


|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Michael Maresh MD, FRCOG
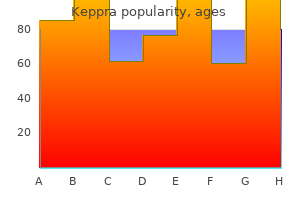
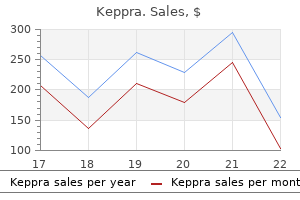
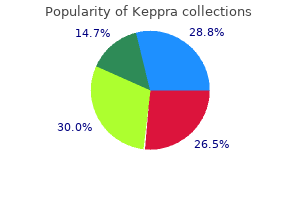
The finding of a statistically significant increase in symptoms with the lactose containing product versus the low lactase product was considered to provide evidence of intolerance 94 medications that can cause glaucoma keppra 250mg overnight delivery. However medications janumet purchase keppra 500mg free shipping, the biological significance of changes in numerical rating seldom was investigated medicine 44291 keppra 500mg free shipping. Only one study attempted to evaluate the association between the symptom score and the global assessment of symptom severity symptoms zinc deficiency order keppra 500mg amex. In this study symptoms chlamydia discount 250mg keppra visa, the majority of a group of subjects who had a significant increase in symptom score when high and low lactose test periods were compared did not clearly identify the high lactose period as being particularly symptomatic medicine hollywood undead order keppra 250mg mastercard. Some data supports the belief that the routine ingestion of lactose increases the quantity of lactose that is tolerable. Very few studies provided data on lactose ingestion by subjects prior to enrollment in controlled trials. In contrast, when lactose/milk is administered as a single test dose without other nutrients, dosages of 12 grams may be symptomatic (Figure 13). As the dose is increased above 12 grams, intolerance becomes more prominent, with single doses of 24 grams usually yielding appreciable symptoms. While the literature is laden with studies of the relationship of ethnicity to lactose malabsorption, no studies made it possible to determine if lactose malabsorbers of differing ethnicities have differing tolerance to lactose. Symptomatic response# of adult lactose malabsorbers to lactose ingested with nutrients other than milk Publication 128 Cheng, 1979 (n=15)* Suarez, 1998110 (n=31) Vesa, 1997132 (n=30) 130 Jones, 1976 (n=16) Rorick, 1979116 (n=23) Suarez, 1997111 (n=19) 113 Suarez, 1995 (n=21) Newcomer, 1978120 (n=59) 118 Hertzler, 1996 (n=18) Daily lactose (grams) # ++ + 0 3 6 7 9 12 15 18 22 30 34 42 49 ++ 50 55 63 70 ++ Symptoms indicated by: - no or trivial symptoms; + minor symptoms; ++ severe symptoms * n indicates number of lactose malabsorbing subjects studied # Figure 13. The details of our search strategy are presented in the methods section and in Figure 2. A total of 37 unique randomized studies (26 on lactase/lactose hydrolyzed milk supplements, lactose reduced milk, eight on probiotics, two on incremental lactose dose for colonic adaptation, and one on other agents) met inclusion criteria. Generally, studies had small sample sizes and reporting of symptoms was variable or not reported: composite scores of four to five symptoms or individual symptoms such as abdominal pain, diarrhea, bloating, and flatulence were reported, either as means or proportion. There was one study representing two trials that tested lactase supplements Lactodigest, DairyEase, and Lactaid,136 while the remaining 25 studies reported on lactose reduced or hydrolyzed milk by adding a lactase enzyme such as betagalactosidase to the milk. The mean age of subjects was 37 years of age, with a range between 10 and 77 (n=19 studies). When compared to controls given greater than 12 grams of lactose, only two out of five trials reported statistically significant reductions in overall symptoms with lactose reduced/ hydrolyzed milk. Some studies did report substantial reductions (improvement from moderate and severe to mild or none, or an absolute reduction of at least 50 percent) in abdominal pain/cramping109,112,123,125,134 and diarrhea136 with use of lactose reduced solution/milk, with lactose content of 0-2 grams, compared to a lactose dose of 12 grams or more. However, even in studies where symptoms were reduced, statistically significant reductions were not consistently observed among all symptoms reported, or only a subset of symptoms was reported. For example, the overall symptom score was significantly reduced by 60 percent with 591 milliliters of lactose reduced milk containing 7. One study showed a statistically significant reduction in abdominal pain from moderate to none or mild with low lactose milk containing 2. Eight randomized trials were included; (Appendix Table D9) seven crossover117,139-141,143-145 and one parallel group design. White subjects comprised two trials,140,141 one study evaluated black African immigrants to France,142 and one trial was conducted in Taiwan Chinese. We found insufficient evidence to determine the effectiveness of yogurt or probiotics to improve lactose intolerance symptoms (Table 19). The inclusion criteria and the studied type of yogurt and probiotics were variable-results either did not show a difference in symptom score, or reported clinically insignificant differences, mostly in the symptoms that are of low clinical relevance, such as flatulence. Only one study noted that the enrolled subjects reported symptoms compatible with malabsorption of lactose prior to study entry144 and reported no difference in symptom score in groups given