




|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Robert T. Eberhardt, MD
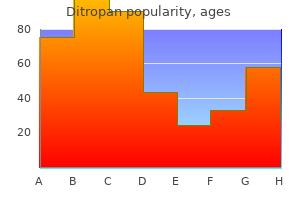
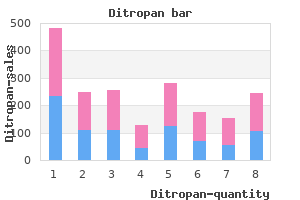
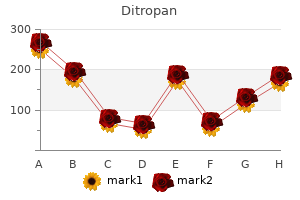
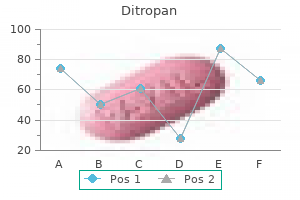
During cardiac catheterization gastritis working out purchase 5 mg ditropan amex, the measurements of both the pressures and the cardiac output can be made simultaneously; with this information gastritis kombucha order 5mg ditropan free shipping, the size of the stenotic orifice can be calculated according to the previously shown equation gastritis diet x program generic ditropan 2.5mg otc. Aortography or left ventriculography is routinely performed to show the details of the aortic valve and the surrounding vascular and cardiac structures gastritis diet ютьюб discount ditropan 5 mg with visa. A fluid-filled catheter-mounted balloon with inflated diameter similar to the measured aortic valve annulus diameter is positioned across the aortic valve and rapidly inflated and deflated. Balloon dilation may result in valvar regurgitation Provided that predilation aortic regurgitation was not severe, any increase is usually well tolerated. Operative considerations Relief of the aortic stenosis gradient, by either balloon dilation or cardiac surgery, is indicated for patients with significant symptoms or for those whose catheterization data or echocardiogram indicate moderate or severe stenosis. In children, the stenotic valve is usually pliable enough for valvotomy or valvuloplasty so that an aortic valve replacement with a prosthesis or homograft (cadaveric human valve) is not required. Ultimately, children who have undergone aortic valvotomy may require a prosthesis or homograft in adulthood if the valve becomes calcified or rigid, or sooner, if the valve develops important regurgitation. No currently available replacement valve is perfect: mechanical prostheses are long lived but thrombogenic, so anticoagulation is required; homograft valves, although free from thrombogenic complications, are often shorter lived because of destruction by calcification at an unpredictable rate. A homograft valve is placed in the pulmonary position, where performing balloon dilation or future surgical revision is less risky because of its more accessible anterior location and presence on the pulmonary side of the circulation. Summary In aortic valvar stenosis, a suprasternal notch thrill is present, associated with a systolic ejection murmur in the aortic area and with an aortic systolic ejection click. The electrocardiogram may show left ventricular hypertrophy and repolarization abnormalities. The echocardiogram is the most crucial laboratory examination for following the course of the patient. The echocardiographic estimate of the degree of obstruction or symptoms, such as chest pain or syncope, alerts the provider that further diagnostic studies and intervention are warranted. Relief of the obstruction by valvotomy or valvuloplasty can be done at low risk in children with moderate or severe stenosis. Discrete membranous subaortic stenosis this is the second most common form of left ventricular outflow obstruction but much less frequent than aortic valvar stenosis. This obstruction is a fibromuscular membrane with a small central orifice located in the left ventricle, usually within 1 cm of the aortic valve (Figure 5. Because the jet strikes the aortic valve, the energy 5 Conditions obstructing blood flow in children 169 of the jet is dissipated so that poststenotic dilation of the ascending aorta rarely occurs; however, problems with aortic valve regurgitation frequently result from alterations in the aortic valve. The symptoms of chest pain and syncope may occur in patients with severe obstruction, but most patients are asymptomatic. Physical examination the prominent physical finding is an aortic systolic ejection murmur heard best along the left sternal border, often lower than in patients with valvar aortic stenosis. Systolic ejection clicks rarely occur because the ascending aorta is usually normal in size. An aortic early diastolic murmur of aortic regurgitation is present in about 70% of the patients. Natural history Discrete membranous subaortic stenosis progresses, not usually because of increasing subaortic stenosis but because of aortic valvar regurgitation. The aortic regurgitation develops and progresses from trauma of the jet on the aortic valve. Echocardiogram A discrete subaortic ridge can usually be seen projecting from the septum into the left ventricular outflow