




|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Philip R. Gehrman, PhD, CBSM
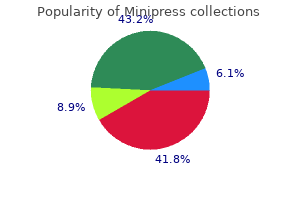
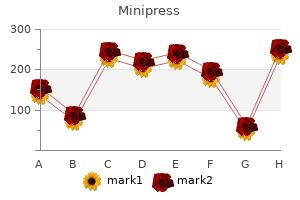
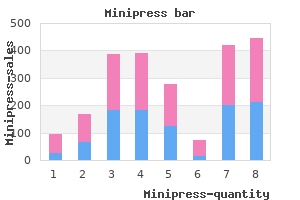
Anaphylactic-like reactions to contrast media are not considered to be dose related antiviral zovirax generic minipress 2.5bottles free shipping. Other Adverse Contrast Reactions Neurotoxicity: Neurotoxicity can be caused by direct contact of a contrast medium with the central nervous system (intrathecal or intracisternal); may occur from "indirect" contact via intravascular injection hiv infection woman to man generic 2 mg minipress amex. Summary Mild reactions to iodinated contrast media are relatively common but severe reactions are rare hiv infection rates uk 2013 generic 2 mg minipress overnight delivery. The exact etiology Adverse Reactions hiv infection female to male discount 2.5mg minipress fast delivery, Iodinated Contrast Media, Delayed 47 and mechanism of these allergic-like reactions are not fully defined though they appear to be caused by the contrast molecule, rather than the iodide itself, through a complex series of events that affects IgE plus activation of other mediators such as the leucotrienes and bradykinin. Reactions to contrast media appear relatively unique to the individual patient and are not consistently predictable. Recognizing the signs and presentations allows the radiologist and clinician to identify the type of reaction which, in turn, facilitates rapid treatment and reversal of the reaction. The over-riding decision about the use of iodinated contrast in the pregnant patient usually relates to the radiation necessary to generate the image and risk of radiation to the fetus. Iodinated contrast and lactation become of concern only because the nursing infant is an "innocent bystander"-the mother, not the infant, needs the contrast medium for the imaging study. An option to avoid any contrast exposure to the infant is for the lactating mother to use a breast pump for days prior to the contrast study to obtain and store (freeze) breast milk; then she pumps and discards the breast milk for 2 days after her contrast study. However, for lactating/nursing mothers after pregnancy, the same principles for contrast use as with iodinated contrast can be applied since less than 0. Reaction Type and Severity the symptoms of delayed reactions most commonly described are headache, skin rash, itching, nausea, dizziness, urticaria, fever, arm pain, and gastrointestinal disturbances. The types of delayed skin reactions and their relative frequencies are similar to those, which occur with many other drugs. Other frequently occurring skin reactions are angioedema, urticaria, erythema, macular exanthema, and scaling skin eruption. In most cases the skin reactions are mild or moderate, that is they may be discomforting and require specific treatment (steroids, antihistamines, topical emollients). Depending on their localization, these reactions may be more or less disturbing, the most troublesome being those confined to the palms, soles of the feet, or face. Severe delayed reactions needing hospital treatment and/or leading to persistent disability or death have been reported, but are very rare. Furthermore, often patients who experienced delayed reactions had underlying serious medical conditions. A number of pathophysiological mechanisms have been proposed for delayed skin reactions. The skin reactions often show typical features of delayed hypersensitivity including exanthematous rash, positive skin tests, and lymphocyte rich dermal perivascular infiltrate sometimes accompanied by eosinophils on skin biopsy. If there is doubt about whether contrast medium is responsible for the skin reaction, skin testing (patch and delayed intradermal tests) may be attempted (1). However, the low negative predictive value of such tests should be reminded and it remains to be established if skin testing is also a suitable tool for selection of an alternative contrast medium. A further problem is the fact that the greater the time interval between the contrast medium injection and the onset of symptoms, the more difficult it is to be sure that the symptoms are contrast mediuminduced. This has been highlighted by studies of "background noise" by several investigators who have shown a high incidence of delayed symptoms after radiological