



|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Jamie Poust, PharmD, BCOP
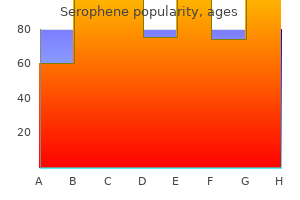
Anteriorly directed myometrial contractions also occur near the time of ovulation breast cancer awareness quotes cheap serophene 50mg otc, and are thought to possibly facilitate the transport of sperm through the female reproductive tract menstruation back pain discount serophene 100 mg mastercard. The endometrium contains a connective tissue lining menstruation zu lange cheap serophene 50mg amex, the lamina propria menopause the musical songs buy serophene 100 mg lowest price, which is covered by epithelial tissue that lines the lumen breast cancer keychains safe serophene 100mg. Structurally women's health clinic vienna austria buy serophene 25mg visa, the endometrium consists of two layers: the stratum basalis and the stratum functionalis (the basal and functional layers). The stratum basalis layer is part of the lamina propria and is adjacent to the myometrium; this layer does not shed during menses. In contrast, the thicker stratum functionalis layer contains the glandular portion of the lamina propria and the endothelial tissue that lines the uterine lumen. It is the stratum functionalis that grows and thickens in response to increased levels of estrogen and progesterone. In the luteal phase of the menstrual cycle, special branches off of the uterine artery called spiral arteries supply the thickened stratum functionalis. This inner functional layer provides the proper site of implantation for the fertilized egg, and-should fertilization not occur-it is only the stratum functionalis layer of the endometrium that sheds during menstruation. Recall that during the follicular phase of the ovarian cycle, the tertiary follicles are growing and secreting estrogen. At the same time, the stratum functionalis of the endometrium is thickening to prepare for a potential implantation. The postovulatory increase in progesterone, which characterizes the luteal phase, is key for maintaining a thick stratum functionalis. As long as a functional corpus luteum is present in the ovary, the endometrial lining is prepared for implantation. Indeed, if an embryo implants, signals are sent to the corpus luteum to continue secreting progesterone to maintain the endometrium, and thus maintain the pregnancy. If an embryo does not implant, no signal is sent to the corpus luteum and it degrades, ceasing progesterone production and ending the luteal phase. Without progesterone, the endometrium thins and, under the influence of prostaglandins, the spiral arteries of the endometrium constrict and rupture, preventing oxygenated blood from reaching the endometrial tissue. As a result, endometrial tissue dies and blood, pieces of the endometrial tissue, and white blood cells are shed through the vagina during menstruation, or the menses. The first menses after puberty, called menarche, can occur either before or after the first ovulation. The Menstrual Cycle Now that we have discussed the maturation of the cohort of tertiary follicles in the ovary, the build-up and then shedding of the endometrial lining in the uterus, and the function of the uterine tubes and vagina, we can put everything together to talk about the three phases of the menstrual cycle-the series of changes in which the uterine lining is shed, rebuilds, and prepares for implantation. Cycle length is determined by counting the days between the onset of bleeding in two subsequent cycles. However, the length of the menstrual cycle varies among women, and even in the same woman from one cycle to the next, typically from 21 to 32 days. Just as the hormones produced by the granulosa and theca cells of the ovary "drive" the follicular and luteal phases of the ovarian cycle, they also control the three distinct phases of the menstrual cycle. Menses Phase the menses phase of the menstrual cycle is the phase during which the lining is shed; that is, the days that the woman menstruates. Although it averages approximately five days, the menses phase can last from 2 to 7 days, or longer. Recall that progesterone concentrations decline as a result of the degradation of the corpus luteum, marking the end of the luteal phase. This decline in progesterone triggers the shedding of the stratum functionalis of the endometrium. Ovulation marks the end of the proliferative phase as well as the end of the follicular phase. High estrogen levels also slightly decrease the acidity of the vagina, making it more hospitable to sperm. In the ovary, the luteinization of the granulosa cells of the collapsed follicle forms the progesteroneproducing corpus luteum, marking the beginning of the luteal phase of the ovarian cycle. In the uterus, progesterone from the corpus luteum begins the secretory phase of the menstrual cycle, in which the endometrial lining prepares for implantation (see Figure 27. If fertilization has occurred, this fluid will nourish the ball of cells now developing from the zygote. At the same time, the spiral arteries develop to provide blood to the thickened stratum functionalis. If no pregnancy occurs within approximately 10 to 12 days, the corpus luteum will degrade into the corpus albicans. These women ranged in age from 14 to 59 years and differed in race, ethnicity, and number of sexual partners. In some cases, however, the virus continues to spread and becomes an invasive cancer. The prevalence of cervical cancer in the United States is very low because of regular screening exams called pap smears. However, women in developing countries often do not have access to regular pap smears. As a result, these women account for as many as 80 percent of the cases of cervical cancer worldwide. Unfortunately, the high cost of manufacturing the vaccine is currently limiting access to many women worldwide. The Breasts Whereas the breasts are located far from the other female reproductive organs, they are considered accessory organs of the female reproductive system. The external features of the breast include a nipple surrounded by a pigmented areola (Figure 27. The areola is typically circular and can vary in size from 25 to 100 mm in diameter. The areolar region is characterized by small, raised areolar glands that secrete lubricating fluid during lactation to protect the nipple from chafing. When a baby nurses, or draws milk from the breast, the entire areolar region is taken into the mouth. The milk itself exits the breast through the nipple via 15 to 20 lactiferous ducts that open on the surface of the nipple. These lactiferous ducts each extend to a lactiferous sinus that connects to a glandular lobe within the breast itself that contains groups of milk-secreting cells in clusters called alveoli (see Figure 27. The clusters can change in size depending on the amount of milk in the alveolar lumen. Hormonal Birth Control Birth control pills take advantage of the negative feedback system that regulates the ovarian and menstrual cycles to stop ovulation and prevent