milk or acidophilus milk (symptom score of 40 in both groups). In the remaining studies, study entry was based solely on breath hydrogen tests, and subjects were not reported to experience symptoms following ingestion of lactose. Overall symptom scores improved from fairly strong to mild with 400 ml of bulgofilus milk (Ofilus bacteria+L. The inclusion criteria were variable, the type, source, and concentration of yogurt and probiotics studied were variable, and no two studies studied the same agent. Based on these findings we found insufficient evidence for the use of yogurt or probiotics for lactose intolerance. Incremental Lactose for Colonic Adaptation We found insufficient evidence to support the role of incremental doses of lactose for lactose intolerance symptoms (Table 19). The authors found that symptoms of flatulence after the lactose challenge decreased by 50 percent after lactose feeding compared to dextrose feeding, while symptoms of abdominal pain and diarrhea did not differ. These results suggest that colonic adaptation may occur, but there is no appreciable decrease in clinically relevant symptoms of abdominal pain and diarrhea. Though subjects were lactose malabsorbers at baseline, average symptom scores were 1 (scale 0-5) even with the highest doses of lactose (70 grams), and very similar to scores were seen with sucrose. The second study evaluated colonic adaptation to lactose compared to sucrose in a double blinded fashion. The study enrolled 46 healthy volunteers in France, 21 males, 25 females, all of Asian origin, with a mean age of 33 (range 20-47 years) that were lactose malabsorbing by hydrogen breath testing. Subjects were fed their regular diet and underwent hydrogen breath testing and symptom evaluation on days 1 and 14. For the 13 days in between, subjects were fed either 34grams of lactose or sucrose in a double blind fashion. The overall clinical score improved from 42 to 20 in the group randomized to lactose, as did the individual mean scores for pain, flatulence, bloating and borborygmi, but similar improvements were seen with sucrose (overall score improvement from 42 to 24), suggesting a placebo response. Other Strategies We found insufficient evidence regarding rifaximin for treatment of lactose intolerance. A single small study met inclusion criteria147 and showed reduction in symptom score after rifaximin treatment compared to placebo and similar to a lactose free control. The study enrolled 40 patients with lactose malabsorption on hydrogen breath test, 16 were randomized to 10-day treatment with rifaximin 800 mg/day, 16 to a 40-day lactose free diet, while eight were given 10 days of placebo. Within the lactase deficient group, symptoms were not significantly reduced during the acidophilus milk period compared to the regular milk period. Percentage of subjects reporting abdominal pain = 15) Che n (n (n= 11) Ra sk-P = 30) V esa (n = 30) Vesa (n (n= 24) Unge r 27) e n (n= Ja rvin 27) e n (n= Ja rvin (n= 6) Bra nd (n= 6) Bra nd (n= 11) Ra sk-P = 39) Vesa (n (n= 6) Bra nd (n= 6) Bra nd (n= 6) Bra nd n= 24) (Unge r V esa (n V esa (n Vesa (n e Ja rvin = 39) = 39) = 39) 7) n (n=2 e Ja rvin 7 n (n=2 Che n (n Vesa (n = 15) = 30) 90 80 70 60 50 40 30 20 100 10 0 123 Figure 15. Prebiotic/probiotic studies Total number of studies 9 to 28 8 Studies with lactose tolerant controls (number of controls) 10 1 Studies in which subjects were not noted to be symptomatic at 9 to 28 7 baseline or symptoms were not required for study inclusion Age range of subjects 18 to 69 7 Gender, female - mean % (range) 34 (0 to 73) 5 (2 exclusively male) Race/ethnicity, White - mean % (range) 45 (0 to 100) 4 (2 exclusive) Race/ethnicity, black - mean % (range) 24 (0 to 100) 4 (1 exclusive) Race/ethnicity, Asian - mean % (range) 30 (0 to 100) 4 (1 exclusive) Number of studies conducted in the United States 9 to 28 5 Diagnosis, hydrogen breath test All studies Noted as "double blind" studies (some studies noted that it may not be 5 studies possible to mask flavors of tests) Single blind or blinding unclear studies 3 studies D and E. Colonic adaptation and incremental lactose load studies/studies with different levels of lactose Total number of studies 13 to 59 4 Studies with lactose tolerant controls (number of controls) 19 1 Studies in which subjects were not noted to be symptomatic at All studies baseline or symptoms were not required for study inclusion Age range of subjects 23 (19 to 32) 3 Gender, female - mean % (range) 46 (25 to 54) 4 Race/ethnicity, Non-white - mean % (range) 51 (29 to 90) 2 Asian 70% in one trial Race/ethnicity, White - mean % (range) 49 (10 to 71) 2 American Indian 59 (1 exclusive) Number of studies conducted in the United States All studies Diagnosis, hydrogen breath test 3 studies Diagnosis, blood sugar test 1 study Noted as "double blind" studies (some studies noted that it may not be 2 studies possible to mask flavors of tests) Single blind or blinding unclear studies 2 studies Characteristic *Subjects could be of any race 125 Table 19. Commercially-available lactase/lactose hydrolyzed milk, or nonlactose solutions A1. At 10 times during the 24 test periods, a 0 was recorded in the scoring chart to indicate no symptoms and a 1 was recorded if symptoms were observed. Studies with