investigations not using contrast medium. The frequency of delayed adverse reactions to nonionic monomers has been reported to be between 0. There do not appear to be significant differences in the incidence of delayed reactions between ionic and nonionic agents, nor between the different nonionic monomers. No significant differences have been found between the nonionic monomers and the ionic dimer ioxaglate either. The available evidence suggests that delayed skin reactions are more common with nonionic dimers. The nonionic dimer iodixanol caused more delayed skin reactions than either the ionic dimer ioxaglate or the nonionic monomers iopamidol and iomeprol (4). In another study, the frequency of delayed skin reactions with iodixanol was similar to that with nonionic monomer, but more of the iodixanol patients were treated with hydrocortisone or antihistamine (3). Most reactions are self-limiting and have resolved by 7 days, with up to three-quarters resolving within 3 days. Predisposing Factors A number of factors appear to predispose to the development of delayed adverse reactions. A previous reaction to contrast medium is an important predisposing factor increasing the risk by a factor of 1. However, there is no evidence that patients with a Frequency Determining the true frequency of delayed adverse reactions to contrast media from the literature is difficult. Adverse Reactions, Iodinated Contrast Media, Delayed 49 Adverse Reactions, Iodinated Contrast Media, Delayed. A history of allergy is a further risk factor, increasing the likelihood of a reaction approximately twice. Especially, a history of drug and contact allergy seems to predispose to delayed skin reactions after contrast medium exposure. A seasonal variation in the incidence of delayed skin reactions has been described: a significantly higher incidence of delayed adverse reactions during the pollinosis period was observed. Coexisting diseases also appear to predispose to delayed reactions, especially renal disease, but also cardiac and liver disease and diabetes mellitus. Some of the most severe skin reactions reported occurred in patients with systemic lupus erythematosus or patients who were taking hydralazine, which induces a lupus-like syndrome in some patients. Bone marrow transplantation patients were reported to be another risk group for severe contrast medium induced skin eruptions. If patients who have previously had a delayed skin reaction to iodinated contrast medium require further contrast medium, it is recommended that an alternative contrast medium is chosen and steroid prophylaxis is given. However, because of frequent cross-reactivity among different contrast media, change of contrast agent is no guarantee against a repeat reaction (1). Conclusion Delayed adverse reactions to iodinated contrast media have been recognized for 20 years. They are mainly mild or moderate skin reactions, which develop from 1 to 7 days after contrast medium administration and usually resolve with 3 to 7 days. Brockow K, Christiansen C, Kanny G et al (2005) Management of hypersensitivity reactions to iodinated contrast media. A retrospective study comparing a non-ionic monomeric contrast medium with a non-ionic dimeric contrast medium. However, it is recommended that patients who have had either a previous delayed skin reaction after contrast medium administration or suffer from major drug or contact allergy are warned about the possibility of a delayed skin reaction and told to contact a doctor if they have a problem. Consider the use of pre-medication, especially in previous contrast medium reactors and high-risk patients. A suitable pre-medication regime is prednisolone 30 mg (or methylprednisolone 32 mg) orally given 12 and 2 h before contrast medium. H2 antihistamines may also be used Characteristics Predisposing Factors the choice of contrast medium and certain patientrelated factors may predispose to an acute idiosyncratic reaction to intravascular iodinated contrast medium. Contrast medium type the use of low osmolality nonionic agents reduces reaction rates by a factor of 4 to 5 compared to high osmolality ionic agents (1). Patient factors (2) A previous reaction to contrast medium is the most important factor predisposing to an acute idiosyncratic reaction. A history of drug or food allergy, or of hayfever or eczema, all increase the risk of reaction but less than asthma.