pregnancy. Although the estrogen in birth control pills does stimulate some thickening of the endometrial wall, it is reduced compared with a normal cycle and is less likely to support implantation. Some birth control pills contain 21 active pills containing hormones, and 7 inactive pills (placebos). The decline in hormones during the week that the woman takes the placebo pills triggers menses, although it is typically lighter than this content is available for free at cnx. Newer types of birth control pills have been developed that deliver low-dose estrogens and progesterone for the entire cycle (these are meant to be taken 365 days a year), and menses never occurs. While some women prefer to have the proof of a lack of pregnancy that a monthly period provides, menstruation every 28 days is not required for health reasons, and there are no reported adverse effects of not having a menstrual period in an otherwise healthy individual. It is important, therefore, that the woman follow the directions on the birth control pill package to successfully prevent pregnancy. Female Reproductive System Female fertility (the ability to conceive) peaks when women are in their twenties, and is slowly reduced until a women reaches 35 years of age. After that time, fertility declines more rapidly, until it ends completely at the end of menopause. Menopause is the cessation of the menstrual cycle that occurs as a result of the loss of ovarian follicles and the hormones that they produce. A woman is considered to have completed menopause if she has not menstruated in a full year. Poor health, including smoking, can lead to earlier loss of fertility and earlier menopause. As a woman reaches the age of menopause, depletion of the number of viable follicles in the ovaries due to atresia affects the hormonal regulation of the menstrual cycle. Eventually, this process leads to the depletion of all follicles in the ovaries, and the production of estrogen falls off dramatically. Although the levels of estrogen are still nearly the same as before the transition, the level of progesterone produced by the corpus luteum is reduced. This decline in progesterone can lead to abnormal growth, or hyperplasia, of the endometrium. This condition is a concern because it increases the risk of developing endometrial cancer. Two harmless conditions that can develop during the transition are uterine fibroids, which are benign masses of cells, and irregular bleeding. As estrogen levels change, other symptoms that occur are hot flashes and night sweats, trouble sleeping, vaginal dryness, mood swings, difficulty focusing, and thinning of hair on the head along with the growth of more hair on the face. Depending on the individual, these symptoms can be entirely absent, moderate, or severe. Cardiovascular disease becomes as prevalent in women as in men, possibly because estrogens reduce the amount of cholesterol in the blood vessels. When estrogen is lacking, many women find that they suddenly have problems with high cholesterol and the cardiovascular issues that accompany it. Osteoporosis is another problem because bone density decreases rapidly in the first years after menopause. The potential positive effects on cardiovascular disease were also not realized in the estrogen-only patients. The results of other hormone replacement studies over the last 50 years, including a 2012 study that followed over 1,000 menopausal women for 10 years, have shown cardiovascular benefits from estrogen and no increased risk for cancer. Some researchers believe that the age group tested in the 2002 trial may have been too old to benefit from the therapy, thus skewing the results. In the meantime, intense debate and study of the benefits and risks of replacement therapy is ongoing. Reproductive development continues in utero, but there is little change in the reproductive system between infancy and puberty. Development of the Sexual Organs in the Embryo and Fetus Females are considered the "fundamental" sex-that is, without much chemical prompting, all fertilized eggs would develop into females. To become a male, an individual must be exposed to the cascade of factors initiated by a single gene on the male Y chromosome. In both male and female embryos, the same group of cells has the potential to develop into either the male or female gonads; this tissue is considered bipotential. Soon after the formation of the testis, the Leydig cells begin to secrete testosterone. Testosterone can influence tissues that are bipotential to become male reproductive structures. For example, with exposure to testosterone, cells that could become either the glans penis or the glans clitoris form the glans penis. The internal reproductive structures (for example the uterus, uterine tubes, and part of the vagina in females; and the epididymis, ductus deferens, and seminal vesicles in males) form from one of two rudimentary duct systems in the embryo. For proper reproductive function in the adult, one set of these ducts must develop properly, and the other must degrade. At the same time, testosterone secretion stimulates growth of the male tract, the Wolffian duct. For more information and a figure of differentiation of the gonads, seek additional content on fetal development. Though the outcomes of puberty for boys and girls are very different, the hormonal control of the process is very similar. In addition, though the timing of these events varies between individuals, the sequence of changes that occur is predictable for male and female adolescents. In pre-pubertal children, the sensitivity of the negative feedback system in the hypothalamus and pituitary is very high. In addition to age, multiple factors can affect the age of onset of puberty, including genetics, environment, and psychological stress. One of the more important influences may be nutrition; historical data demonstrate the effect of better and more consistent nutrition on the age of menarche in girls in the United States, which decreased from an average age of approximately 17 years of age in 1860 to the current age of approximately 12. Some studies indicate a link between puberty onset and the amount of stored fat in an individual. Body fat, corresponding with secretion of the hormone leptin by adipose cells, appears to have a strong role in determining menarche. This may reflect to some extent the high metabolic costs of gestation and lactation. In girls who are lean and highly active, such as gymnasts, there is often a delay in the onset of puberty. Signs of Puberty Different sex steroid hormone concentrations between the sexes also contribute to the development and function of secondary sexual characteristics. Development of the Secondary Sexual Characteristics Male Increased larynx size and deepening of the voice Increased muscular development Growth of facial, axillary, and pubic hair, and increased growth of body hair Table 27. A growth spurt normally starts at approximately age 9 to 11, and may last two years or more.