doses of lactose 12 g per dose/test 109 Severity of each symptom was graded from 0=none to 4=severe. Symptom score represents the sum of symptoms, based on 0=none to 40=all, very severe (data were extracted from graph). The total symptom score was calculated as (n=35) the sum of the score for each person. On a 24 hour diary sheet, subjects reported abdominal symptoms based on Rask Pedersen, 1982 the following, 0=none; 1=mild/moderate; 2=severe. For diarrhea, no diarrhea=formed stools; mild/moderate= (n=11) 3 liquid/soft stools; severe= 4 liquid/soft stools. Studies in which subjects were not noted to be symptomatic at baseline or symptoms were not required for study inclusion (based on biochemical measures only) Number of Lactose Overall Abdominal Abdominal Borborygmi Subjects Study (n) / Interventions Content/ Symptom Flatulence Diarrhea Reporting Pain/Cramps Bloating (or other) Day Score Symptoms Lin, Study 1, 1993136 Symptom scores, expressed as the mean of the sum of scores rating symptoms (gas, stomach pain and/or cramps and diarrhea) from 0 (none) to 5 (severe) for each hour from baseline to 8 hr after the challenge. A numerical score was given for the presence or absence of 4 symptoms (abdominal cramps, gas/flatulence, vomiting, and/or diarrhea), 0=absent to 3=severe, except for diarrhea which was always marked a 3. Frequency of symptoms is based on only the subjects who reported symptoms, 7 in the malabsorber group, 18 in the absorber group and subjects could be intolerant to both test drinks. Symptoms were scored as severe if diarrhea was present or if a cumulative rating of other symptoms (abdominal cramps, bloating, flatulence) was 4+. Subjects were not specifically asked if they developed any symptoms commonly associated with lactose intolerance. Studies that reported subjects with symptoms at baseline in addition to lactose intolerance by testing Number of Lactose Overall Subjects Abdominal Abdominal Borborygmi Content/ Symptom Study (n) / Interventions Flatulence Diarrhea Pain/Cramps Bloating (or other) Reporting Day Score Symptoms Newcomer, 1983144 Mean symptom score over 10wk for diarrhea + pain + gas + borborygmi, averaged and compared to control. Studies in which subjects were not noted to be symptomatic at baseline or symptoms were not required for study inclusion (based on biochemical measures only) Number of Lactose Overall Study (n) / Subjects Abdominal Abdominal Borborygmi Content/ Symptom Flatulence Diarrhea Interventions Pain/Cramps Bloating (or other) Reporting Day Score Symptoms Lin, 1998117 Mean symptom score over 8 hours, 0-5 from none to severe for abdominal pain, gas and diarrhea averaged and compared to control. Other therapies Study (n) / Interventions Cappello 2005147 Rifaximin x 10 days (n=14) Lactose Content/ Day Number of Abdominal Abdominal Borborygmi Subjects Flatulence Diarrhea Reporting Pain/Cramps Bloating (or other) Symptoms Symptoms score referred to the 5 days preceding each evaluation and scored as: 0=absent; 1=mild (awareness of a symptom but easily tolerated); 2=moderate; 3=severe; and 4=very severe at baseline (b), 10 and 40 days (d). Lactose 17 g plus 50 g aspartame (to mask taste) twice daily (34 g lactose total) over 13 days (days 2 to 14). Every hour, subjects reported any occurrence of abdominal pain, borborygmus, flatulence, and abdominal distension, and graded each symptom5 as absent = 0, mild = 1, moderate = 2, or severe = 3. The total clinical score was calculated for each subject by summing the scores for each symptom (range 0 to 144). A subject was considered to have a positive symptomatic response if he/she had 1 loose stools or had a grade 2+ or higher in at least one of the following symptoms: abdominal cramps/pain, bloating or gas, borborygmi, flatulence. Each symptom, except urgency, was scored from 0 to 4, with 0 being no symptoms and 4 being most severe. Overall Symptom Score During the double blind, placebo controlled challenges, two of the seven (29%) showed worsening symptoms with higher levels of lactose. Subjects scored symptoms (pain, flatulence, distension, diarrhea, mucus, incomplete evacuation) from 0=no complaints, 1=mild; 2=moderate; and 3 as severe. Symptoms included constipation, diarrhea, abdominal pain, (n=12, 8 were lactose nonpersistent based on abdominal distension, and flatulence. Scored as following: 0=no trouble; 1=slight trouble; 2=mild; 3=moderate; 4=severe. Discussion Summary and Discussion Our evidence synthesis has the following major conclusions: (1) Reliable estimates of U. There was also insufficient evidence on the effects of other treatment options, including probiotics and incremental lactose loads. Data available tended to be from highly selected populations and not likely representative of the overall U. Racial and ethnic variation was clearly present, but the variation in symptoms reported following a challenge does not seem as extreme as the racial and ethnic variation seen in lactose malabsorption and prevalence of hypolactasia. Dietary lactose intake and supplemental calcium consumption were recorded in a few observational studies. We found inconsistent increased risk of bone fracture in populations with documented or assumed low lactose intake. Poor documentation of dietary intake may contribute to inconsistency