




|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Prakashchandra M. Rao, MD, FACS
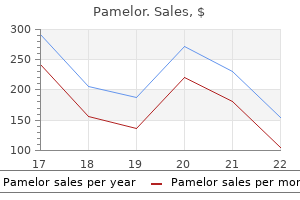
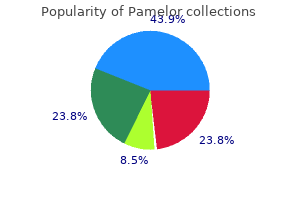
Glanders is associated with close contact with horses or other equines and is caused by B anxiety symptoms before sleep purchase pamelor 25 mg without prescription. Outbreaks have been traced to drinking water systems and rarely to cooling towers anxiety nos icd 10 generic pamelor 25mg with visa. Levofloxacin infection may be an alternative anxiety symptoms losing weight purchase pamelor 25 mg with amex, but Ticarcillin/clavulanate there is little published (3 anxiety yoga poses purchase pamelor 25 mg with mastercard. Diagnosis the use of Legionella testing-especially the Legionella urinary antigen test-is recommended for all pts with community-acquired pneumonia. Among immunocompetent hosts, mortality can approach 31% without treatment but ranges from 0 to 11% with appropriate and timely therapy. Epidemiology Brucellosis is transmitted via ingestion, inhalation, or mucosal or percutaneous exposure; the disease in humans is usually associated with exposure to infected animals or their products in either occupational settings. The global prevalence of brucellosis is unknown because of difficulties in diagnosis and inadequacies in reporting systems. Diagnosis Laboratory personnel must be alerted to the potential diagnosis to ensure that they take precautions to prevent occupational exposure. Single titers of 1:160 and 1:320 are diagnostic in nonendemic and endemic areas, respectively. Pts present with signs and symptoms similar to those of pneumonia of other etiologies. This form is the result of a large inoculum or a preexisting compromising condition. Diagnosis the diagnosis of tularemia is most frequently confirmed by serology, although up to 30% of pts infected for 3 weeks have negative results in serologic tests. As the rodent population succumbs to disease, fleas (the arthropod vector) search for a new host and can transmit the bacteria to humans. Persons >40 years old are at greater risk, although this form of the disease can occur in all age groups. Subcutaneous masses or nodules, ulcerated plaques, and verrucous growths also occur. Even if incubated for prolonged periods (up to 6 weeks), blood cultures are positive in only ~25% of cases. In 2006, ~290,000 people-most of them in Southeast Asia and Africa-died of tetanus; maternal and neonatal infections accounted for ~60% of these deaths. As the disease progresses, painful muscle spasms develop and can sometimes be strong enough to cause crush fractures. Because natural disease does not induce immunity, recovering pts should be immunized. For persons who have received a complete primary course in childhood but no further boosters, two doses at least 4 weeks apart are recommended. Prognosis A shorter incubation period (time from wound to first symptom) or onset period (time from first symptom to first generalized spasm) is associated with worse outcome. Clinical Manifestations Botulism occurs naturally as four syndromes: (1) food-borne illness; (2) wound infection; (3) infant botulism; and (4) adult intestinal toxemia, which is similar to infant botulism. The disease presents as symmetric cranial nerve palsies (diplopia, dysarthria, dysphonia, ptosis, and/or dysphagia) followed by symmetric descending flaccid paralysis that may progress to respiratory arrest and death. Nausea, vomiting, and abdominal pain may precede or follow the onset of paralysis; constipation due to paralytic ileus is nearly universal. This form in infants has been associated with contaminated