tract. In contrast to valvar aortic stenosis, the disturbed color Doppler signals indicating turbulent flow begin at the site of the membrane, proximal to the valve itself. The maximum velocity of flow through the outflow tract is used to estimate the gradient. Some patients with a relatively unimportant gradient, less than 40 mmHg, have important aortic valvar regurgitation. A systolic pressure gradient is found below the level of the aortic valve within the left ventricle (Figure 5. Aortic regurgitation, if severe, causes a wide aortic pulse pressure and an elevated left ventricular end-diastolic pressure. Left ventriculography may identify the location of the membrane but is less helpful than echocardiography. Operative considerations Excision of the membrane is indicated in most patients, unless the gradient is small. Balloon dilation of subaortic membrane has been unsuccessful in reducing the gradient. The purposes of operation are relief of the elevated left ventricular systolic pressure and reduction of the aortic valve trauma. The operative risk, which is minimal, approaches that of operation for valvar aortic stenosis. The major hazard of the operation is damage to the septal leaflet of the mitral valve, since the membrane is often attached to this leaflet. The results are generally very good, with near-normal left ventricular systolic pressure postoperatively. The degree of aortic valve regurgitation is lessened and progression is generally halted. Summary Discrete membranous subaortic stenosis clinically resembles valvar aortic stenosis in many respects, but it lacks the clinical and roentgenographic findings of poststenotic dilation of the aorta. Supravalvar aortic stenosis Obstruction to left ventricular outflow can also result from supravalvar stenosis. In most patients, the ascending aorta narrows in an hourglass deformity (Figure 5. Although usually limited to the ascending aorta, other arteries, such as the brachiocephalic and the renal arteries, may also be narrowed. Peripheral pulmonary arterial stenosis and hypoplasia may coexist and represent the most important cardiovascular problem. The elevation can lead to tortuosity of the coronary arteries and to premature atherosclerosis. The coronary artery ostia may be narrowed by the same obstructive process operating in the aorta and other large vessels and has a poor prognosis. The second is familial supravalvar aortic stenosis, which occurs in patients who do not have Williams syndrome; they probably carry a mutated elastin gene (see Chapter 2). History Most patients are asymptomatic; cardiac disease is identified by either the presence of a murmur or the facial characteristics of Williams syndrome. Congestive cardiac failure or growth retardation is rare, as in other forms of aortic stenosis, but sudden death can occur. The risk might even be higher because of acquired abnormalities of the coronary arteries. Physical examination the general physical characteristics of the child, particularly the facies, suggest the diagnosis of supravalvar aortic stenosis (see Chapter 2). Careful blood pressure recording in both arms and legs can lead to suspicion of supravalvar aortic stenosis if a blood pressure discrepancy of 20 mmHg or more is found between the arms (Coanda effect). This effect is related to either a narrowing of a subclavian artery or the pressure effect of the jet from the supravalvar aortic stenosis directed into the right subclavian artery. An aortic systolic ejection murmur is the prominent cardiac finding and, in contrast to valvar stenosis, is located maximally beneath the right clavicle, not along the left sternal border. A systolic ejection click is not present because poststenotic dilation does not occur. Electrocardiogram the electrocardiogram usually shows features similar to those of valvar aortic stenosis, including left ventricular hypertrophy. Some patients, for unknown reasons, show an rSr pattern in lead V1 and an Rs in lead V6, without criteria of left ventricular hypertrophy. The major change over the course of this disease is the development of myocardial ischemia and fibrosis and its consequences, although findings of right heart hypertension predominate in peripheral pulmonary artery stenosis. Echocardiogram Cross-sectional views of the ascending aorta parallel to its long axis show discrete and often severe narrowing at the sinotubular junction and, at times, more diffuse narrowing into the distal ascending aorta. Unlike valvar aortic stenosis, flow acceleration and turbulence begin at the supravalvar narrowing.