Syndromes
Differential Diagnosis Between Noninfected and Infected Neuropathic Joint Disease It is often clinically impossible to diagnose infection in acute or subacute neuroarthropathy since both entities present with symptoms such as swelling hiv symptoms eye infection buy generic minipress 2 mg online, redness antivirus windows server 2008 2.5 mg minipress with amex, and tenderness hiv global infection rates order 2 mg minipress free shipping. As a general rule of thumb hiv infection symptoms after 2 years 2 mg minipress amex, the greater and the more extensive the marrow signal abnormality from the articular surface, the more likely the bone is to be superinfected. Therefore, a bone marrow abnormality without contiguous soft-tissue infection or nearby skin ulceration favors diagnoses other than infection. In addition, neuropathic osteoarthropathy is primarily an articular disease; marrow abnormalities centered in a subarticular location favor such an articular disorder. Distribution of osteomyelitis mirrors that of ulceration, which is most common at the toes, metatarsal heads, calcaneus, and malleoli, whereas neuropathic arthropathy is most common at the Lisfranc and Chopart joints. Finally, neuropathic arthropathy tends to involve a number of joints in a region, whereas infection tends to remain localized or spread contiguously. Table 2 Nuclear Medicine Radionuclide imaging can sometimes be a useful investigative tool in pedal neuroarthropathy. It may be difficult to distinguish infection in bone and soft tissue Differentiation of osteomyelitis from neuropathic osteoarthropathy Neuropathic Lisfranc joint, Chopart joint Comments Osteomyelitis Typical location Toes (tips, dorsum), metatarsal heads (especially first and fifth), calcaneus malleoli Focal, local-centripetal spread Predominant involvement of one bone Uncommon (unless there is underlying neuropathic disease) Adjacent ulcer, cellulitis, sinus tract Distribution Pattern of edema/ enhancement Deformity Soft tissues Multiple joints in a region Epicenter in joint and subchondral bone Common (rocker-bottom) Enhancement limited to juxtaarticular Diffuse subcutaneous; soft tissues; skin, subcutaneous tissues edema is typical In intact diabetic feet Neuropathic Joint Disease 1355 Neuropathic Joint Disease. Figure 3 Diagnosis of osteomyelitis in a patient with long-standing neuroarthropathy. There is hypointense signal of the bone marrow of the distal fibula (small white arrow) and calcaneus (long white arrow). Dorsal subluxation of metatarsal bases (white arrow) is indicative of neuropathic arthropathy. Note peroneal tendon phlegmon (black arrow) with diffuse peritendinous enhancement and hypointense pus in the tendon sheath. Bibliography Diagnosis Diagnosis of early neuropathic joint disease may be difficult, especially if a joint above the foot is involved and if the concomitant disease leading to sensory deprivation is unknown to the radiologist. In advanced stages, radiographic changes are almost pathognomonic, displaying Resnick D (2002) Neuropathic osteoarthropathy. It may be spontaneous or induced by expression, and it may be milky, clear, green, dark, grey, brown, and/or bloody. Duct Disease, Breast Neurovascular Conflict Nodal Necrosis A vascular compression of a cranial nerve at the root entry zone that manifests clinically as neuralgia and/or spasm. Strict diagnostic criteria include deviation and/or indentation of the nerve by the offending vessel. Chronic pulsatility and pressure upon this vulnerable area of the nerve lead to segmental areas of axonal ischemia and demyelination. Most common causes include vascular loops, vascular dolichoectasia, aneurysms and vascular malformations. Facial Nerve Palsy Nodal necrosis is a pathognomonic feature for metastatic nodes from head and neck squamous cell carcinomas. Nodal necrosis is considered to occur as cancer cells infiltrate into the medullary portion of the node to surpass the blood supply. Lymphadenopathies, Head and Neck Nodular Adenosis New Neoplasm Breast neoplasms detected during the follow-up of patients previously diagnosed and treated for breast cancer. The characteristic of these tumors is that their location (not close to the primary tumor or the surgical scar, even in the contralateral breast) and their histological characteristics indicate that they are tumors different to that initially diagnosed and treated. Recurrent Neoplasms, Breast Sclerosing Adenosis, Breast Nodular Regenerative Hyperplasia, Hepatic Tumor-like condition of unknown origin, rare in children, usually underdiagnosed because imaging is nonspecific and may resemble focal nodular hyperplasia or may occur as regenerative nodules in cirrhosis. Nodules grouped in a cluster and lying in the lung periphery are more suspicious for an underlying infection. Pulmonary arteriovenous malformations consist of abnormal communications between pulmonary