honey; thus honey should not be fed to children <12 months of age. Adult pts typically have some anatomic or functional bowel abnormality or have a bowel flora disrupted by recent antibiotic use. The definitive test is the demonstration of the toxin in clinical specimens (serum, stool, gastric aspirates, wound material) with a mouse bioassay. In the United States, 95% of pts recover fully, but this process may take many months. Epidemiology and Clinical Manifestations Life-threatening clostridial infections range from intoxications. Diagnosis and treatment of clostridial infection should be based on clinical signs and symptoms, given that clostridia are isolated with equal frequency from both suppurative and well-healing wounds. Neutropenia (of any origin) is also associated with clostridial bloodstream infection. Most pts develop severe pain, crepitus, brawny induration with rapid progression to skin sloughing, violaceous bullae, and marked tachycardia. Disease initially presents as excruciating pain at the affected site and the development of a foul-smelling wound containing a thin serosanguineous discharge and gas bubbles. Confusion, extreme pain in the absence of trauma, and fever should heighten suspicion. Diagnosis Isolation of clostridia from clinical sites does not in itself indicate severe disease. Hyperbaric oxygen therapy may be considered after surgery and antibiotic treatment have been initiated. Bacterial synergy, bacterial virulence factors, and mechanisms of abscess formation are factors involved in the pathogenesis of anaerobic infections. Clinical Manifestations the clinical presentation of anaerobic infections depends, in part, on the anatomic location affected. Pts have a sore throat, foul breath, fever, a choking sensation, and tonsillar pillars that are swollen, red, ulcerated, and covered with a gray membrane. Bacterial aspiration pneumonia is associated with a depressed gag reflex, impaired swallowing, or altered mental status; anaerobic lung abscess usually arises from a dental source. Anaerobes, typically in combination with coliforms, are isolated from most women with genital tract infections. The major anaerobic pathogens are Bacteroides fragilis, Prevotella species (bivia, disiens, melaninogenica), anaerobic cocci, and Clostridium species. These infections most frequently occur at sites prone to contamination with feces or with upper airway secretions. Should generally be used in conjunction with drugs active against aerobic or facultative organisms. Actinomycosis is the leading cause of anaerobic bone infections worldwide; Fusobacterium species are the most common anaerobic cause of septic arthritis. Diagnosis the three critical steps in successfully culturing anaerobic bacteria from clinical samples are (1) proper specimen collection, with avoidance of contamination by normal flora; (2) rapid specimen transport to the microbiology laboratory in anaerobic transport media; and (3) proper specimen handling. A foul odor is often indicative (and nearly pathognomonic) of an anaerobic infection. Accordingly, the recommended regimens include clindamycin, a -lactam/-lactamase inhibitor combination, or metronidazole in combination with a drug active against microaerophilic and aerobic streptococci. Treatment should also cover the aerobic gram-negative flora, including enterococci. Superinfection with resistant gram-negative facultative or aerobic bacteria should also be considered. The risk of disease is greater than usual among persons who have deficient cell-mediated immunity-e. Pathogenesis Pneumonia and disseminated disease follow inhalation of fragmented bacterial mycelia.
