although these findings may help exclude significant hypovolemia or impairment of cardiac output, which are associated with increased systemic vascular resistance, they do not exclude sepsis and other processes in which systemic vascular resistance is decreased. When skin findings are unreliable, O2 delivery and utilization may be assessed in other organs where blood supply is maintained despite hypoperfusion elsewhere. In this regard, the onset of confusion or obtundation in a previously healthy patient may signify a significant decrease in cerebral oxygenation. Thus, the Ca O2 (mL O2 /dL blood) can be calculated from the following equation: where 1. At a normal Sa O2 of approximately 100%, a Pa O2 of 100 mm Hg, and a hemoglobin concentration of 14 g, the Ca O2 is 20 mL O2 /dL of blood. Cardiac output can be measured with the thermodilution technique using a pulmonary artery catheter. With this technique, a bolus of cold liquid, usually dextrose in water, is rapidly injected into the right atrium through the proximal catheter port, causing the negative heat to be diluted by mixing with blood as it passes into the pulmonary artery. A thermistor senses the temperature of blood on passing the distal catheter port, and the temperature change is used to compute cardiac output, which averages 5 L/min in healthy persons. If arterial O2 content is normal, the amount of O 2 delivered to the tissues normally averages 1000 mL O2 /min. Measurement of Mixed Venous Oxygen Saturation Placement of a pulmonary artery catheter allows the collection of samples for determination of the O2 tension, saturation, and content of mixed venous blood. The saturation can also be measured continuously with an oximetric pulmonary artery catheter containing fiberoptic bundles that transmit and receive light from the catheter tip. Normal persons have a mixed venous O2 saturation of approximately 75%, which corresponds to a mixed venous O2 tension of 40 mm Hg on an unshifted O2 hemoglobin dissociation curve. Reductions in mixed venous O2 saturation to below 60%, corresponding to mixed venous O2 tension values of less than 28 mm Hg, are associated with a severely impaired amount of O2 delivered to the tissues. Indeed, anaerobic metabolism commonly develops when the mixed venous O2 saturation falls below 50%. Although a low mixed venous O2 saturation may be clinically alarming, inadequate O2 transport and utilization may exist in the face of normal or supranormal values. For example, a mixed venous O2 saturation >80% may be seen in sepsis, when the tissues either cannot extract O2 from the blood or perform aerobic metabolism, or when blood is redistributed to metabolically inactive organs such as the skin. Because the mixed arterial content is usually 20 mL/dL, the normal difference is 5 mL O2 /mL blood. With this value and a cardiac output of 5 L/min, total body O2 consumption averages 250 mL O2 /min in healthy persons. It reveals, for example, that normally only 25% of the O2 in systemic arterial blood is extracted by the tissues, leaving a large O2 reserve. Patients characteristically call on this reserve when the amount of O 2 delivered to the tissues decreases because of a fall in cardiac output, a fall in the content of O2 in systemic arterial blood (and its major components, Sa O2 and hemoglobin), or both. Nevertheless, a shift to anaerobic metabolism generally occurs when more than 50% of the O2 is extracted, and lactic acidosis may result. Measurement of Other Indicators of Oxygen Transport and Utilization Clinicians commonly monitor serum lactate levels as a sign of the development and progression of anaerobic metabolism. This approach is supported by studies demonstrating that lactate levels above 2 mEq/L correspond to a mixed venous O2 tension less than 28 mm Hg with an increased mortality rate among critically ill patients. Nevertheless, elevated lactate levels may result from decreased lactate degradation rather than increased production, and they should be interpreted with caution. Assessment of oxygenation of the gastrointestinal tract may provide an early indication of inadequate tissue perfusion in the critically ill. Such assessment can be derived from measurement of gastric intramucosal pH by a saline-filled balloon passed into the lumen of the stomach.
Because of stasis of blood in dilated hypokinetic cardiac chambers treatment for dogs eating poop generic flagyl 400mg, patients with a dilated cardiomyopathy are at increased risk of cardiac thrombi and embolic events 8hr infection control course flagyl 250 mg without prescription. Yet antibiotic resistance science project order 400 mg flagyl with amex, it is unclear whether all patients with a depressed ejection fraction should receive treatment with anticoagulant drugs antibiotics history order 250 mg flagyl, even if they are known to harbor a cardiac thrombus. Most cardiac thrombi detected by echocardiography do not embolize, and most embolic events are related to thrombi that were not visualized. Anticoagulation is recommended primarily for patients with a previous embolic event or atrial fibrillation. Drugs To Be Avoided in Patients with Heart Failure Patients with heart failure can improve