veins and arteries. They present as solitary or in about one-third of patients as multiple intrapulmonary nodules. Strong enhancement after contrast injection and the presence of draining vessels are the diagnostic key features. In most of these cases additional clinical findings and imaging features will help to narrow the differential diagnosis. Yet, distribution, localization and morphological details provide important clues for further differential diagnosis. Pathology/Histopathology the differential diagnosis for multiple pulmonary nodules is long. Metastatic solid organ malignancies are the most common cause of multiple pulmonary nodules and account for about 80% of these cases. Radiology 237:395 N Clinical Presentation Dependent on the extent and on the underlying disease clinical symptoms are very variable. To cause loss of respiratory function the nodules have to be extensive and are mostly associated with other thoracic manifestations such as pleural effusion or airway obstruction. With the history of a known primary, newly developed multiple nodules-mostly but not necessarily spherical and sharply demarcated-are highly suspicious for metastases. Definition A pulmonary nodule, or coin lesion, is defined as a spherical opacity and with well-defined edges, a diameter smaller than 3 cm which is surrounded by lung parenchyma. Clinical Presentation Typically, a solitary pulmonary nodule is an incidental finding in an asymptomatic patient. Imaging Even 1 cm nodules are frequently missed on a chest radiograph dependant on their anatomic location and the amount of overlying "anatomic noise. Radiological imaging features helpful for determining the differential diagnosis of a solitary pulmonary nodule are 1. Calcification: Various types of calcifications are differentiated such as laminated, punctuate, cloud-like eccentric, or concentric. They have a different probability of being associated with a benign lesion or suspicion for malignancy. Uniform, concentric, or popcorn calcifications are typical for benign lesions (tuberculoma, histoplasmoma, hamartoma. The visibility of the calcifications on a chest radiograph depends on their size and whether they are surrounded by soft tissue or air. Attention has to be paid to the proper technique with respect to volume and flow of injected contrast. Rate of growth: Bronchogenic carcinomas have a volume-doubling time between 1 and 18 months. Faster doubling time (<1 month) is suggestive for infection, infarction, lymphoma, or fast growing metastases while a longer doubling time is suggestive for a benign nature of the lesion. Figure 1 A benign intrapulmonary lesion (hamartoma) with a central calcification, a round well-defined margin and a constant size over more than 2 years. Size and shape: While the size is a definite tool for stratifying the next diagnostic steps, the role of shape related criteria such as lobulation, notching (Rigler-sign), irregularity of borders (corona radiata), or the presence of a pleuro-pulmonary tail (pleural finger. They may be used for complex multifactor likelihood calculations but eventually do not replace invasive procedures for histological proof. Air-bronchogram and bubble-like lucencies: An airbronchogram within a solitary pulmonary nodule seen on a chest radiograph makes the diagnosis of a lymphoma, rounded atelectasis, or bronchiolo-alveolar carcinoma more likely than a metastasis or primary lung cancer. More spherical so-called air bubbles are quite common in adenocarcinoma, especially bronchiolo-alveolar carcinoma. Cavitation: It describes an air containing space within a nodule or mass; wall thickness, wall regularity, and the reaction of the surrounding lung parenchyma vary with the underlying etiology. The most frequent differential diagnoses include a neoplasm, an infectious or granulomatous process, or an ischemic lesion. Figure 3 A malignant intrapulmonary lesion with spiculae (corona radiata) and a pleural finger. Pathologically the cavitation is the result of a necrosis of the central portion of the lesion that has been expelled via the bronchial tree, leaving an air filled space with or without a fluid-gas level. Diagnosis the diagnostic work up of a solitary pulmonary nodule depends on the size of the lesion, age of the patient as well as the clinical symptoms and history of the patient. Older 1360 Non-Encapsuled Sclerosing Lesion Non-Bronchial Arteries Non-bronchial arteries frequently involved in hemoptysis or recurrent bleeding include intercostal, inferior phrenic, subclavian, axillary and internal mammary arteries. Figure 4 Patient suffering from neutropenia after chemotherapy and showing multiple intrapulmonary nodules and masses surrounded by a halo due to an angio-invasive aspergillus infection. Lesions larger than 1 cm in diameter require definite diagnostic work up; smaller lesions are followed under specific conditions (see 4).