Cannon expanded the idea womens health 06484 cheap serophene 50 mg amex, and introduced the idea that an animal responds to a threat by preparing to stand and fight or run away women's health clinic nambour cheap serophene 100 mg. The nature of this response was thoroughly explained in a book on the physiology of pain breast cancer awareness products cheap 50mg serophene with amex, hunger women's health clinic colorado springs discount 100 mg serophene fast delivery, fear women's health and wellness issues buy generic serophene 100mg on-line, and rage encyclopedia of women's health issues serophene 25 mg generic. When students learn about the sympathetic system and the fight-or-flight response, they often stop and wonder about other responses. If you were faced with a lioness running toward you as pictured at the beginning of this chapter, would you run or would you stand your ground The common epithet of "fight or flight" is being enlarged to be "fight, flight, or fright" or even "fight, flight, fright, or freeze. The sympathetic system is responsible for the physiological responses to emotional states. The name "sympathetic" can be said to mean that (sym- = "together"; -pathos = "pain," "suffering," or "emotion"). As described in this video, the nervous system has a way to deal with threats and stress that is separate from the conscious control of the somatic nervous system. This video describes how the autonomic system is only part of the response to threats, or stressors. The main difference between the somatic and autonomic systems is in what target tissues are effectors. The autonomic system, however, targets cardiac and smooth muscle, as well as glandular tissue. Whereas the basic circuit is a reflex arc, there are differences in the structure of those reflexes for the somatic and autonomic systems. The Structure of Reflexes One difference between a somatic reflex, such as the withdrawal reflex, and a visceral reflex, which is an autonomic reflex, is in the efferent branch. The output of a somatic reflex is the lower motor neuron in the ventral horn of the spinal cord that projects directly to a skeletal muscle to cause its contraction. The output of a visceral reflex is a two-step pathway starting with the preganglionic fiber emerging from a lateral horn neuron in the spinal cord, or a cranial nucleus neuron in the brain stem, to a ganglion-followed by the postganglionic fiber projecting to a target effector. The other part of a reflex, the afferent branch, is often the same between the two systems. Somatic reflexes, for instance, involve a direct connection from the ventral horn of the spinal cord to the skeletal muscle. Visceral reflexes involve a projection from the central neuron to a ganglion, followed by a second projection from the ganglion to the target effector. Afferent Branch the afferent branch of a reflex arc does differ between somatic and visceral reflexes in some instances. Many of the inputs to visceral reflexes are from special or somatic senses, but particular senses are associated with the viscera that are not part of the conscious perception of the environment through the somatic nervous system. For example, there is a specific type of mechanoreceptor, called a baroreceptor, in the walls of the aorta and carotid sinuses that senses the stretch of those organs when blood volume or pressure increases. You do not have a conscious perception of having high blood pressure, but that is an important afferent branch of the cardiovascular and, particularly, vasomotor reflexes. The baroreceptor apparatus is part of the ending of a unipolar neuron that has a cell body in a sensory ganglion. The baroreceptors from the carotid arteries have axons in the glossopharyngeal nerve, and those from the aorta have axons in the vagus nerve. The sensory homunculus-the representation of the body in the primary somatosensory cortex-only has a small region allotted for the perception of internal stimuli. If you swallow a large bolus of food, for instance, you will probably feel the lump of that food as it pushes through your esophagus, or even if your stomach is distended after a large meal. If you inhale especially cold air, you can feel it as it enters your larynx and trachea. These sensations are not the same as feeling high blood pressure or blood sugar levels. When particularly strong visceral sensations rise to the level of conscious perception, the sensations are often felt in unexpected places. For example, strong visceral sensations of the heart will be felt as pain in the left shoulder and left arm. This irregular pattern of projection of conscious perception of visceral sensations is called referred pain. Depending on the organ system affected, the referred pain will project to different areas of the body (Figure 15. The location of referred pain is not random, but a definitive explanation of the mechanism has not been established. The most broadly accepted theory for this phenomenon is that the visceral sensory fibers enter into the same level of the spinal cord as the somatosensory fibers of the referred pain location. By this explanation, the visceral sensory fibers from the mediastinal region, where the heart is located, would enter the spinal cord at the same level as the spinal nerves from the shoulder and arm, so the brain misinterprets the sensations from the mediastinal region as being from the axillary and brachial regions. Projections from the medial and inferior divisions of the cervical ganglia do enter the spinal cord at the middle to lower cervical levels, which is where the somatosensory fibers enter. Some sensations are felt locally, whereas others are perceived as affecting areas that are quite distant from the involved organ. The spleen is in the upper-left abdominopelvic quadrant, but the pain is more in the shoulder and neck. The sympathetic fibers connected to the spleen are from the celiac ganglion, which would be from the mid-thoracic to lower thoracic region whereas parasympathetic fibers are found in the vagus nerve, which connects in the medulla of the brain stem. However, the neck and shoulder would connect to the spinal cord at the mid-cervical level of the spinal cord. These connections do not fit with the expected correspondence of visceral and somatosensory fibers entering at the same level of the spinal cord. The incorrect assumption would be that the visceral sensations are coming from the spleen directly. The motor fibers that make up this nerve are responsible for the muscle contractions that drive ventilation. These fibers have left the spinal cord to enter the phrenic nerve, meaning that spinal cord damage below the mid-cervical level is not fatal by making ventilation impossible. Therefore, the visceral fibers from the diaphragm enter the spinal cord at the same level as the somatosensory fibers from the neck and shoulder. The visceral sensation is actually in the diaphragm, so the referred pain is in a region of the body that corresponds to the diaphragm, not the spleen. Efferent Branch the efferent branch of the visceral reflex