Unless hypoxia is treated xifaxan gastritis generic 2.5mg ditropan free shipping, it becomes severe gastritis tratamiento cheap 5mg ditropan with visa, leading to metabolic acidosis and death gastritis duration of symptoms generic 5mg ditropan fast delivery. This substance opens and/or maintains patency of the ductus arteriosus and improves blood flow from aorta to pulmonary artery gastritis diet 3 day ditropan 2.5mg on line. Patients with inadequate mixing benefit from the creation of an atrial septal defect (enlargement of the foramen ovale). At cardiac catheterization or by echocardiographic guidance, a balloon catheter is inserted through a systemic vein and advanced into the left atrium through the foramen ovale. The balloon is inflated and then rapidly and forcefully withdrawn across the septum, creating a larger defect and often improving the hypoxia. Infants who do not experience adequate improvement of cyanosis despite a large atrial defect and patent ductus are rare. Factors responsible in these neonates include nearly identical ventricular compliances, which limits mixing through the atrial defect, and elevated pulmonary vascular resistance, which limits the ductal shunt and pulmonary blood flow. Rarely, an atrial defect is created surgically by atrial septectomy, an open-heart procedure. The first successful corrective procedure was performed by Senning in the 1950s and later modified by Mustard. Since the circulation of transposition is reversed at the arterial level, these operations reverse it the atrial level. This procedure involves removal of the atrial septum and creation of an intra-atrial baffle to divert the systemic venous return into the left ventricle and thus to the lungs, whereas the pulmonary venous return is directed to the right ventricle and thus to the aorta. It can be performed at low risk in patients with an intact ventricular septum and at a higher risk in patients with ventricular septal defect. Arrhythmias, the most frequent long-term complication, are often related to abnormalities of the sinoatrial node and of the atrial surgical scar. Sometimes these are life threatening, although the exact mechanism of sudden death in the rare child who succumbs is not usually known. The most common significant complication is not sudden death but progressive dysfunction of the right ventricle, leading to death from chronic heart failure in adulthood. This complication is related to the right ventricle functioning as the systemic ventricle. Predicting which patients will develop failure and at the age postoperatively is not possible. This operation, developed in the 1970s, avoids the complications inherent with the atrial (venous) switch and involves switching the aorta and pulmonary artery to the correct ventricle. The great vessels are transected and reanastomosed, so blood flows from left ventricle to aorta and from right ventricle to pulmonary arteries. Since the coronary arteries arise from the aortic root, they are transferred to the pulmonary (neoaortic) root. Certain variations of coronary artery origins or branching make transfer more risky. The arterial switch operation must occur early in life (within the first 2 weeks) before the pulmonary resistance falls and the left ventricle becomes "deconditioned" to eject the systemic pressure load. Arterial switch is not free from complications: coronary artery compromise may result in left ventricular infarct or failure; pulmonary artery stenosis can result from stretching or kinking during the surgical repositioning of the great vessels; and the operative mortality may be higher, partly because of the risks of neonatal openheart surgery. The short- and long-term outcomes favor those receiving the arterial switch procedure. Summary Complete transposition of the great arteries is a common cardiac anomaly that results in neonatal cyanosis and ultimately in cardiac failure. Developmentally, this anomaly results from failure of incorporation of the pulmonary veins into the left atrium, so that the pulmonary venous system retains earlier embryologic communications to the systemic venous system. In the embryo, the pulmonary veins communicate with both the left and right anterior