Enzyme leakage into extra-discal tissue has been reported hiv infection rate dc minipress 1 mg mastercard, with the possibility of damage to nerve roots hiv infection and stages buy minipress 2.5bottles, dural sac or spinal cord hiv infection rates singapore minipress 2.5mg for sale. The overall mortality rate following chymopapain injection is approximately 1 in 5 how long after hiv infection do symptoms occur cheap 2.5mg minipress mastercard,000 patients (0. Ozone has a direct lytic effect on the proteoglycan molecules that form the nucleus pulposus (7). As in chemonucleolysis, the resulting proteoglycan fragments have limited water-binding abilities, which leave intradiscal water molecules free to diffuse into the surrounding tissues (7). The degenerated nucleus pulposus tissue is gradually replaced by fibrous tissue, with limited water-binding capabilities. In addition to the proteolytic properties, ozone also has certain anti-inflammatory and analgesic effects that may help counteract disc-induced pain. The antiseptic activity of ozone is thought to further reduce the risk of infectious complications associated with percutaneous interventions (7). Nucleoplasty Nucleoplasty is one of the newest percutaneous interventions for radicular syndrome. In nucleoplasty, nucleus pulposus tissue is ablated using a special wand, which is inserted into the centre of the intervertebral disc under fluoroscopic guidance. By rotating the curved tip of the wand, up to six channels are created within the nucleus pulposus, decreasing intradiscal volume and hence lowering intradiscal pressure. The results of several non-randomised trials show success rates that vary from 78% to 89% (5). Percutaneous Nucleotomy Percutaneous nucleotomy is a minimally invasive intervention, in which nucleus pulposus material is mechanically removed using an automated nucleotome. This nucleotome is a 2-mm blunt-tipped device, equipped with a reciprocating suction cutter (6). The nucleotome is introduced through a cannula that is placed into the centre of the nucleus pulposus under fluoroscopic guidance. When the nucleotome is in place, nucleus pulposus material is cut and aspirated at a rate of 180 times per minute. The tip of the nucleotome is alternatingly rotated, depressed and elevated within the nucleus in order to optimise the removed amount of nucleus pulposus material (6). Serious neurological complications are extremely rare, although two cases of cauda equina injuries have been reported due to probe misplacement (6). A small laser fibre is inserted through a hollow needle into the centre of the intervertebral disc under fluoroscopic guidance. When the laser fibre is in place, up to 2,000 J of laser energy are applied into the nucleus pulposus in order to evaporate its water content, thereby reducing intradiscal pressure. The temperature increase also induces protein denaturation and subsequent renaturation. This causes a structural change of the nucleus pulposus, limiting its capability to attract water and therefore leading to a permanent reduction of intradiscal pressure (3, 4). The results of several non-randomised trials that have been published over the years show success rates ranging from 75% to 87% (4). This complication can be largely avoided with careful monitoring of patient complaints during the procedure, with adjustment of laser parameters when heat sensations occur. In this fashion, an excessive buildup of heat can be countered before structural damage is caused to the surrounding tissues. However when conservative treatment fails, surgery is an option depending on preferences of patients and their treating physicians. Cervical and thoracic radicular syndromes are managed conservatively for a longer period. Complaints in these cases are as severe as in lumbar radicular syndromes, but the functional disability seems more tolerable and a higher proportion of patients are cured in the natural course of the disease. Severe neurological deficit is a compelling reason for surgery, whereas pain is a relative indication. As a rule compression occurs far laterally with anterior impingement of the nerve. All anatomical approaches have been used, employing posterior, lateral and anterior techniques. A laminectomy consists of the complete removal of posterior bony elements except for the facet joint. This historical technique is occasionally used in present times, when patients present with a combined radicular and spinal cord compression. The exiting nerve root is decompressed by the removal of the posterior medial facet joint. If the procedure is solely intended to decompress the nerve root, a small hole may be drilled in this area, leaving the posterior elements intact. Lateral approaches to the cervical spine for the treatment of radicular syndromes have historical interest but are sometimes used for more complex pathologies compressing the exiting root. The anterior approach presently comprises more than 90% of all surgical techniques employed in cervical radicular syndromes. The main reason for this is the origin of the pathology anterior to the root and cord, and the sparing nature of the technique leaving intact all spinal anatomical structures except for the disc. The latter is removed including