arc begins with the projection from the central neuron along the preganglionic fiber. This fiber then makes a synapse on the ganglionic neuron that projects to the target effector. The effector organs that are the targets of the autonomic system range from the iris and ciliary body of the eye to the urinary bladder and reproductive organs. The thoracolumbar output, through the various sympathetic ganglia, reaches all of these organs. The cranial component of the parasympathetic system projects from the eye to part of the intestines. The sacral component picks up with the majority of the large intestine and the pelvic organs of the urinary and reproductive systems. Visceral reflexes that involve the thoracolumbar or craniosacral systems share similar connections. A long reflex has afferent branches that enter the spinal cord or brain and involve the efferent branches, as previously explained. A short reflex is completely peripheral and only involves the local integration of sensory input with motor output (Figure 15. The short reflex involves the direct stimulation of a postganglionic fiber by the sensory neuron, whereas the long reflex involves integration in the spinal cord or brain. Because the efferent branch of a visceral reflex involves two neurons-the central neuron and the ganglionic neuron-a "short circuit" can be possible. A division of the nervous system that is related to the autonomic nervous system is the enteric nervous system. The word enteric refers to the digestive organs, so this represents the nervous tissue that is part of the digestive system. There are a few myenteric plexuses in which the nervous tissue in the wall of the digestive tract organs can directly influence digestive function. If stretch receptors in the stomach are activated by the filling and distension of the stomach, a short reflex will directly activate the smooth muscle fibers of the stomach wall to increase motility to digest the excessive food in the stomach. That neuron, connected to the smooth muscle, is a postganglionic parasympathetic neuron that can be controlled by a fiber found in the vagus nerve. In the end, one expert, one question, and a simple blood pressure cuff answers the question. Balance in Competing Autonomic Reflex Arcs the autonomic nervous system is important for homeostasis because its two divisions compete at the target effector. The balance of homeostasis is attributable to the competing inputs from the sympathetic and parasympathetic divisions (dual innervation). At the level of the target effector, the signal of which system is sending the message is strictly chemical. A signaling molecule binds to a receptor that causes changes in the target cell, which in turn causes the tissue or organ to respond to the changing conditions of the body. Competing Neurotransmitters the postganglionic fibers of the sympathetic and parasympathetic divisions both release neurotransmitters that bind to receptors on their targets. For any given target, the difference in which division of the autonomic nervous system is exerting control is just in what chemical binds to its receptors. In the sympathetic system, there are exceptions to this pattern of dual innervation. This does not create any problem because there is no parasympathetic input to the sweat glands. At most of the other targets of the autonomic system, the effector response is based on which neurotransmitter is released and what receptor is present. For example, regions of the heart that establish heart rate are contacted by postganglionic fibers from both systems. If norepinephrine is released onto those cells, it binds to an adrenergic receptor that causes the cells to depolarize faster, and the heart rate increases. Without this parasympathetic input, the heart would work at a rate of approximately 100 beats per minute (bpm). Photoreceptors are activated, and the signal is transferred to the retinal ganglion cells that send an action potential along the optic nerve into the diencephalon. If light levels are low, the sympathetic system sends a signal out through the upper thoracic spinal cord to the superior cervical ganglion of the sympathetic chain. The postganglionic fiber then projects to the iris, where it releases norepinephrine onto the radial fibers of the iris (a smooth muscle). When those fibers contract, the pupil dilates-increasing the amount of light hitting the retina. When those fibers contract, the pupil constricts to limit the amount of light hitting the retina. The output of the sympathetic system projects through the superior cervical ganglion, whereas the parasympathetic system originates out of the midbrain and projects through the oculomotor nerve to the ciliary ganglion, which then projects to the iris. The postganglionic fibers of either division release neurotransmitters onto the smooth muscles of the iris to cause changes in the pupillary size. In this example, the autonomic system is controlling how much light hits the retina. It is a homeostatic reflex mechanism that keeps the activation of photoreceptors within certain limits. In the context of avoiding a threat like the lioness on the savannah, the sympathetic response for fight or flight will increase pupillary diameter so that more light hits the retina and more visual information is available for running away. Likewise, the parasympathetic response of rest reduces the amount of light reaching the retina, allowing the photoreceptors to cycle through bleaching and be regenerated for further visual perception; this is what the homeostatic process is attempting to maintain. What constitutes the afferent and efferent branches of the competing reflex (dilation) Autonomic Tone Organ systems are balanced between the input from the sympathetic and parasympathetic divisions. When something upsets that balance, the homeostatic mechanisms strive to return it to its regular state. For each organ system, there may be more of a sympathetic or parasympathetic tendency to the resting state, which is known as the autonomic tone of the system. Because the resting heart rate is the result of the parasympathetic system slowing the heart down from its intrinsic rate of 100 bpm, the heart can be said to be in parasympathetic tone. In a similar fashion, another aspect of the cardiovascular system is primarily under sympathetic control. Blood pressure is partially determined by the contraction of smooth muscle in the walls of blood vessels. These tissues have adrenergic receptors that respond to the release of norepinephrine from postganglionic sympathetic fibers by constricting and increasing blood pressure. The hormones released from the adrenal medulla-epinephrine and norepinephrine-will also bind to these receptors. Those hormones travel through the bloodstream where they can easily interact with the receptors in the vessel walls. The parasympathetic system has no significant input to the systemic blood vessels, so the sympathetic system determines their tone. There are a limited number of blood vessels that respond to sympathetic input in a different fashion.