In a general pregnant population anxiety symptoms constipation cheap 25mg pamelor free shipping, the authors noted moderate evidence of a pooled sensitivity of 0 anxiety symptoms breathing generic pamelor 25mg fast delivery. In a high-risk pregnant population anxiety symptoms forum discount pamelor 25mg without a prescription, the authors noted moderate evidence of pooled sensitivities for trisomies 21 and 18 of 0 anxiety symptoms pain 25 mg pamelor with amex. Sensitivity was lower in twin than singleton pregnancies, reduced by 9% for Down, 28% for Edwards, and 22% for Patau syndrome. Pooled sensitivity was also lower in the first trimester of pregnancy in studies of the general obstetric population. Aneuploidy was confirmed in 720/781 cases positive for trisomy 21, 167/218 cases positive for trisomy 18, and 22/67 cases positive for trisomy 13. Nine false negatives were identified, including six cases of trisomy 21 and three of trisomy 18. The authors reported no significant difference in test performance between 72,382 high-risk and 40,287 low-risk pregnancies (sensitivity, 99. The major factors contributing to false-positive and false-negative results were maternal copy number variant and fetal/placental mosaicism. Determination of the birth outcome was based on diagnostic genetic testing or newborn examination. Of 18,955 women who were enrolled, results from 15,841 were available for the primary analysis. Fifty-four cases did not get results because of lost sample (n=1), low fetal fraction (n=38), and test failure (n=15). Samples were received from 31,030 patients, 30,705 met study criteria and 28,739 passed quality-control metrics and received a report detailing aneuploidy risk. Samples that passed quality control were analyzed for trisomy 21, trisomy 18, trisomy 13, and monosomy X. Results were reported as high or low risk for fetal aneuploidy for each chromosome. In all, 507 patients received a high-risk result for any of the 4 tested conditions (324 trisomy 21, 82 trisomy 18, 41 trisomy 13, 61 monosomy X; including one double aneuploidy case). Within the 17,885 cases included in follow-up analysis, 356 were high risk, and outcome information revealed 184 (51. However, the authors also noted that the main limitation of the study is the incomplete followup data, particularly on low-risk patients. With a total of 681 pregnancies included, overall sensitivity was 125/125 (100%) and specificity 552/556 (99. MaterniT21 In a prospective multicenter observational study of pregnant women at high risk for fetal aneuploidy, Porreco et al. There were 137 fetuses with trisomy 21, 39 with trisomy 18, and 16 with trisomy 13. There were no false-negative results for trisomy 21, three for trisomy 18, and two for trisomy 13. Despite high sensitivity, there was modest positive predictive value for the small number of common sex chromosome aneuploidies because of their very low prevalence rate. Among a cohort of 4664 high-risk pregnancies, maternal plasma samples were tested from 25 twin pregnancies (17 euploid, five discordant and two concordant for Down syndrome; one discordant for trisomy 13) and two euploid triplet pregnancies. Seven twin pregnancies with Down syndrome, one with trisomy 13, and all 17 twin euploid pregnancies were correctly classified [detection rate 100%, false positive rate 0%], as were the two triplet euploid pregnancies. Further studies, with larger patient populations, are needed to confirm these results. Test results were compared to those obtained after chorionic villus sampling or amniocentesis. Of the remaining cases, 218 (5%) fetuses were diagnosed with trisomy 21 based on the results of invasive testing. Fetal karyotyping was compared with an internally validated, laboratory-developed test based on next-generation sequencing. This method can substantially reduce the need for invasive diagnostic procedures and attendant procedure-related fetal losses. Sixty-two pregnancies with trisomy 18 and 12 with trisomy 13 were included in the analysis. The diagnostic accuracy was validated against full karyotyping, using prospectively collected or archived maternal plasma samples. Results were available from 753 pregnancies with the 8-plex sequencing protocol and from 314 pregnancies with the 2-plex protocol. The performance of the 2-plex protocol was superior to that of the 8-plex protocol. With the 2-plex protocol, trisomy 21 fetuses were detected at 100% sensitivity and 97. In all, 449 samples remained: 39 trisomy 21 samples were correctly classified; one sample was misclassified as trisomy 21. The authors reported that extending the scope of previous