in results of observational studies. A recently published systematic review of the association between vitamin D and dietary calcium also found that inconsistent dietary analysis hampered synthesis of evidence. Because the major Appendixes and evidence tables cited in this report are available at. We found that dairy interventions in healthy children with low baseline milk intake may result in short but not longterm improvement of bone mineral content and density. Adults with lactose free or low lactose diet may have increased risk of bone fractures. Low and inconsistent evidence suggested that adults with milk intolerance and malabsorption had greater odds of fractures and worse bone outcomes. Children with low baseline calcium consumption may benefit from increased lactose intake. However, as the dose is increased above 12 grams, these individuals can be informed that intolerance becomes more prominent, with single doses of 24 grams usually yielding appreciable symptoms. There is some evidence that if 24 grams of lactose is distributed throughout the day, many lactose malabsorbers will tolerate this dosage. No studies assessed if lactose malabsorbers of differing ethnicities have differing tolerance to lactose. Advice regarding additional management strategies is hampered from the lack of study uniformity in design and methodology. However, we caution that the criterion of being symptomatic at baseline was found only in a few studies, and not all of the enrolled subjects may have actually been lactose intolerant. Most studies had an 8-hour recording period, and it is difficult to generalize these findings to individuals with chronic relapsing remitting problems with a constellation of symptoms. Individuals can be informed that while some studies indicated that treatments provided a statistical benefit, symptomatic improvement generally went from none to mild or slight, and the clinical significance for many individuals may be low. There is little information on the effect of these interventions on diarrhea and abdominal pain. Key Question 1 In order to accurately assess the population prevalence of lactose, future studies will need to be derived from population based samples that include adequate distributions across ages and ethnic variation in order to map the effects of these important factors. Effort will also need to be made to account for possible placebo effects in reporting symptoms. The best mechanisms available for accounting for placebo effects would be to conduct blinded challenges with and without lactose and to assign the difference in reported symptoms and the true prevalence due to the lactose challenge.
Pathogenesis Rickettsiae are inoculated by the tick after 6 h of feeding symptoms uterine prolapse buy keppra 500 mg cheap, spread lymphohematogenously medicine ball workouts buy generic keppra 250mg on line, and infect numerous foci of contiguous infected endothelial cells treatment jammed finger buy 250mg keppra with visa. Increased vascular permeability medications 512 generic 500mg keppra overnight delivery, with edema medications prescribed for ptsd generic keppra 500 mg mastercard, hypovolemia medicine advertisements discount keppra 250mg fast delivery, and ischemia, causes tissue and organ injury. Symptoms in the first 3 days of illness are nonspecific and include fever, headache, malaise, myalgias, nausea, vomiting, and anorexia. Macules typically appear on the wrists and ankles, subsequently spreading to the rest of the extremities and the trunk. Lesions initially blanch; however, because of vascular damage, central hemorrhage later develops and the lesions become petechial. Pts develop hypovolemia, prerenal azotemia, hypotension, noncardiogenic pulmonary edema, and cardiac involvement with dysrhythmias. Pulmonary disease is an important factor in fatal cases and develops in 17% of cases overall. Meningoencephalitis can develop, with cerebrospinal fluid notable for pleocytosis, mononuclear cell predominance, and increased protein and normal glucose levels. Renal and hepatic injury can occur, and bleeding is a rare but potentially life-threatening consequence of severe vascular damage. Other laboratory findings may include increased plasma levels of acute-phase reactants such as C-reactive protein, hyponatremia, and elevated levels of creatine kinase. Immunohistologic examination of a cutaneous biopsy sample from a rash lesion is the only diagnostic test of use during acute illness. Disease is characterized by high fever, rash, and-in most locales-an inoculation eschar (tache noire) at the site of the tick bite. A severe form of disease with ~50% mortality occurs in pts with diabetes, alcoholism, or heart failure. Recognized principally in New York City, rickettsialpox has been reported in other urban and rural locations in the United States as well as in Ukraine, Croatia, and Turkey. Some pts have nausea, vomiting, abdominal pain, cough, conjunctivitis, or photophobia. Humans become infected when rickettsia-laden flea feces are scratched into pruritic bite lesions; less often, the flea bite itself transmits the organisms. In the United States, endemic typhus occurs mainly in southern Texas and southern California; globally, it occurs in warm (often coastal) areas throughout the