Membranes menopause kim cattrall serophene 25 mg with amex, Surface Features menopause black cohosh 50mg serophene for sale, and Layers Our exploration of more in-depth heart structures begins by examining the membrane that surrounds the heart pregnancy 0-2 weeks order serophene 100mg on-line, the prominent surface features of the heart pregnancy rash on stomach 25 mg serophene otc, and the layers that form the wall of the heart womens health skinny pill generic serophene 100 mg with mastercard. Membranes the membrane that directly surrounds the heart and defines the pericardial cavity is called the pericardium or pericardial sac pregnancy quickening serophene 25mg discount. It also surrounds the "roots" of the major vessels, or the areas of closest proximity to the heart. The pericardium, which literally translates as "around the heart," consists of two distinct sublayers: the sturdy outer fibrous pericardium and the inner serous pericardium. The fibrous pericardium is made of tough, dense connective tissue that protects the heart and maintains its position in the thorax. The more delicate serous pericardium consists of two layers: the parietal pericardium, which is fused to the fibrous pericardium, and an inner visceral pericardium, or epicardium, which is fused to the heart and is part of the heart wall. The pericardial cavity, filled with lubricating serous fluid, lies between the epicardium and the pericardium. However, in the case of the heart, it is not a microscopic layer but rather a macroscopic layer, consisting of a simple squamous epithelium called a mesothelium, reinforced with loose, irregular, or areolar connective tissue that attaches to the pericardium. This mesothelium secretes the lubricating serous fluid that fills the pericardial cavity and reduces friction as the heart contracts. Heart: Cardiac Tamponade If excess fluid builds within the pericardial space, it can lead to a condition called cardiac tamponade, or pericardial tamponade. With each contraction of the heart, more fluid-in most instances, blood-accumulates within the pericardial cavity. However, the excess fluid in the pericardial cavity puts pressure on the heart and prevents full relaxation, so the chambers within the heart contain slightly less blood as they begin each heart cycle. Surface Features of the Heart Inside the pericardium, the surface features of the heart are visible, including the four chambers. There is a superficial leaflike extension of the atria near the superior surface of the heart, one on each side, called an auricle-a name that means "ear like"-because its shape resembles the external ear of a human (Figure 19. Also prominent is a series of fat-filled grooves, each of which is known as a sulcus (plural = sulci), along the superior surfaces of the heart. The anterior interventricular sulcus is visible on the anterior surface of the heart, whereas the posterior interventricular sulcus is visible on the posterior surface of the heart. From superficial to deep, these are the epicardium, the myocardium, and the endocardium (see Figure 19. The outermost layer of the wall of the heart is also the innermost layer of the pericardium, the epicardium, or the visceral pericardium discussed earlier. It is built upon a framework of collagenous fibers, plus the blood vessels that supply the myocardium and the nerve fibers that help regulate the heart. It is the contraction of the myocardium that pumps blood through the heart and into the major arteries. Deeper ventricular muscles also form a figure 8 around the two ventricles and proceed toward the apex. In order to overcome the high resistance required to pump blood into the long systemic circuit, the left ventricle must generate a great amount of pressure. The right ventricle does not need to generate as much pressure, since the pulmonary circuit is shorter and provides less resistance. Both ventricles pump the same amount of blood, but the left ventricle must generate a much greater pressure to overcome greater resistance in the systemic circuit. The innermost layer of the heart wall, the endocardium, is joined to the myocardium with a thin layer of connective tissue. It is made of simple squamous epithelium called endothelium, which is continuous with the endothelial lining of the blood vessels (see Figure 19. Once regarded as a simple lining layer, recent evidence indicates that the endothelium of the endocardium and the coronary capillaries may play active roles in regulating the contraction of the muscle within the myocardium. The endothelium may also regulate the growth patterns of the cardiac muscle cells throughout life, and the endothelins it secretes create an environment in the surrounding tissue fluids that regulates ionic concentrations and states of contractility. The foramen ovale allowed blood in the fetal heart to pass directly from the right atrium to the left atrium, allowing some blood to bypass the pulmonary circuit. Unlike the interatrial septum, the interventricular septum is normally intact after its formation during fetal development. It is substantially thicker than the interatrial septum, since the ventricles generate far greater pressure when they contract. The septum between the atria and ventricles is known as the atrioventricular septum. Located in each of these openings between the atria and ventricles is a valve, a specialized structure that ensures one-way flow of blood. In this figure, the atrioventricular septum has been removed to better show the bicupid and tricuspid valves; the interatrial septum is not visible, since its location is covered by the aorta and pulmonary trunk. Since these openings and valves structurally weaken the atrioventricular septum, the remaining tissue is heavily reinforced with dense connective tissue called the cardiac skeleton, or skeleton of the heart. It includes four rings that surround the openings between the atria and ventricles, and the openings to the pulmonary trunk and aorta, and serve as the point of attachment for the heart valves. The cardiac skeleton also provides an important boundary in the heart electrical conduction system. The presence of the pulmonary trunk and aorta covers the interatrial septum, and the atrioventricular septum is cut away to show the atrioventricular valves. Patent foramen ovale is normally detected by auscultation of a heart murmur (an abnormal heart sound) and confirmed by imaging with an echocardiogram. Despite its prevalence in the general population, the causes of patent ovale are unknown, and there are no known risk factors. In nonlife-threatening cases, it is better to monitor the condition than to risk heart surgery to repair and seal the opening. If severe, this condition drastically restricts blood flow through the primary systemic artery, which is life threatening. In some individuals, the condition may be fairly benign and not detected until later in life. Detectable symptoms in an infant include difficulty breathing, poor appetite, trouble feeding, or failure to thrive. In older individuals, symptoms include dizziness, fainting, shortness of breath, chest pain, fatigue, headache, and nosebleeds. Treatment involves surgery to resect (remove) the affected region or angioplasty to open the abnormally narrow passageway. Studies have shown that the earlier the surgery is performed, the better the chance of survival. A patent ductus arteriosus is a congenital condition in which the ductus arteriosus fails to close. This additional fluid moving toward the lungs increases pulmonary pressure and makes respiration difficult. Symptoms include shortness of breath (dyspnea), tachycardia, enlarged heart, a widened pulse pressure, and poor weight gain in infants. Treatments include surgical closure (ligation), manual closure using platinum coils or specialized mesh inserted via the femoral artery or vein, or nonsteroidal antiinflammatory drugs to block the synthesis of prostaglandin E2, which maintains the vessel in an open position. Septal defects are not uncommon in individuals and may be congenital or caused by various disease processes. Tetralogy of Fallot is a congenital condition that may also occur from exposure to unknown environmental factors; it occurs when there is an opening in the interventricular septum caused by blockage of the pulmonary trunk, normally at the pulmonary semilunar valve. The term "tetralogy" is derived from the four components of the condition, although only three may be present in an individual patient: pulmonary infundibular stenosis (rigidity of the pulmonary valve), overriding aorta (the aorta is shifted above both ventricles), ventricular septal defect (opening), and right ventricular hypertrophy (enlargement of the right ventricle). Other heart defects may also accompany this condition, which is typically confirmed by echocardiography imaging. Normal treatment involves extensive surgical repair, including the use of stents to redirect blood flow and replacement of valves and patches to repair the septal defect, but the condition has a relatively high mortality. Survival rates are currently 75 percent during the first year of life; 60 percent by 4 years of age; 30 percent by 10 years; and 5 percent by 40 years. In the case of severe septal defects, including both tetralogy of Fallot and patent foramen ovale, failure of the heart to develop properly can lead to a condition commonly known as a "blue baby. Septal defects are commonly first detected through auscultation, listening to the chest using a stethoscope. In this case, instead of hearing normal heart sounds attributed to the flow of blood and closing of heart valves, unusual heart sounds may be detected. Right Atrium the right atrium serves as the receiving chamber for blood returning to the heart from the systemic circulation. The two major systemic veins, the superior and inferior venae cavae, and the large coronary vein called the coronary sinus that drains the heart myocardium empty into the right atrium. The superior vena cava drains blood from regions superior to the diaphragm: the head, neck, upper limbs, and the thoracic region. The inferior vena cava drains blood from areas inferior to the diaphragm: the lower limbs and abdominopelvic region of the body. It, too, empties into the posterior portion of the atria, but inferior to the opening of the superior vena cava. Immediately superior and slightly medial to the opening of the inferior vena cava on the posterior surface of the atrium is the opening of the coronary sinus. This thin-walled vessel drains most of the coronary veins that return systemic blood from the heart. The majority of the internal heart structures discussed in this and subsequent sections are illustrated in Figure 19. While the bulk of the internal surface of the right atrium is smooth, the depression of the fossa ovalis is medial, and the anterior surface demonstrates prominent ridges of muscle called the pectinate muscles. The atria receive venous blood on a nearly continuous basis, preventing venous flow from stopping while the ventricles are contracting. While most ventricular filling occurs while the atria are relaxed, they do demonstrate a contractile phase and actively pump blood into the ventricles just prior to ventricular contraction. Right Ventricle the right ventricle receives blood from the right atrium through the tricuspid valve. They are composed of approximately 80 percent collagenous fibers with the remainder consisting of elastic fibers and endothelium. They connect each of the flaps to a papillary muscle that extends from the inferior ventricular surface. When the myocardium of the ventricle contracts, pressure within the ventricular chamber rises. Blood, like any fluid, flows from higher pressure to lower pressure areas, in this case, toward the pulmonary trunk and the atrium. To prevent any potential backflow, the papillary muscles also contract, generating tension on the chordae tendineae. This prevents the flaps of the valves from being forced into the atria and regurgitation of the blood back into the atria during ventricular contraction. In addition to these muscular ridges, a band of cardiac muscle, also covered by endocardium, known as the moderator band (see Figure 19. It arises from the inferior portion of the interventricular septum and crosses the interior space of the right ventricle to connect with the inferior papillary muscle. When the right ventricle contracts, it ejects blood into the pulmonary trunk, which branches into the left and right pulmonary arteries that carry it to each lung. The superior surface of the right ventricle begins to taper as it approaches the pulmonary trunk. At the base of the pulmonary trunk is the pulmonary semilunar valve that prevents backflow from the pulmonary trunk. Left Atrium After exchange of gases in the pulmonary capillaries, blood returns to the left atrium high in oxygen via one of the four pulmonary veins. While the left atrium does not contain pectinate muscles, it does have an auricle that includes these pectinate ridges. Blood flows nearly continuously from the pulmonary veins back into the atrium, which acts as the receiving chamber, and from here through an opening into the left ventricle. This atrial contraction accounts for approximately 20 percent of ventricular filling. Left Ventricle Recall that, although both sides of the heart will pump the same amount of blood, the muscular layer is much thicker in the left ventricle compared to the right (see Figure 19. There are two papillary muscles on the left-the anterior and posterior-as opposed to three on the right. Heart Valve Structure and Function A transverse section through the heart slightly above the level of the atrioventricular septum reveals all four heart valves along the same plane (Figure 19. Between the right atrium and the right ventricle is the right atrioventricular valve, or tricuspid valve. It typically consists of three flaps, or leaflets, made of endocardium reinforced with additional connective tissue. The flaps are connected by chordae tendineae to the papillary muscles, which control the opening and closing of the valves. Emerging from the right ventricle at the base of the pulmonary trunk is the pulmonary semilunar valve, or the pulmonary valve; it is also known as the pulmonic valve or the right semilunar valve. The pulmonary valve is comprised of three small flaps of endothelium reinforced with connective tissue. When the ventricle relaxes, the pressure differential causes blood to flow back into the ventricle from the pulmonary trunk. This flow of blood fills the pocket-like flaps of the pulmonary valve, causing the valve to close and producing an audible sound. Unlike the atrioventricular valves, there are no papillary muscles or chordae tendineae associated with the pulmonary valve. Located at the opening between the left atrium and left ventricle is the mitral valve, also called the bicuspid valve or the left atrioventricular valve. Structurally, this valve consists of two cusps, known as the anterior medial cusp and the posterior medial cusp, compared to the three cusps of the tricuspid valve. In a clinical setting, the valve is referred to as the mitral valve, rather than the bicuspid valve.