reports, these results warrant clinical validation in a larger multicenter study. Pregnancy outcome was obtained by genetic counselors and /or Quest diagnostics client services. Further studies are needed to determine the clinical validity of sequence-based fetal aneuploidy testing in this patient population. Another study, which involved 6123 patients with blood samples submitted for testing with the Verifi Prenatal Test, 155 (2. Unclassifiable results were obtained in up to 1% of cases for each of the chromosomes analyzed. Follow-up information was not available for the remaining cases at the time of publication (Futch et al. Blood samples were collected from 2,882 women undergoing invasive prenatal diagnostic procedures. The authors reported high sensitivity and specificity for the detection of trisomies 21, 18, 13 in women with singleton pregnancies at an increased risk for aneuploidy. Further studies are needed to build confidence in the diagnostic performance of the test in low-risk populations and in multiple gestations. Existing algorithms focus on the detection of fetal trisomy 21 (T21); however, these same algorithms have difficulty detecting trisomy 18 (T18). Blood samples were collected from 1014 patients prior to undergoing an invasive prenatal procedure. The classification process was then evaluated on an independent test set of 48 samples with 27 abnormal karyotypes. Sequencing of the independent test set led to 100% correct classification of T21 (13 of 13) and T18 (8 of 8) samples. Results were reported based on the presence or absence of the Y chromosome fragments. For the 727 disomic pregnancies, 725 were correctly identified as low-risk for sex chromosome aneuploidy (99. However, the observed positive predictive value in this group may not be applicable to routine prenatal screening populations. The same group of authors updated the meta-analysis with data from 37 studies published since the initial review. The overall incidence of aneuploidy was higher than anticipated for the low or mixed risk population. When studies were broken out by technology, the sample sizes for the different types of tests was individually low. This suggests that more data is needed to determine the positive predictive value for the low risk or mixed risk populations (Gil et al. A two-phase, blinded, case-control study was performed to optimize and validate the trisomy 13 algorithm. The trisomy 13 algorithm was subsequently modified and the trisomy 13 risk score was > 99% in all 11 cases of trisomy 13 and < 0. In the second phase, the new algorithm was used to generate trisomy 13 risk scores for 10 cases of trisomy 13 and 1939 euploid cases. A single patient, who had a first-trimester screening result of one in five for trisomy 21, elected to have invasive prenatal diagnosis, which revealed a normal fetal karyotype.
Gamma-thalassemia Know the transient neonatal hemolytic disorders associated with gamma-thalassemia syndromes (e) anxiety while pregnant buy cheap pamelor 25 mg online. Beta-thalassemia/structural hgb variants Know the clinical and laboratory features of homozygous hgb E and hgb E-beta-thalassemia (3) anxiety symptoms in men generic 25mg pamelor amex. Diagnosis Know the indications for and limitations of prenatal diagnosis using chorionic villus sampling (a) anxiety 2 days after drinking buy 25mg pamelor with amex. Hereditary persistence of fetal hgb Know the characteristics which differentiate thalassemia from hereditary persistence of hgb F (4) anxiety during pregnancy purchase 25mg pamelor amex. Treatment Recognize when splenectomy is indicated in thalassemia major Know the indications for and management of chronic transfusion therapy for thalassemia syndromes Understand the principles of iron chelation therapy and when to initiate it in a patient with a thalassemia syndrome Know the beneficial effects and toxicity of ascorbic acid when given to iron-overloaded patients with thalassemia Distinguish the relative advantages and disadvantages of stem cell transplantation and conventional therapy for thalassemia major Understand the proper management of thalassemia intermedia Know the value of different laboratory and imaging studies in the assessment of iron overload Know the pharmacology of deferoxamine and how this influences drug 14 administration Know the adverse side effects of deferoxamine (hearing loss, vision changes, growth retardation) Know the pharmacology of the oral iron chelator deferasirox Know the adverse side effects of deferasirox 6. Pathophysiology Understand the effect of a major blood group incompatibility on Rh sensitization Know the erythrocyte