tropics and subtropics. Flea bites are not often recalled by pts, but exposure to animals such as cats, opossums, raccoons, skunks, and rats is reported by ~40%. Rash is apparent at presentation (usually ~4 days after symptom onset) in 13% of pts; 2 days later, half of the remaining pts develop a maculopapular rash that involves the trunk more than the extremities, is seldom petechial, and rarely involves the face, palms, or soles. Disease can be severe enough for admission to an intensive care unit, and complications include respiratory failure requiring intubation and mechanical ventilation, hematemesis, cerebral hemorrhage, and hemolysis. Lice feed on pts with epidemic typhus and then defecate the organism into the bite at their next meal. Brill-Zinsser disease is a recrudescent and mild form of epidemic typhus whose occurrence years after acute illness suggests that R. Confusion and coma, skin necrosis, and gangrene of the digits are noted in severe cases. Diagnosis the diagnosis can be based on serology or immunohistochemistry or on detection of the organism in a louse found on a pt. Pts have an eschar at the site of chigger feeding, regional lymphadenopathy, and maculopapular rash. After a median incubation period of 8 days, pts develop fever, headache, myalgia, and malaise. Most cases of human anaplasmosis occur in northeastern and upper midwestern states. Co-infection with either Borrelia burgdorferi (the agent of Lyme disease) or Babesia microti should be considered in all cases because these three agents share the Ixodes scapularis vector and have the same geographic distribution. The primary sources of human infection are infected cattle, sheep, and goats, but cats, rabbits, pigeons, and dogs can transmit the disease as well. At parturition, the organism is dispersed as an aerosol, and infection usually follows inhalation. Abattoir workers, veterinarians, and others persons who have contact with infected animals are at risk. Ingestion of contaminated milk is believed to be an important route of transmission in some areas, although the evidence on this point is contradictory. Clinical presentations include flulike syndromes, prolonged fever, pneumonia, hepatitis, pericarditis, myocarditis, meningoencephalitis, and infection during pregnancy. Pts with acute Q fever and lesions of native or prosthetic heart valves should be monitored serologically for 2 years. Some authorities treat pts with acute Q fever and valvulopathy for 1 year with doxycycline and hydroxychloroquine to prevent chronic Q fever. Hepatomegaly and/or splenomegaly in combination with a positive rheumatoid factor, high erythrocyte sedimentation rate, high C-reactive protein level, and/or increased -globulin concentration suggests the diagnosis. The currently recommended treatment for chronic Q fever is doxycycline (100 mg bid) and hydroxychloroquine (200 mg tid; plasma concentrations maintained at 0. Pts should be advised about photosensitivity and retinal toxicity risks with treatment. Pts who cannot receive this regimen should be treated with at least two agents active against C. Treatment should be given for at least 3 years and discontinued only if phase I IgA and IgG antibody titers are 1:50 and 1:200, respectively. Children <5 years old usually have only upper respiratory tract disease; children >5 years old and adults usually have bronchitis and pneumonia. Infection can be severe in pts with sickle cell disease as a result of functional asplenia. Pts often have antecedent upper respiratory tract symptoms and then develop fever, sore throat, and prominent headache and cough. Diagnosis Chest x-ray may show reticulonodular or interstitial infiltrates, primarily in the lower lobes. The elementary body (the infective form) is adapted for extracellular survival, while the reticulate body is adapted for intracellular survival and multiplication. After replication, reticulate bodies condense into elementary bodies that are released to infect other cells or people. Epidemiology Trachoma causes ~20 million cases of blindness worldwide, primarily in northern and sub-Saharan Africa, the Middle East, and parts of Asia. With progression, there is inflammatory leukocytic infiltration and superficial vascularization (pannus formation) of the cornea. Eventually, the corneal epithelium ulcerates, with subsequent scarring and blindness. Diagnosis Clinical diagnosis is based on the presence of two of the following signs: lymphoid follicles on the upper tarsal conjunctiva, typical conjunctival scarring, vascular pannus, or limbal follicles. Chlamydial polymerase chain reaction or ligase chain reaction is more sensitive and often gives positive results when smears or cultures are negative. Psittacosis is an occupational disease in pet-shop owners, poultry workers, and other individuals with regular avian contact. The pathognomonic histologic finding is the presence of macrophages with typical cytoplasmic inclusion bodies in alveoli filled with fluid, erythrocytes, and lymphocytes. Physical findings are less prominent than symptoms and x-ray findings would suggest. Diagnosis this diagnosis should be considered in a pt with pneumonia and splenomegaly and is confirmed by serologic studies. Erythromycin is an alternative agent; azithromycin and some fluoroquinolones