cardinal veins and the umbilical vitelline system, both precursors of systemic veins. Therefore, the right atrium receives not only the entire systemic venous return, but also the entire pulmonary venous return. An obligatory right-to-left shunt exists at the atrial level through either a patent foramen ovale or usually an atrial septal defect. The volume of blood shunted from the right to the left atrium and the volume of blood that enters each ventricle depends upon their relative compliances. Ventricular compliance is influenced by ventricular pressures and vascular resistances. Right ventricular compliance normally increases following birth as pulmonary vascular resistance and pulmonary arterial pressure fall. Therefore, in most patients with total anomalous pulmonary venous connection, pulmonary blood flow becomes considerably greater than normal; systemic blood flow is usually normal. Since a disparity exists between the volume of blood being carried by the right and left sides of the heart, the right side becomes dilated and hypertrophied, whereas the left side is relatively smaller but near-normal size. In patients with total anomalous pulmonary venous connection, the degree of cyanosis inversely relates to the volume of pulmonary blood flow. As the volume of pulmonary blood flow becomes larger, the proportion of the pulmonary venous blood to total venous blood returning to the right atrium becomes greater. As a result, the saturation of blood shunted to the left side of the heart is higher, being only slightly reduced from normal. On the other hand, in hemodynamic situations in which the resistance to flow through the lungs is increased. Therefore, the pulmonary and systemic venous systems contribute nearly equal volumes of blood to the right atrium, and these neonates exhibit noticeable cyanosis. The other shows intense cyanosis and a radiographic pattern of pulmonary venous obstruction. Usually, the anomaly is recognized in the neonatal period or with fetal echocardiography. If not operated upon in early infancy, most patients develop congestive cardiac failure, grow slowly, and have frequent respiratory infections, but a few may be asymptomatic into later childhood. The degree of cyanosis varies because of differences in the volume of pulmonary blood flow. Although systemic arterial desaturation is always present, children with greatly increased pulmonary blood flow appear acyanotic or show only slight cyanosis. Cardiomegaly, precordial bulge, and right ventricular heave are found in older unoperated infants. Wide, fixed splitting of the second heart sound is heard and the pulmonary component may be accentuated, reflecting elevated pulmonary pressure. A mid-diastolic murmur caused by increased blood flow across the tricuspid valve is found along the lower left sternal border and is associated with greatly increased pulmonary blood flow. In total anomalous pulmonary venous connection to the superior vena cava, a venous hum may exist along the upper right sternal border because of the large venous blood flow. The electrocardiogram reveals enlargement of the rightsided cardiac chambers with right-axis deviation, right atrial enlargement, and right ventricular enlargement/hypertrophy. Cardiomegaly, primarily of right-sided chambers, and increased pulmonary blood flow 6 Congenital heart disease with a right-to-left shunt in children 199 are found. In contrast to most other admixture lesions, the left atrium is not enlarged because blood flow through this chamber is normal. Except for total anomalous pulmonary venous connection to a left superior vena cava ("vertical vein"), the roentgenographic contour is not characteristic. In this form, the cardiac silhouette can be described as a figure-of-eight or as a "snowman heart" (Figure 6. The upper portion of the cardiac contour is formed by the enlarged left and right superior venae cavae. Summary of clinical findings the clinical, electrocardiographic, and roentgenographic findings resemble those of atrial septal defect because the effects on the heart are similar. Cyanosis distinguishes the conditions; although it may be minimal or not clinically evident, it is easily detectable by pulse oximetry.