antigens that most frequently cause erythroblastosis fetalis (2). Clinical and laboratory features Recognize the clinical features of erythroblastosis fetalis Know that transient conjugated hyperbilirubinemia may occur as a complication of severe isoimmune hemolytic disease (3). Treatment Know when to expect and how to treat the late anemia of isoimmune sensitization Know the indications for exchange transfusion Know what type of blood to use for exchange transfusions and delayed simple transfusions in sensitized infants (5). Pathophysiology Know the biologic properties and clinical significance of IgG and IgM erythrocyte antibodies Know the mechanism of erythrocyte destruction in IgG-mediated autoimmune hemolytic anemia Know the relationship between the response to corticosteroid therapy and the type of autoantibody Know the direct antiglobulin test results with warm-reactive antibodies, cold agglutinin disease, and paroxysmal cold hemoglobinuria (2). Warm-antibody hemolytic disease Know the antigen specificity (or lack thereof) in warm autoimmune hemolytic anemia Know the clinical presentation and features of idiopathic autoimmune hemolytic anemia of childhood Know of the association of warm-reactive antibodies with other autoimmune disorders Plan the therapy for autoimmune hemolytic anemia (3). Cold agglutinin disease Know the antigen specificity of cold-reactive antibodies Recognize the infections that are associated with cold-reactive antibodies Know the principles of therapy for cold agglutinin disease (4). Paroxysmal cold hemoglobinuria Identify the clinical features of autoimmune hemolytic anemia due to a Donath-Landsteiner antibody Know the characteristics of the Donath- Landsteiner antibody (5). Drug-induced immune hemolytic anemia Know the mechanism of hematologic toxicity of offending drugs Recognize the examples of drug-induced immune hemolysis 16 c. Anemia due to infection, chemical, physical agents Recognize intravascular hemolysis as a complication of recluse spider bites Know that thermal burns and envenomization may be complicated by acquired spherocytic anemia d. Erythrocyte fragmentation syndromes Recognize the pathogenic mechanisms and the clinical and laboratory features of the erythrocyte fragmentation syndromes. Paroxysmal nocturnal hemoglobinuria Recognize the laboratory and clinical manifestations of paroxysmal nocturnal hemoglobinuria Know the association of paroxysmal nocturnal hemoglobinuria with thrombosis Understand the molecular and pathophysiologic basis for paroxysmal nocturnal hemoglobinuria 7. Pathophysiology Recognize anemia due to vitamin B12 deficiency in a breast-fed infant with a vegan mother or a mother with B12 deficiency Recognize the genetically determined disorders of vitamin B12 malabsorption Know the association of small bowel bacterial overgrowth or surgery and megaloblastic anemia (2). Clinical and laboratory features Know the clinical and laboratory features of pernicious anemia Know the association of pernicious anemia with other autoimmune phenomena Know the clinical and laboratory features of the Imerslund-Graesbeck syndrome Know the ages at which different disorders of vitamin B12 metabolism are first manifested Know the morphology of peripheral blood smears and examinations of the bone marrow in megaloblastic anemia (3). Diagnosis 17 Know the indications for the Schilling test and how to interpret results of the test (4). Treatment Understand the principles of treatment for the vitamin B12 deficiency syndromes Know the potential of folic acid to correct megaloblastic anemia but not the neuropathy of pernicious anemia b. Pathophysiology Understand the biochemical pathway of tetrahydrofolate metabolism that is associated with megaloblastosis Recognize the association of folic acid deficiency with anticonvulsant therapy Know that megaloblastic anemia associated with goat milk ingestion is due to folic acid deficiency Know that folate deficiency may be associated with chronic hemolytic disorders (2). Clinical and laboratory features Understand the progression of laboratory abnormalities in folate deficiency Recognize the clinical and laboratory characteristics of dietary folate deficiency (3). Diagnosis Know the limitations of measuring serum folate concentrations in the diagnosis of folate deficiency (4). Treatment Other causes of megaloblastosis Recognize disorders other than folate or B12 deficiency causing megaloblastosis 8. Fetomaternal hemorrhage Recognize the clinical and laboratory characteristics of fetomaternal hemorrhage b. Blood loss in the infant and child Recognize the clinical signs of acute hypovolemia