are active in vitro and are likely to be effective. Both antibody-mediated and cell-mediated immunity (including type-specific immunity) are clinically important. Pts commonly have gingivostomatitis, pharyngitis, and up to 2 weeks of fever, malaise, myalgia, inability to eat, and cervical adenopathy with lesions on the palate, gingiva, tongue, lip, face, posterior pharynx, and/or tonsillar pillars. Pts undergoing trigeminal nerve root decompression or dental extraction can develop oral-labial herpes a median of 3 days after the procedure. Antiviral treatment should be started empirically until the diagnosis is confirmed or an alternative diagnosis is made. Numbness, tingling of the buttocks or perineal areas, urinary retention, constipation, and impotence can occur. Hypesthesia and/or weakness of the lower extremities may develop and persist for months. Its sensitivity is higher in vesicular rather than ulcerative mucosal lesions, in primary rather than recurrent disease, and in compromised rather than immunocompetent hosts. In bone marrow and renal transplant recipients, oral valacyclovir (2 g/d) is also effective in reducing cytomegalovirus infection. Symptomatic recurrent genital herpes: Short-course (1- to 3-day) regimens are preferred because of low cost and convenience. Oral acyclovir (800 mg tid for 2 days), valacyclovir (500 mg bid for 3 days), or famciclovir (750 or 1000 mg bid for 1 day, a 1500-mg single dose, or 500 mg stat followed by 250 mg q12h for 3 days) effectively shortens lesion duration. Other options include oral acyclovir (200 mg 5 times per day), valacyclovir (500 mg bid), and famciclovir (125 mg bid) for 5 days. Suppression of recurrent genital herpes: Oral acyclovir (200-mg capsules tid or qid, 400 mg bid, or 800 mg qd), famciclovir (250 mg bid), or valacyclovir (500 mg qd) is effective. Pts with >9 episodes per year should take oral valacyclovir at a dosage of 1 g qd or 500 mg bid. First episode: Oral acyclovir (200 mg) is given 4 or 5 times per day; an oral acyclovir suspension can be used (600 mg/m2 qid). Recurrent episodes: If initiated at onset of the prodrome, single-dose or 1-day therapy effectively reduces pain and speeds healing. Regimens include oral famciclovir (a 1500-mg single dose or 750 mg bid for 1 day) or valacyclovir (a 2-g single dose or 2 g bid for 1 day). The optimal duration of therapy and the usefulness of its continuation in suppressing lesions are unclear. Some pts may benefit from cutaneous application of trifluorothymidine or 5% cidofovir gel. With vaccine use, the annualized incidence of chickenpox has decreased significantly. Skin lesions include maculopapules, vesicles, and scabs in various stages of evolution. Acute cerebellar ataxia and meningeal irritation usually appear ~21 days after the onset of rash and run a benign course.
Protect with light medicine 3d printing purchase 250mg keppra free shipping, dry medications during labor order 250mg keppra fast delivery, sterile dressings; cover with warm blankets and prevent re-exposure 3 symptoms quit drinking order keppra 250 mg fast delivery. If unresponsive with no breathing or no normal breathing (only gasping) check for a pulse symptoms ectopic pregnancy buy 250 mg keppra with mastercard. All persons submerged 1 hour should be resuscitated unless there are signs of obvious death treatment xerophthalmia safe 500mg keppra. Cold-induced hypovolemia medicine man gallery 250mg keppra overnight delivery, cold myocardium, and impaired reflexes may result in significant hypotension. If hypothermic, appropriate rewarming should be done concurrent with resuscitation. Consider need for advanced airway if patient does not respond to initial bag and mask ventilations. When hypoglycemia is corrected and confirmed by a repeat bG reading, they can be re-assessed for ability to refuse care. If S&S of hypoglycemia fully reverse and pt becomes decisional after partial dose, reassess bG If >70; clamp off D10% and open 0. If S&S of hypoglycemia fully reverse and pt becomes decisional after a partial dose, reassess bG. If combative and/or uncooperative (See possible medication Rx below): Attempt verbal reassurance to calm pt. Ensure an adequate airway, ventilations, and peripheral perfusion distal to restraint after application. Metabolic disorders: hypoglycemia (glucose), acidosis, electrolyte imbalance, thyroid/liver/renal disease etc. If patient is non-decisional and/or a threat to self or others and/or is unable to care for themselves Complete Petition Form for all adults who meet above criteria: Persons who witnessed statements or behaviors should sign the form. Questions: Age, month (orientation) Commands: Open/close eyes Facial asymmetry/droop: smile, show teeth Vision deficits: loss of visual fields; diplopia Horizontal gaze abnormalities: dysconjugate gaze, forced or crossed gaze Other deficits: pupil changes; light sensitivity, deviated uvula; hoarse voice; vertigo/dizziness, sound sensitivity hold both arms out for 10 sec. Obtain and document history; stroke screen; and other physical exam findings as above 6. Obtain call back number from reliable historian; provide to receiving staff if not accompanying pt. Vomiting/aspiration precautions; suction prn Protect patient from injury; do not restrain during