His mean arterial pressure has fallen gastritis diet гороскоп generic ditropan 2.5 mg with mastercard, and several fluid boluses were administered gastritis gerd ditropan 2.5mg visa. Several days following esophagectomy gastritis symptoms at night cheap 5mg ditropan amex, a patient complains of dyspnea and chest tightness gastritis medscape safe ditropan 2.5 mg. A large pleural effusion is noted on chest radiograph, and thoracentesis yields milky fluid consistent with chyle. A 56-year-old woman presents for evaluation of a murmur suggestive of mitral stenosis and is noted on echocardiography to have a lesion attached to the fossa ovalis of the left atrial septum. A 56-year-old woman has been treated for 3 years for wheezing on exertion, which was diagnosed as asthma. A 59-year-old man is found to have a 6-cm thoracoabdominal aortic aneurysm which extends to above the renal arteries for which he desires repair, but he is concerned about the risk of paralysis postoperatively. Which of the following maneuvers should be employed to decrease the risk of paraplegia after repair Infusion of a bolus of steroids immediately postoperatively with a continuous infusion for 24 hours b. A 70-year-old woman undergoes a cardiac catheterization for exertional chest pain. Two-vessel coronary disease with proximal left anterior descending artery stenosis and depressed left ventricular ejection fraction b. Isolated left main stenosis, no diabetes, and normal left ventricular ejection fraction c. Left main stenosis and additional coronary artery disease with depressed left ventricular ejection fraction. A 27-year-old woman seeks your advice regarding pain and numbness in the right arm and hand. On examination, the right radial pulse disappears when the patient takes a deep breath and turns her head to the left. Which of the following is the most appropriate initial treatment for this patient He has no evidence of recurrence or extrathoracic disease and is in good general health. A 65-year-old woman has had pain in her right shoulder and has been treated with analgesics without relief. Superior pulmonary sulcus carcinomas (Pancoast tumors) are bronchogenic carcinomas that typically produce which of the following clinical features A 63-year-old man has a chylothorax that after 2 weeks of conservative therapy appears to be persistent. Imaging suggests ipsilateral mediastinal lymph node involvement but no extrathoracic disease. Right lower lobectomy and mediastinal lymph node dissection followed by adjuvant chemotherapy c. Neoadjuvant chemotherapy followed by right lower lobectomy and mediastinal lymph node dissection d. Neoadjuvant chemoradiation followed by right lower lobectomy and mediastinal lymph node dissection. Six months ago at the time of lumpectomy for breast cancer, a 60-year-old female attorney quit a 30-year smoking habit of 2 packs per day. She had the chest radiograph shown here as part of her routine follow-up examination. Based on her age and history of smoking, you are concerned for either a new primary lung or metastatic breast malignancy. Which of the following is the most appropriate next step in the management of this lesion Magnetic resonance imaging of bilateral breasts to evaluate for recurrence of the breast cancer c. At the time of operation on this patient, a firm, rubbery lesion in the periphery of the lung is discovered. It is sectioned in the operating room to reveal tissue that looks like cartilage and smooth muscle. A 45-year-old woman presents with dysphagia, regurgitation of undigested food, and weight loss. Upper endoscopy reveals no evidence of malignancy and esophageal motility studies show incomplete lower esophageal sphincter relaxation. Transhiatal esophagectomy Questions 398 to 402 For each physical finding or group of findings, select the cardiovascular disorder with which it is most likely to be associated. A patient with flushing and paling of the nail beds (Quincke pulse) and a bounding radial pulse. Questions 403 to 407 For each clinical scenario, select the mediastinal tumor with which it is most likely to be associated. A 23-year-old patient with hypertension and increased urinary catecholamine levels. A 63-year-old woman with vague symptoms of fatigue and depression presents with hematuria. Questions 408 to 412 For each clinical scenario, select the most appropriate pharmacologic agent for the patient. A 65-year-old man presents with cardiogenic shock following a myocardial infarction. A 30-year-old man presents with perforated appendicitis and heart rate of 120 beats per minute, blood pressure of 80/40 mm Hg, and central venous pressure of 17 mm Hg. A 