osteophytes which may be present, and the posterior longitudinal ligament is Synonyms Laminectomy; (Micro)discectomy Definition A radicular syndrome is characterized by pain radiating in the dermatome of a spinal nerve root. Pain may be accompanied by one or more of the following: lumbar muscle spasm, reflex abnormalities, motor and sensory disturbances. Surgical therapy for a radicular syndrome refers to all procedures which have the goal to decompress the exiting nerve roots. Pathology Disc herniations are the most frequent cause of a radicular syndrome, followed by stenosis of the lateral recess and occasionally narrowing of the neuroforamen. The latter occur more frequently in the cervical spine in elderly populations, where progressive disc degeneration leads to spine deformities with compression at the spinal outlet of nerve. Disc herniations can be divided into contained and uncontained protrusions of nuclear material, and the latter may give rise to a sequester or free fragment of disc material. In the past, autologous bone from the iliac crest was used to fill the gap in the open disc space. Pain in the iliac crest area directed surgeons to the use of cement and later to cages filled with bone, the latter followed by an anterior plate and screw fixation of both vertebrae in some countries. Recently, disc prostheses have been used with the goal of preserving cervical mobility and thus preventing future disc degeneration at adjacent levels. To emphasize the variety of procedures used for the same disease, it can be noted that many surgeons prefer to perform a discectomy without any graft, cement, cage, or prosthesis. Lack of scientific data and huge industrial influence are the main reasons for this lack of consensus. Randomized trials are started to provide better insight in the value and (cost-)effectiveness of the different techniques. The timing of surgery is subject of a randomized trial in Europe (2), whereas a trial in the United States sets out to determine the effectiveness of surgery compared to conservative treatment (3). Surgical interventions can be divided into percutaneous techniques indirectly decompressing the nerve root by intradiscal action and posterior surgical techniques, actually removing the disc herniation and therefore direct decompression. After the first description in 1934 of removal of a lumbar disc herniation by laminectomy (4), this technique was the method of choice for many years.
In this article hiv infection by age group cheap 1mg minipress fast delivery, we were only able to cite a few of hundreds of malformations anti viral cleanse order 1mg minipress with amex, which are increasingly being associated with specific genetic findings antiviral y retroviral order 2mg minipress mastercard. In the equinus tibiocalcaneal relationship oregano antiviral purchase 2mg minipress overnight delivery, often due to a tight heel cord, the front of the calcaneus is lower than normal in its relationship to the tibia, resembling the "q" in the front of the lower case word equinus that extends below the row of the other letters; in the calcaneus tibiocalcaneal relationship, the front of the calcaneus is higher than normal, like the "l" of the lower case word calcaneus. In a valgus relationship, the distal part heads further from the midline than normal compared to the proximal part, judged with the proximal part in anatomic position; in varus, the distal part heads closer to the midline than normal. Mnemonic: the varus proximal right femur looks like a lower case "r" and the valgus right femur looks like a lower case "l. Several genes, proteins, and molecules are involved in the various stages of cerebellar development, and it is expected that this knowledge will influence the classification of congenital cerebellar malformations in the future. Figure 2 Calcaneus and equinus mnemonic diagram, by Tamar Kahane Oestreich, see text. Thieme Verlag, Stuttgart p 115) Pathology/Histopathology Although the anatomy of the cerebellum is straightforward, the understanding of embryology is still limited. Congenital Malformations, Cerebellar 395 Approximately during the fourth week of gestation, the rhombencephalon divides into the metencephalon (pons and cerebellum) and the myelencephalon (medulla oblongata). The metencephalon will give rise to the vermis and the hemispheres, while the cavity in the rhombencephalon will expand to become the fourth ventricle. The roof of the fourth ventricle is divided into an anterior and a posterior membranous area; the posterior membranous area will ultimately communicate with the subarachnoid space at the foramen of Magendie. In the formation of the cerebellar cortex, there is first an outward migration of the Purkinje cells and granular cells. The foliation and fissuration occur at least partly simultaneously and are triggered by the migration of Purkinje and granular cells. These processes explain at least to some extent the malformations of fissuration and foliation. Imaging in different planes is required, and if available, three-dimensional T2-weighted images can be helpful. A classification is not yet available today, but using knowledge of anatomy, embryology, and histopathology, a provisional classification can be presented. The two