secondary to blood loss and differentiate them from hemolytic anemia 18 Recognize the need for iron therapy in hemolytic anemias associated with intravascular hemolysis 9. Congenital sideroblastic anemia Know the clinical and laboratory manifestations of congenital sideroblastic anemia C. Maternal-fetal and fetal-fetal transfusions Know how to document a maternal-fetal hemorrhage or twin-twin transfusion causing erythrocytosis Recognize erythrocytosis as a feature of the twin transfusion syndrome b. High oxygen affinity hemoglobins Know the relationship of high oxygen-affinity hgb with erythrocytosis c. Other causes of erythrocytosis Differentiate relative erythrocytosis from erythrocytosis due to an increase in erythrocyte mass Know the causes of primary and secondary erythrocytosis 2. Congenital cytochrome b5 reductase deficiency Know how to differentiate methemoglobinemia due to deficient methemoglobin reduction from methemoglobinemia due to increased methemoglobin production c. Hgb M disorders Recognize the clinical and laboratory findings of hgb M disease in the newborn infant 3. Normal granulocyte characteristics Know the age- and race-related normal values of granulocytes Know the life cycle of granulocytes Know the changes associated with systemic diseases, ie, cell numbers and morphology Understand and know when to order various tests of neutrophil function 2. Stage of myeloid maturation Understand progenitor cell differentiation and maturation Recognize morphologic features of myeloid precursors b. Cytokine stimulation Understand the action of cytokines on primitive myeloid progenitors and precursors and mature cells 20 3. Granules Recognize the different granulocytic granules and know their content and functions Know the diseases associated with abnormalities of granule function and morphology 4. Biochemistry Understand the various stimulators of biochemical reactions in granulocytes including degranulation, oxidative burst, phagocytosis, and killing 5. Chemotaxis, motility, and ingestion Know the factors that mediate adherence, movement, and phagocytosis in granulocyte function b. Opsonins Know the different opsonins and their role in neutrophil chemotaxis, ingestion, and killing c. Degranulation Know the different stimulators and inhibitors of granulocyte degranulation and granular fusion and the mechanism involved in degranulation and granular fusion d. Killing of ingested microorganisms Understand the mechanisms of oxygen-dependent and oxygen-independent microbial killing by phagocyte-mediated granulocytes 7. General Know the appropriate clinical and laboratory evaluation of childhood neutropenia Understand and differentiate the childhood presentations of neutropenia b. Cyclic neutropenia Know the clinical presentation, molecular biology, genetics, bone marrow findings, and therapy of cyclic neutropenia (3). Shwachman-Diamond syndrome Know the clinical presentation, molecular biology, genetics, bone marrow findings, and therapy of Shwachman-Diamond syndrome (4). Benign congenital neutropenia Know the clinical presentation, genetics, laboratory findings, and therapy of benign congenital neutropenia (5). Isoimmune and alloimmune neutropenia Know the presentation and pathophysiology of alloimmune neutropenia in newborn infants Understand the role of specific antigens in alloimmune neutropenia Know the natural history of, complications of, and therapy for alloimmune neutropenia (2). Autoimmune neutropenia Understand the use and limitations of antineutrophil antibodies in the diagnosis and treatment of autoimmune neutropenia Know the natural history of autoimmune neutropenia in infancy Understand the various therapeutic strategies for autoimmune neutropenia 22 Recognize autoimmune neutropenia as a manifestation of autoimmune disorders Know the clinical presentation of autoimmune neutropenia (3). Postinfectious and infection-related neutropenia Know the viruses commonly associated with infection-related neutropenia Know the bacteria commonly associated with postinfectious neutropenia Know the natural history of infection-related neutropenia (4). Drug-induced neutropenia Know the agents commonly involved in drug- induced neutropenia Know the mechanisms of bone marrow suppression and peripheral destruction of neutrophils Understand the therapeutic use of cytokines in drug-induced neutropenia (5). Neutropenia associated with nutritional deficiency Recognize neutropenia as a feature of copper, B12, or folate deficiency (6). Neutropenia associated with immune defects Recognize that neutropenia is a feature of immune defects (7). Neutropenia associated with