21-year-old man undergoes major abdominal surgery after a motor vehicle collision. He has a cardiac arrest in the intensive care unit shortly after returning from surgery. A 45-year-old woman presents with a blood pressure of 220/130 mm Hg and a headache. After several hours of an intravenous drip of medication to control her hypertension, she becomes acidotic. The only effective therapy with good longterm results is aortic valve replacement, with most patients achieving symptom relief after surgery. Percutaneous aortic balloon valvuloplasty is an option for patients who are not candidates for aortic valve replacement or whose long-term survival is poor. Valvuloplasty involves passing balloon catheters through the aortic orifice and inflating them in an effort to break the calcium that is retarding leaflet motion. The results are not as durable as those for valve replacement, with a third of the patients having recurrent symptoms by 6 months. Aortic stenosis is most often thought to result from calcification of the aortic valve associated with advanced age. The process is mostly idiopathic, with only a small percentage associated with rheumatic fever. The combination of aortic stenosis and congestive heart failure, which is the presenting symptom in nearly one-third of patients, has a worse prognosis. Medical management, percutaneous coronary artery angioplasty and stenting, and coronary artery bypass surgery are options for angina due to coronary artery disease. Carbon monoxide diffusing capacity measures the rate at which carbon monoxide moves from the alveolar space to combine with hemoglobin in the red blood cells. It is determined by calculating the difference between inspired and expired samples of gas. Most are centrally located and characterized by an aggressive tendency to metastasize. They spread early to mediastinal lymph nodes and distant sites, most commonly to the bone marrow and the brain. Based on the history (3 weeks of symptoms) and the fluid analysis demonstrating a glucose level less than 40 mg/dL and a pH less than 7. In this phase, the fluid collection is loculated and depositions of fibrin create a thick pleural rind, which prevents apposition of the lung to the parietal pleura.
A 10-year-old boy was the backseat belted passenger in a high-speed motor vehicle collision gastritis diet 6 small discount 5mg ditropan overnight delivery. He is complaining of abdominal pain and has an ecchymosis on his anterior abdominal wall where the seatbelt was located gastritis diet natural treatment buy ditropan 2.5mg overnight delivery. Discharge him home if his abdominal plain films are negative for the presence of free air gastritis and celiac diet buy ditropan 5 mg on-line. A 65-year-old man who smokes cigarettes and has chronic obstructive pulmonary disease falls and fractures the third gastritis diet русская ditropan 2.5mg fast delivery, fourth, and fifth ribs in the left anterolateral chest. On examination, he has tenderness and bruising over his left lateral chest below the nipple. The patient has a fractured femur, a pelvic fracture, a tender abdomen, and no pulses in the right foot with minimal tissue damage to the right leg. On examination, there are weak pulses palpable distal to the injury and the patient is unable to move his foot. A 17-year-old adolescent boy is stabbed in the left seventh intercostal space, midaxillary line. Your hospital is conducting an ongoing research study involving the hormonal response to trauma. Which of the following values are likely to be seen after a healthy 36-year-old man is hit by a bus and sustains a ruptured spleen and a lacerated small bowel He is taken to the operating room and, after management of a liver injury, is found to have a complete transection of the common bile duct with significant tissue loss. You evaluate an 18-year-old man who sustained a right-sided cervical laceration during a gang fight. Which of the following is a relative, rather than an absolute, indication for neck exploration Following blunt abdominal trauma, a 12-year-old girl develops upper abdominal pain, nausea, and vomiting. An upper gastrointestinal series reveals a total obstruction of the duodenum with a coiled spring appearance in the second and third portions. In the absence of other suspected injuries, which of the following is the most appropriate management of this patient He has a seatbelt sign across his neck and chest with an ecchymosis over his left neck. In the absence of other significant injuries, what is the next step in his management An 18-year-old man was assaulted and sustained significant head and facial trauma. Which of the following