Thus zyrtec menstrual cycle buy cheap serophene 25mg, the race into the uterine tubes pregnancy videos giving birth purchase 50 mg serophene with mastercard, which is the most typical site for sperm to encounter the oocyte women's health center lebanon tennessee cheap 25mg serophene otc, is reduced to a few thousand contenders women's health clinic uw 100mg serophene. Their journey-thought to be facilitated by uterine contractions-usually takes from 30 minutes to 2 hours menopause 53 years old serophene 25 mg without a prescription. Thus women's health clinic east london generic 50 mg serophene with mastercard, fertilization can still occur if intercourse takes place a few days before ovulation. In comparison, an oocyte can survive independently for only approximately 24 hours following ovulation. Intercourse more than a day after ovulation will therefore usually not result in fertilization. During the journey, fluids in the female reproductive tract prepare the sperm for fertilization through a process called capacitation, or priming. Sperm must undergo the process of capacitation in order to have the "capacity" to fertilize an oocyte. Contact Between Sperm and Oocyte Upon ovulation, the oocyte released by the ovary is swept into-and along-the uterine tube. Fertilization must occur in the distal uterine tube because an unfertilized oocyte cannot survive the 72-hour journey to the uterus. As you will recall from your study of the oogenesis, this oocyte (specifically a secondary oocyte) is surrounded by two protective layers. The corona radiata is an outer layer of follicular (granulosa) cells that form around a developing oocyte in the ovary and remain with it upon ovulation. As it is swept along the distal uterine tube, the oocyte encounters the surviving capacitated sperm, which stream toward it in response to chemical attractants released by the cells of the corona radiata. Then, upon contact with the zona pellucida, the sperm bind to receptors in the zona pellucida. This initiates a process called the acrosomal reaction in which the enzyme-filled "cap" of the sperm, called the acrosome, releases its stored digestive enzymes. These enzymes clear a path through the zona pellucida that allows sperm to reach the oocyte. Some sperm undergo a spontaneous acrosomal reaction, which is an acrosomal reaction not triggered by contact with the zona pellucida. The digestive enzymes released by this reaction digest the extracellular matrix of the corona radiata. As you can see, the first sperm to reach the oocyte is never the one to fertilize it. Rather, hundreds of sperm cells must undergo the acrosomal reaction, each helping to degrade the corona radiata and zona pellucida until a path is created to allow one sperm to contact and fuse with the plasma membrane of the oocyte. If you consider the loss of millions of sperm between entry into the vagina and degradation of the zona pellucida, you can understand why a low sperm count can cause male infertility. When the first sperm fuses with the oocyte, the oocyte deploys two mechanisms to prevent polyspermy, which is penetration by more than one sperm. This is critical because if more than one sperm were to fertilize the oocyte, the resulting zygote would be a triploid organism with three sets of chromosomes. The first mechanism is the fast block, which involves a near instantaneous change in sodium ion permeability upon binding of the first sperm, depolarizing the oocyte plasma membrane and preventing the fusion of additional sperm cells. The fast block sets in almost immediately and lasts for about a minute, during which time an influx of calcium ions following sperm penetration triggers the second mechanism, the slow block. In this process, referred to as the cortical reaction, cortical granules sitting immediately below the oocyte plasma membrane fuse with the membrane and release zonal inhibiting proteins and mucopolysaccharides into the space between the plasma membrane and the zona pellucida. The mucopolysaccharides then coat the nascent zygote in an impenetrable barrier that, together with hardened zona pellucida, is called a fertilization membrane. The unneeded complement of genetic material that results is stored in a second polar body that is eventually ejected. The two haploid nuclei derived from the sperm and oocyte and contained within the egg are referred to as pronuclei. The pronuclei then migrate toward each other, their nuclear envelopes disintegrate, and the male- and femalederived genetic material intermingles. This step completes the process of fertilization and results in a single-celled diploid zygote with all the genetic instructions it needs to develop into a human. However, in approximately 1 percent of ovulation cycles, two eggs are released and both are fertilized. Two zygotes form, implant, and develop, resulting in the birth of dizygotic (or fraternal) twins. Because dizygotic twins develop from two eggs fertilized by two sperm, they are no more identical than siblings born at different times. Much less commonly, a zygote can divide into two separate offspring during early development. These two scenarios are distinct from each other, in that the twin embryos that separated at the two-cell stage will have individual placentas, whereas twin embryos that form from separation at the blastocyst stage will share a placenta and a chorionic cavity. In vitro, which in Latin translates to "in glass," refers to a procedure that takes place outside of the body. For example, a woman may produce normal eggs, but the eggs cannot reach the uterus because the uterine tubes are blocked or otherwise compromised. A man may have a low sperm count, low sperm motility, sperm with an unusually high percentage of morphological abnormalities, or sperm that are incapable of penetrating the zona pellucida of an egg. Right before the ova would be released from the ovary, they are harvested using ultrasound-guided oocyte retrieval. The sperm sample is also concentrated, to increase the sperm count per milliliter. If there are severe problems with the sperm-for example, the count is exceedingly low, or the sperm are completely nonmotile, or incapable of binding to or penetrating the zona pellucida-a sperm can be injected into an egg. The embryos are then incubated until they either reach the eight-cell stage or the blastocyst stage. In the United States, fertilized eggs are typically cultured to the blastocyst stage because this results in a higher pregnancy rate. The period of time required for full development of a fetus in utero is referred to as gestation (gestare = "to carry" or "to bear"). The first 2 weeks of prenatal development are referred to as the pre-embryonic stage. By the end of the embryonic period, all of the organ systems are structured in rudimentary form, although the organs themselves are either nonfunctional or only semifunctional. Pre-implantation Embryonic Development Following fertilization, the zygote and its associated membranes, together referred to as the conceptus, continue to be projected toward the uterus by peristalsis