groups of cerebellar malformations are cerebellar hypoplasia and cerebellar dysgenesis. Cerebellar dysgenesis can further be divided into vermian and/or hemispheric dysgenesis. It seems inevitable that there will be some overlap between the two groups of malformations. The Chiari malformations are not included in the classification and are discussed separately. C Diagnosis the imaging aspects of the common cerebellar malformations will be briefly reviewed. The Chiari I malformation is defined as a caudal herniation of the cerebellar tonsils over a distance of at least 5 mm through the foramen magnum (below a line from the basion to the opisthion on a sagittal image;. This malformation is likely to be the result of an abnormally small posterior fossa and/or the occurrence of craniovertebral anomalies. The posterior fossa remains too small, and the cerebellum extends downward, upward, and around the brainstem. Not only the tonsils but parts of the vermis and even the fourth ventricle can herniate through the foramen magnum. It consists of (i) a variable degree of vermian agenesis, (ii) a dilatation of the fourth ventricle with cyst formation, and (iii) an enlarged posterior fossa. It is thought that a genetic mutation causes an abnormal development of the roof of the fourth ventricle. Cerebellar abnormalities will usually cause cerebellar signs and symptoms, such as ataxia, cranial nerve palsies, delayed language and speech development, eye movement disorders (nystagmus, oculomotor dyspraxia, and so on), and head/body turning attacks. Epilepsy and mild cognitive deterioration can also be part of the clinical spectrum. The Chiari I malformation appears to be asymptomatic in up to 14% of the patients in a large series. The typical symptom is occipital headache when coughing or otoneurological disturbances, but the presentation is often more ambiguous. Joubert syndrome is a separate entity within the molar tooth malformations and is characterized by episodic hyperpnea, abnormal eye movements, ataxia, and mental retardation. Computed tomography is not suited to assess intrinsic 396 Congenital Malformations, Cerebellar Congenital Malformations, Cerebellar. Note the herniation of the cerebellar tonsils through the foramen magnum reaching the level of the endplate of C2. Note the displacement of the fourth ventricle and the herniation of cerebellar tissue to the level of C3. This malformation resembles megacisterna magna, but hydrocephalus is not seen in the latter. A late opening of the foramen of Magendie has been suggested as an underlying cause. Arachnoid cysts in the posterior fossa can resemble a megacisterna magna, but they usually cause symptoms and are often located laterally in the posterior fossa. These malformations are named after the molar tooth appearance of the midbrain on axial images (. This is due to the horizontal course of the superior cerebellar peduncles (due to a lack of decussation of the superior cerebellar peduncles) and a narrow pontomesencephalic junction. Rhombencephalosynapsis consists of vermian agenesis or severe hypogenesis, fusion of the hypoplastic cerebellar hemispheres, and fusion of the dentate nuclei. Dilated lateral ventricles, fusion of the thalami, and absence of the septum pellucidum can be associated. The disorder is possibly induced by a genetic mutation of the Lmx 1a gene, which regulates events at the pontomesencephalic junction between the fourth and the sixth weeks of gestation. Because of this early timing, metencephalosynapsis might be a more appropriate term. There is an upward rotation of the remaining part of the superior vermis, and there is a large posterior fossa cyst. Note the displacement of the sinus rectus and the hypogenesis of the corpus callosum. There is a large communication between the fourth ventricle and the posterior fossa cyst. There is a large communication between the fourth ventricle and the subarachnoid space, and there is supratentorial hydrocephalus. Recently, a series of abnormalities have been reported consisting of vermian and/or hemispheric dysgenesis. When only the vermian fissures are involved, this is almost always an asymptomatic incidental finding (type 1a;. Some patients also have an abnormal foliation of the anterior lobe and part of the posterior lobe of the vermis (type 1b). In abnormalities of foliation and fissuration type 2, three different hemispheric malformations can be recognized: (i) cortical dysgenesis, (ii) cortical hypertrophy, and (iii) aberrant orientation of the folia. In 60% of the children with type 2 abnormalities, type 1b abnormalities are present, and more than 50% of these children have congenital cerebral anomalies. Although the lesion is classified as a dysplastic gangliocytoma according to 398 Congenital Malformations, Cerebellar Congenital Malformations, Cerebellar. Note the molar tooth appearance due to the horizontal course of the hypoplastic superior cerebellar peduncles. The cortical dysgenesis is clearly visible in the left hypoplastic cerebellar hemisphere compared with the normal right hemisphere. A masslike lesion is observed in the right cerebellar hemisphere with a striated folial pattern.
Generic minipress 2 mg without prescription. If the blood supply to HIV infection.