is the most common initial manifestation of increased intracranial pressure On examination, he is noted to have an obvious skull fracture and his right pupil is dilated. Which of the following is the most appropriate method for initially reducing his intracranial pressure A 45-year-old man was an unhelmeted motorcyclist involved in a high-speed collision. Examination reveals stable vital signs and no evidence of respiratory distress, but the patient exhibits multiple palpable rib fractures and paradoxical movement of the right side of the chest. There is no evidence of vascular injury, but he cannot flex his three radial digits. Following a 2-hour firefighting episode, a 36-year-old fireman begins complaining of a throbbing headache, nausea, dizziness, and visual disturbances. A 75-year-old man with a history of coronary artery disease, hypertension, and diabetes mellitus undergoes a right hemicolectomy for colon cancer. On the second postoperative day, he complains of shortness of breath and chest pain. He becomes hypotensive with depressed mental status and is immediately transferred to the intensive care unit. After intubation and placement on mechanical ventilation, an echocardiogram confirms cardiogenic shock. A central venous catheter is placed that demonstrates a central venous pressure of 18 mm Hg. An electrical spark jumps from the wire to his metal belt buckle and burns his abdominal wall, knocking him to the ground. Intravenous fluid replacement is based on the percentage of body surface area burned. Evaluation for fracture of the other extremities and visceral injury is indicated. The entrance wound is 3 cm inferior to the nipple and the exit wound is just below the scapula. A chest tube is placed that drains 400 mL of blood and continues to drain 50 to 75 mL/h during the initial resuscitation. Initial blood pressure of 70/0 mm Hg has responded to 2-L crystalloid and is now 100/70 mm Hg. His heart rate is 120 beats per minute, blood pressure is 80/40 mm Hg, and respiratory rate is 35 breaths per minute. Which of the following is the most appropriate next step in the workup of his hypotension Neurosurgical consultation for emergent ventriculostomy to manage his intracranial pressure b. Neurosurgical consultation for emergent craniotomy for suspected subdural hematoma c. Administration of mannitol and hyperventilation to treat his elevated intracranial pressure. A 25-year-old man is involved in a gang shoot-out and sustains an abdominal gunshot wound from a. At laparotomy, it is discovered that the left transverse colon has incurred a throughand-through injury with minimal fecal soilage of the peritoneum. Primary repair should be performed, but only in the absence of hemodynamic instability. Primary repair should be performed with placement of an intra-abdominal drain next to the repair. Primary repair should be performed and intravenous antibiotics administered for 14 days. The patient should undergo a 2-stage procedure with resection of the injured portion and reanastomosis 48 hours later when clinically stabilized. A 34-year-old prostitute with a history of long-term intravenous drug use is admitted with a 48hour history of pain in her left arm. Physical examination is remarkable for crepitus surrounding needle track marks in the antecubital space with a serous exudate. A 47-year-old man is extricated from an automobile after a motor vehicle accident. Which of the following is the best next test for evaluation for a blunt cardiac injury Measurement of serial creatinine phosphokinase and creatinine kinase (including the myocardial band) levels b. Decreased glutamine consumption by fibroblasts, lymphocytes, and intestinal epithelial cells 160. There is no exit wound, and an x-ray of the abdomen shows the bullet to be located in the right lower quadrant. Which of the following is most appropriate in the management of his suspected rectal injury On physical examination, he is hypotensive with distended neck veins and absence of breath sounds in the left chest. A 48-year-old man sustains a gunshot wound to the right upper thigh just distal to the inguinal crease. Peripheral pulses are palpable in the foot, but the foot is pale, cool, and hypesthetic. The patient should be taken to the operating room immediately to evaluate for a significant arterial injury. A neurosurgical consult should be obtained and somatosensory evoked potential monitoring performed. The patient should be observed for at least 6 hours and then reexamined for changes in the physical examination.
Purchase ditropan 5mg free shipping. Discover the secret of method eliminate gastritis and heartburn - YeGaDi.