metabolic diseases Recognize neutropenia as a feature of glycogen storage disease I and other metabolic disorders (8). Neutropenia associated with hypersplenism Recognize that hypersplenism can present with neutropenia 8. Neutrophilia Know the effect of glucocorticoids on the absolute neutrophil count Know the major causes of acute and chronic neutrophilia Know the significance of neutrophilia in newborn infants 23 9. Eosinophilia Know the disorders associated with primary and secondary eosinophilia Know the correlation of eosinophilia with specific parasitic infestations Know the clinical consequences of hypereosinophilia 10. General Differentiate the granulocyte functional abnormalities associated with altered killing of microorganisms Know the clinical features associated with various neutrophil function disorders b. Chronic granulomatous disease Know the current approaches to the diagnosis and treatment of chronic granulomatous disease 24 Know the organisms that are poorly killed by the granulocytes of patients with chronic granulomatous disease Know the clinical manifestations, molecular biology, and inheritance patterns of chronic granulomatous disease. Hyperimmunoglobulinemia E syndrome Know the clinical manifestations of hyperimmunoglobulin E syndrome Understand the laboratory evaluation and differential diagnosis of hyperimmunoglobulin E syndrome f. Myeloperoxidase deficiency Know the genetics, clinical presentation, and laboratory evaluation of neutrophil myeloperoxidase deficiency g.
Although meconium is sterile anxiety 2 calm buy 25 mg pamelor free shipping, it inhibits the normally bacteriostatic quality of amniotic fluid anxiety symptoms concentration purchase pamelor 25mg fast delivery. However anxiety symptoms duration buy pamelor 25 mg cheap, because it is difficult to differentiate meconium aspiration from pneumonia radiographically anxiety symptoms jaw spasms pamelor 25 mg lowest price, infants with infiltrates on a chest radiograph should be started on broad-spectrum antibiotics (ampicillin and gentamicin; for dosages, see Chapter 148) after appropriate cultures have been obtained. Some clinicians may elect to maintain Pao2 at a higher level because the risk of retinopathy should be negligible among full-term infants. The same goal of preventing alveolar hypoxia requires cautious weaning from oxygen therapy. Many of the patients are very labile, and weaning from oxygen should be made slowly, sometimes at a pace of 1% at a time. The prevention of alveolar hypoxia includes a high index of suspicion for the diagnosis of air leak as well as efforts to minimize handling of the child. Patients with severe disease who are in impending respiratory failure with hypercapnia and persistent hypoxemia require mechanical ventilation. The use of relatively short inspiratory time may further limit potential air trapping. Modes of ventilation that allow the infant to regulate the frequency and degree of mechanical assistance (assist/control or pressure support ventilation) may be preferable. With the development of atelectasis, air trapping, and decreased lung compliance, high mean airway pressures may be required in a patient who is at risk for air leak. For any unexplained deterioration of clinical status, the possibility of a pneumothorax or pneumomediastinum should be considered and appropriate evaluation undertaken. The approach to ventilation must be directed at preventing hypoxemia and providing adequate ventilation at the lowest mean airway pressure possible to reduce the risk of catastrophic air leak. Both high-frequency jet ventilation and high-frequency oscillatory ventilation are efficacious in infants in whom adequate ventilation cannot 108: MeconiuM AspirAtion 753 be maintained on conventional ventilation without using excessive ventilatory pressures. In a limited study, the use of heliox was associated with improved oxygenation but failed to demonstrate significant improvement in other outcomes, including oxygenation index, survival, or degree of respiratory support, beyond the reduction in Fio2. Doses may exceed those used for preterm infants with respiratory distress syndrome. Because of the potential for concomitant pulmonary hypertension, close observation is required to prevent the consequences of transient airway obstruction that may develop during the tracheal instillation of surfactant. Current clinical trials have failed to demonstrate a statistically significant impact on other outcome measures but did demonstrate a trend toward improved survival. Although some animal data and limited human trials suggest a potential benefit, there are not