tonic/clonic movements Position on side during postictal phase unless contraindicated 2. Weigh risk of waiting for resources against benefit of rapid transport to definitive care. Re-sequencing priorities if exsanguinating external hemorrhage: C-A-B-C-D-E: Hemorrhage control first. Consider possible spine injury Open/maintain using position, suction, appropriate adjuncts, & manual spine precautions prn Once airway controlled: Apply appropriate size c-collar + selective spine precautions if indicated Vomiting/seizure precautions as indicated 5. If direct pressure ineffective or impractical: - Pack wound w/ topical hemostatic gauze/ apply direct pressure. Uncontrolled bleeding limb: Tourniquet 2-3 cm proximal to wound; not over joint; tighten until bleeding stops/distal pulse occluded. Report pertinent positive/negative signs as able; any major changes from primary assessment 5. Victims of submersion, lightning strike and hypothermia deserve special consideration as they may have an altered prognosis. If patient has not had tetanus immunization in the last 10 yrs, advise to acquire it Provide disclosure of risk and obtain signature on refusal form. Remove clothing, constricting jewelry; belts, suspenders, steel toed shoes (retain heat) Do not pull away clothing stuck to skin (cut around). Circumferential burns to torso/limbs dangerous due to potential vascular and ventilatory compromise; careful ongoing assessments of distal perfusion. Do not break blisters, debride skin, or apply topical ointments, creams, or anti-microbials in the field Wrap digits individually or place gauze between burned skin areas 3. Assess for stridor, wheezing, carbonaceous (black) sputum, cough, hoarseness, singed nasal or facial hair, dyspnea, burns, edema or inflammatory changes in oral pharynx/upper airway 3. Ensure scene safety: do not contact pt until certain electrical source has been disabled/disconnected 3. Describe appearance of wounds (often full thickness); No cooling needed unless an associated thermal burn; Apply dry, sterile dressings. Assess for potential associated trauma from being thrown from contact point; note neurovascular function all limbs. Avoid self-injury; haz-mat precautions; decon per procedure; remove contaminated clothing. Burned children in hospitals w/o qualified personnel or equipment to care for them. Burn injury in pts who will require special social, emotional, or rehabilitative intervention. Needle pleural decompression on affected side while on scene (takes priority over airway). Monitor for tension pneumothorax; prepare to perform needle pleural decompression 5. Irritants and detergents may not produce burns, but can damage eyes by inflammation or drawing water into the tissues. Cover with protective shield or paper cup; do not patch eye directly or pad under metal shield. Avulsed tooth: Avoid touching root, pick up by crown; do not wipe off, if dirty rinse under cold water for 10 sec. Mandible fx: Cannot open/close jaw, spit/swallow effectively; malocclusion/sublingual hematoma: no chin lift; aspiration risk 4. Rapid neuro exam for evidence suggesting traumatic brain injury Reassess at least q. If nonresponsive to verbal efforts to calm them or uncooperative in remaining still: Restrain as necessary per system policy. Gently attempt to align long-bone fx unless open; resistance to movement; extreme pain, or involves a joint 3. Immobilize/splint per procedure; If pulses lost after applying a traction splint: Do not release traction. Acute injury: Apply cold pack over injury site and elevate extremity after splinting unless contraindicated. Transport amputations above the wrist or ankle to a replantation center if ground transport times are 30 minutes or less. Stabilize object with bulky dressings; insert gauze rolls into the mouth to absorb excess blood. Condition in which a person is trapped in an upright position within a safety harness without any movement for a period of time obstructing normal venous return from legs to torso. At risk for Reflow Syndrome: Occurs when toxins that accumulated in pooled blood suddenly return to body after pt lies flat following suspension release. If conscious: Position sitting up with legs bent at the hips and knees for at least 30 min. A backboard can induce pain, agitation, and respiratory compromise, & decrease tissue perfusion at pressure points leading to pressure sores. A backboard or similar device may be useful to facilitate spine precautions during extrication. Securing a pt to a stretcher w/o a backboard, with or without a c-collar is acceptable for maintaining spine precautions during transport. Unless necessary to maintain an open airway/other compelling reasons, keep neck/back in original position (of a deformity) until exam is done. Stop if pain or resistance; apply an appropriately sized c-collar (unless contraindicated). Secure head, neck, and torso to a stable reference point (scoop stretcher or firm padded surface) with blocks, blanket roll, or head immobilizer so flexion, extension, and/or rotation is minimized. If using a scoop stretcher or spine board, secure device & patient to ambulance cot with appropriate straps. Selective spine precaution guidelines: See below - Additional caveats: Penetrating trauma to head, neck, or torso: No spine precautions