dramatically after the withdrawal of drugs that are known to affect cardiac function adversely or that interact unfavorably with drugs of established benefit. Prostaglandins play an important role in circulatory homeostasis and in the action of many drugs used to treat heart failure. These substances are endogenous vasodilators that act to unload the heart when peripheral vessels are constricted and can support glomerular filtration when renal perfusion is compromised. As a result, most patients with heart failure should not receive non-steroidal anti-inflammatory agents. Whether the recommendation to avoid inhibitors of prostaglandin synthesis applies to aspirin remains controversial. Aspirin is widely prescribed to patients with heart failure, either to reduce the risk of recurrent myocardial ischemic events in patients with coronary artery disease or to decrease the frequency of systemic embolic events in patients with normal coronary arteries. Although calcium channel blockers are peripheral vasodilators, these agents have not improved the symptoms of heart failure or enhanced exercise tolerance. Instead, the short- and long-term administration of these drugs has caused serious adverse cardiovascular reactions, including profound hypotension, worsening heart failure, pulmonary edema, and cardiogenic shock. These deleterious responses have been observed with short- or long-acting formulations of the same drug. As a result, clinicians should not use calcium channel blockers for the treatment of heart failure, and most calcium channel blockers should be avoided for the treatment of angina, atrial fibrillation, or hypertension in patients with heart failure. Of the available agents, only amlodipine has strong evidence supporting its safety in patients with advanced disease. Antiarrhythmic agents can suppress ventricular arrhythmias in patients with heart failure, but these agents have not been shown to reduce the risk of sudden death. Instead, the short- and long-term administration of these drugs has caused serious adverse cardiovascular reactions, including worsening heart failure, life-threatening proarrhythmia, and death. As a result, antiarrhythmic therapy should not be used to treat patients with heart failure who have asymptomatic ventricular arrhythmias, regardless of their frequency or complexity. Antiarrhythmic drugs may be useful for patients with rapid atrial fibrillation or for those with hemodynamically destabilizing ventricular tachycardia or ventricular fibrillation. Such toxicity has been reported with all types of agents of this class (except for digitalis), whether these have been prescribed orally or intravenously or administered continuously or intermittently. Because of the lack of data demonstrating efficacy and important concerns about toxicity, the use of intermittent intravenous positive inotropic therapy cannot be recommended as a long-term treatment strategy, even in patients with end-stage heart failure. The major syndromes requiring hospitalization include (1) fluid overload resistant to orally administered diuretics. Each syndrome represents an exaggerated expression of each of the pathophysiologic mechanisms that play a role in the evolution of heart failure; that is, refractory edema reflects excessive sodium and water retention; acute pulmonary edema is the result of extreme vasoconstriction; and refractory symptoms associated with systemic hypoperfusion are the ultimate consequence of contractile failure. These syndromes share a common therapeutic approach: that is, because of their immediate life-threatening nature, physicians must rely on short-term hemodynamic interventions to achieve clinical stability as rapidly as possible. If the syndromes are the result of changes in diet or medications or the advent of a treatable complicating illness. However, if these syndromes represent the end-stage of a terminal disease that is refractory to medical therapy, hemodynamic support must be continued until a definitive mechanical solution can be devised. In either case, neurohormonal activation is not a therapeutic target in patients who are hospitalized for the treatment of decompensated heart failure. Indeed, by supporting cardiac contractility and systemic blood pressure, the activation of the sympathetic nervous system and renin-angiotensin system may help to maintain circulatory homeostasis in acutely ill patients. Fluid Overload Refractory to Oral Diuretics (Refractory Peripheral Edema) Patients with heart failure are frequently hospitalized for the treatment of edema that persists despite the use of diuretics. These patients typically present with a marked increase in body weight, associated with pleural effusions, ascites, and massive peripheral edema. The degree of fluid retention can become so severe that the edema itself becomes incapacitating and may require mechanical removal of fluid for relief of symptoms. However, in some patients, the occurrence of refractory edema is indicative of advancing right and left ventricular failure. By causing mesenteric congestion, right ventricular failure can impair the rate of absorption of diuretics; by causing renal hypoperfusion, left ventricular