sufficient data to warrant the use of steroids. In patients surviving severe meconium aspiration, bronchopulmonary dysplasia/chronic lung disease may result from prolonged mechanical ventilation. Neurodevelopmental outcome of infants with meconium aspiration syndrome: report of a study and literature review. Randomized controlled trial of lung lavage with dilute surfactant for meconium aspiration syndrome. Role of distinct phospholipases A2 and their modulators in meconium aspiration syndrome in human neonates. High frequency oscillatory ventilation versus conventional ventilation for infants with severe pulmonary dysfunction born at or near term. Neonatal meningitis is often accompanied by ventriculitis, which makes resolution of infection more difficult. There is also a predilection for vasculitis, which may lead to hemorrhage, thrombosis, and infarction. In the very low birthweight infant, coagulase-negative staphylococci need to be considered as causative organisms in bacterial meningitis. Many unusual organisms, including Ureaplasma, fungi, and anaerobes, have been described in case reports of neonatal meningitis. The clinical presentation is usually nonspecific and indistinguishable from those caused by sepsis. Meningitis must be excluded in any infant being evaluated for sepsis or infection. Signs and symptoms of meningitis include temperature instability (the most common), lethargy, irritability, poor tone, seizures, feeding intolerance, vomiting, respiratory distress, apnea, or cyanotic episodes. Seizures, often focal, can be the presenting manifestation in up to 50% of the cases. Gram-stained smear can be helpful in making a more rapid definitive diagnosis and identifying the initial classification of the causative agent. Imaging studies are recommended to detect the complications of meningitis, especially when the clinical course is complicated. Infection with certain microorganisms such as Citrobacter koseri and Enterobacter sakazakii predispose for the development of brain abscesses. The most useful and noninvasive method of imaging is ultrasonography, which provides information regarding ventricular size, inflammation (echogenic strands), and the presence of hemorrhage. General supportive measures like ventilation/oxygenation, cardiovascular support, intravenous dextrose, and anticonvulsant therapy are considered essential components of managing the neonate with bacterial meningitis. Optimal antibiotic selection depends on culture and sensitivity testing of the causative organisms. Ampicillin and gentamicin are usually started as empirical therapy for suspected early sepsis. Lastly, for the infant <60 days who is coming from home to the emergency department, the empiric therapy consists of ampicillin and cefotaxime. Because of the increased prevalence of methicillinresistant staphylococci both in the nosocomial setting and in the community, vancomycin should be substituted for penicillin or ampicillin as initial coverage. Most clinicians would use ampicillin plus cefotaxime plus an aminoglycoside as initial therapy. There is an emerging problem with multidrug-resistant enteric microorganisms (especially Klebsiella pneumoniae); for this situation, the drug of choice is meropenem. Persistence of infection may indicate a focus, such as obstructive ventriculitis, subdural empyema, or multiple smallvessel thrombi. External ventricular drainage may be indicated in certain cases complicated by ventriculitis. Treatment should continue until 14 days after cultures are negative or for 21 days, whichever is longer. Contrary to childhood meningitis, dexamethasone does not seem to improve the outcome of neonatal meningitis. Other therapies focusing on enhancing the immune system in the newborn, such as hematopoietic growth factors or intravenous immune globulins, do not seem to help either. Head circumference should be measured daily, and neurologic examination should be performed frequently. Hearing and vision evaluation should be done in all neonates who develop meningitis. Group B streptococcal meningitis: cerebrospinal fluid parameters in the era of intrapartum antibiotic prophylaxis. Repeat lumbar punctures in infants with meningitis in the neonatal intensive care unit. Traumatic lumbar punctures in neonates: test performance of the cerebrospinal fluid white blood cell count. Should a neonate with possible late onset infection always have a lumbar puncture The source of the bacteria could be a health care worker, another patient, equipment, or a family member.
Generic 25 mg pamelor overnight delivery. Anxiety Disorder - Panic Attacks - Free Hypnosis CD.
References