and beating cilia. During its journey to the uterus, the zygote undergoes five or six rapid mitotic cell divisions. Although each cleavage results in more cells, it does not increase the total volume of the conceptus (Figure 28. Each daughter cell produced by cleavage is called a blastomere (blastos = "germ," in the sense of a seed or sprout). The cells that had been loosely grouped are now compacted and look more like a solid mass. It continues to divide, creating a ball of approximately 100 cells, and consuming nutritive endometrial secretions called uterine milk while the uterine lining thickens. The ball of now tightly bound cells starts to secrete fluid and organize themselves around a fluid-filled cavity, the blastocoel. Within this structure, a group of cells forms into an inner cell mass, which is fated to become the embryo. The cells that form the outer shell are called trophoblasts (trophe = "to feed" or "to nourish"). These cells will develop into the chorionic sac and the fetal portion of the placenta (the organ of nutrient, waste, and gas exchange between mother and the developing offspring). The inner mass of embryonic cells is totipotent during this stage, meaning that each cell has the potential to differentiate into any cell type in the human body. As the blastocyst forms, the trophoblast excretes enzymes that begin to degrade the zona pellucida. In a process called "hatching," the conceptus breaks free of the zona pellucida in preparation for implantation. Implantation At the end of the first week, the blastocyst comes in contact with the uterine wall and adheres to it, embedding itself in the uterine lining via the trophoblast cells. Thus begins the process of implantation, which signals the end of the pre-embryonic stage of development (Figure 28. The blastocyst typically implants in the fundus of the uterus or on the posterior wall. However, if the endometrium is not fully developed and ready to receive the blastocyst, the blastocyst will detach and find a better spot. The high rate of implantation failure is one reason why pregnancy typically requires several ovulation cycles to achieve. When implantation succeeds and the blastocyst adheres to the endometrium, the superficial cells of the trophoblast fuse with each other, forming the syncytiotrophoblast, a multinucleated body that digests endometrial cells to firmly secure the blastocyst to the uterine wall. In response, the uterine mucosa rebuilds itself and envelops the blastocyst (Figure 28. Most of the time an embryo implants within the body of the uterus in a location that can support growth and development. However, in one to two percent of cases, the embryo implants either outside the uterus (an ectopic pregnancy) or in a region of uterus that can create complications for the pregnancy. If the embryo implants in the inferior portion of the uterus, the placenta can potentially grow over the opening of the cervix, a condition call placenta previa. However, there are also ovarian ectopic pregnancies (in which the egg never left the ovary) and abdominal ectopic pregnancies (in which an egg was "lost" to the abdominal cavity during the transfer from ovary to uterine tube, or in which an embryo from a tubal pregnancy re-implanted in the abdomen). Tubal pregnancies can be caused by scar tissue within the tube following a sexually transmitted bacterial infection. The scar tissue impedes the progress of the embryo into the uterus-in some cases "snagging" the embryo and, in other cases, blocking the tube completely. Implantation in a uterine tube causes bleeding, which appears to stimulate smooth muscle contractions and expulsion of the embryo. If diagnosis is late and the uterine tube is already ruptured, surgical repair is essential. Even if the embryo has successfully found its way to the uterus, it does not always implant in an optimal location (the fundus or the posterior wall of the uterus). Placenta previa can result if an embryo implants close to the internal os of the uterus (the internal opening of the cervix). As the fetus grows, the placenta can partially or completely cover the opening of the cervix (Figure 28. Embryonic Membranes During the second week of development, with the embryo implanted in the uterus, cells within the blastocyst start to organize into layers. Some grow to form the extra-embryonic membranes needed to support and protect the growing embryo: the amnion, the yolk sac, the allantois, and the chorion. At the beginning of the second week, the cells of the inner cell mass form into a two-layered disc of embryonic cells, and a space-the amniotic cavity-opens up between it and the trophoblast (Figure 28. Cells from the upper layer of the disc (the epiblast) extend around the amniotic cavity, creating a membranous sac that forms into the amnion by the end of the second week. Early in development, amniotic fluid consists almost entirely of a filtrate of maternal plasma, but as the kidneys of the fetus begin to function at approximately the eighth week, they add urine to the volume of amniotic fluid. Floating within the amniotic fluid, the embryo-and later, the fetus-is protected from trauma and rapid temperature changes. It can move freely within the fluid and can prepare for swallowing and breathing out of the uterus. On the ventral side of the embryonic disc, opposite the amnion, cells in the lower layer of the embryonic disk (the hypoblast) extend into the blastocyst cavity and form a yolk sac. The yolk sac supplies some nutrients absorbed from the trophoblast and also provides primitive blood circulation to the developing embryo for the second and third week of development. When the placenta takes over nourishing the embryo at approximately week 4, the yolk sac has been greatly reduced in size and its main function is to serve as the source of blood cells and germ cells (cells that will give rise to gametes). During week 3, a finger-like outpocketing of the yolk sac develops into the allantois, a primitive excretory duct of the embryo that will become part of the urinary bladder. Together, the stalks of the yolk sac and allantois establish the outer structure of the umbilical cord. The last of the extra-embryonic membranes is the chorion, which is the one membrane that surrounds all others. The development of the chorion will be discussed in more detail shortly, as it relates to the growth and development of the placenta. Embryogenesis As the third week of development begins, the two-layered disc of cells becomes a three-layered disc through the process of gastrulation, during which the cells transition from totipotency to multipotency. The embryo, which takes the shape of an oval-shaped disc, forms an indentation called the primitive streak along the dorsal surface of the epiblast. A node at the caudal or "tail" end of the primitive streak emits growth factors that direct cells to multiply and migrate. Cells migrate toward and through the primitive streak and then move laterally to create two new layers of cells.
Order 50mg serophene free shipping. Essential womens health advice.
References