failure can impede the delivery of diuretics to active sites in the renal tubules. As a result, as heart failure advances, patients become increasingly resistant to the effects of diuretic drugs and require larger and larger doses to achieve a therapeutic response. Management of Refractory Peripheral Edema Several strategies should be considered in the management of patients with refractory edema. Non-steroidal anti-inflammatory drugs, which can decrease the efficacy and increase the risk of diuretics, should be withdrawn. If the patient fails to respond to the intravenous administration of large doses of furosemide, the physician may add a second diuretic with a different renal tubular site of action. A combination of two diuretics can produce a dramatic increase in urine output, but such a regimen is commonly accompanied by striking (and occasionally life-threatening) degrees of hypokalemia. If a combination of intravenous furosemide and oral metolazone proves ineffective, these diuretics should be co-administered with drugs that increase renal blood flow. Finally, if the edema becomes refractory to all pharmacologic interventions, hemofiltration or peritoneal dialysis may be useful in restoring fluid balance in selected patients. Regardless of the severity of fluid retention, every effort should be made to achieve dry weight, even if achievement of this goal requires a prolonged hospitalization. Patients discharged prematurely with residual edema due to an inadequate diuresis are commonly readmitted to the hospital for refractory edema within several weeks. In contrast, patients who achieve dry weight frequently become responsive to conventional treatments for heart failure and have a lower risk of recurrent hospitalization. Pulmonary Congestion (Acute Pulmonary Edema) One of the most common clinical presentations of advanced left ventricular failure is the syndrome of pulmonary congestion. These patients complain of dyspnea at rest and have pulmonary rales on physical examination. Pulmonary congestion may be the first evidence of heart failure in patients without a history of cardiac disease; it may appear in patients who are already hospitalized for an acute cardiac disorder. If severe, abrupt, and accompanied by clinical evidence of sympathetic overactivity (tachycardia, diaphoresis and vasoconstriction), the syndrome is designated as acute pulmonary edema. Acute pulmonary edema may also be triggered by non-cardiac disorders, including direct injury to the alveolar-capillary membrane, high-altitude stress, catastrophes of the central nervous system, narcotic overdose, or pulmonary embolism. Regardless of its cause, pulmonary edema reflects the transudation of fluid into the alveolar space and arises from an imbalance in the factors that regulate the transport of fluid from the pulmonary microcirculation to the interstitial space of the lung. When the cause of the syndrome is cardiac, pulmonary edema results from the rapid onset of intense peripheral vasoconstriction that leads to a marked increase in pulmonary venous pressures. The profound constriction of systemic arteries and veins causes a sudden and dramatic redistribution of blood from peripheral reservoirs to the pulmonary circuit, causing the pulmonary capillary hydrostatic pressure in the lung to exceed the capillary colloid osmotic pressure. However, the transudation of fluid into the alveoli cannot occur if pulmonary blood flow is impaired; thus, patients with an elevated pulmonary vascular resistance or depressed right ventricular function rarely develop acute pulmonary edema. Management of Pulmonary Edema Several general measures are advisable for most patients with pulmonary congestion. Every effort should be made to identify an underlying precipitating factor, because its correction is often critical to the success of treatment. Patients usually feel most comfortable resting in bed in the upright position with the legs dependent. Special attention should be devoted to maintaining adequate oxygenation, which can be achieved by increasing the concentration of 225 inspired oxygen or (if necessary) by endotracheal intubation and mechanical ventilation. Given the importance of peripheral vasoconstriction in the pathogenesis of pulmonary edema, pharmacologic dilation of peripheral vessels represents the critical element in any successful approach to management. This goal can be achieved with the use of (1) morphine; (2) loop diuretic drugs. Because of the need for rapid and reliable treatment, these interventions are generally administered intravenously. Morphine remains the most effective single agent for the treatment of acute cardiogenic pulmonary edema. The drug acts specifically to antagonize the peripheral vasoconstrictor effects of the sympathetic nervous system; the resultant vasodilatation leads to an immediate and dramatic decline in pulmonary arterial and venous pressures, leading directly to symptomatic improvement. The magnitude of venodilation produced by the drug in the limbs is insufficient to explain its effects on pulmonary flow and pressures; instead, morphine appears to act primarily to increase the pooling of blood in the splanchnic circulation.