Ambulatory at scene or long transport time: apply c-collar and secure to firm padded surface (stretcher) w/o scoop or board Stable pt. Board should have recess for head or elevate torso 1-2 cm to avoid neck flexion when immobilized. If nonresponsive to verbal efforts to calm them or uncooperative in remaining still: Restrain prn per system policy/procedure. The sports medical team must be familiar with the types of protective equipment specific to the sport and techniques for equipment removal. Equipment removal should be directed by those with the highest level of expertise and performed by at least 3 trained rescuers competent in the procedure at the earliest possible time (prior to transport). Do not remove equipment until at least 3 persons can assist unless an extreme airway emergency exists. The airway cannot be observed with helmet in place Contraindications to helmet removal: - Paresthesia or neck pain during removal; suggests worsening stretch or pressure on nerve endings. Call for an officer; describe incident: nature, location, presence of debris, hazards, traffic, entrapments, estimated # patients, ask dispatch to alert Resource Hospital if possible med-lg scale incident; help with triage/treatment when initial communication is complete. If small-scale incident: Contact hospital (per local policy/procedure) to distribute remaining patients. Establish loading area accessible to treatment area, that allows safe/coordinated access & egress Request ambulances from staging. Assign pts to ambulances; ensure appropriate loading (prioritizing pts based on triage/trauma score). Scene safety: If hazard is suspected, approach site w/ extreme caution, position personnel, vehicles, and command post at a safe distance (200-300 ft) upwind of the site. Chemical protective clothing should be worn when local and systemic effects of possible agents are unknown. Scene size up: Consider dispatch information (multiple persons seizing or having difficulty breathing) Does scene look routine? Establish hot & warm zones & perimeters Isolate/secure area by establishing boundary of the contaminated area and a non-contaminated buffer area. State & Local governmental agencies - may need water control, natural resources and public utilities for full response. Treatment Rescue victims if possible; provide life-saving care in the hot zone and move pts to the warm zone for further treatment and monitoring. If dermal chemical exposure: Determine decontamination needs: establish decon area; avoid cross-contamination; decontaminate pts/rescuers Cover open wounds with dressings and roller bandage. Transport contaminated victims by positioning a clean stretcher on the clean side of the control line with a clean sheet to receive and cover the victim. Tuck the clean sheet around the patient to reduce risk of contaminating the ambulance. Rescuers should remove outer protective clothing/gloves and don clean gloves for handling patient enroute. Cover floor of ambulance with a securely taped sheet or paper to possibility of contaminating ambulance. Decontamination at hospital: If radioactive exposure: Rescue personnel should be thoroughly surveyed for contamination. Onset of action or toxicity can occur within minutes up to a few hours depending on concentration of the gas. Cholinergic S&S: Salivation/sweating, lacrimation, urination, defecation, gastrointestinal distress, emesis, breathing difficulty with bronchospasm and copious secretions, arrhythmias, miosis (pinpoint pupils) resulting in blurred vision, headache, unexplained runny nose, chest tightness, jerking, twitching, staggering, seizures, coma, apnea, death S&S vesicants (blistering agents). Contraindications: Do not use Auto-Injectors for prophylaxis or on children < 88 lbs (40 kg) When a nerve agent has been ingested, exposure may continue for some time due to slow absorption from the lower bowel and fatal relapses have been reported after initial improvement. Contact Resource Hospital to alert them of incident and to request Chem Pac supplies. Definitions: Active shooter event - vent involving one or more individuals actively engaged in causing death and/or great bodily harm using firearms in a confined and/or populated area Ballistic Protective Equipment - Protective vest, helmet, and eyewear that are made to protect the wearer from ballistic threats such as gunfire, shrapnel, or sharp objects meant to do bodily harm. When in effect, occupants of the building will ignore all bells and fire alarms unless they receive verbal instructions from local emergency responders or the conditions warrant the evacuation of the area (fire, structural damage). On duty Shift Commanders shall be notified by dispatch if any hard lockdowns occur within their response areas. Places all reserve resources in a central location and requirement implementation of a Staging Officer. May also be used after the incident is stabilized to prevent the accidental spoliation of evidence by first responders. Second, a situation in the building where the school or local emergency responders need to keep students and staff in their classrooms and away from an incident or activity. During soft lockdowns, student and staff can continue normal classroom activities, but shall not leave the classroom or officers until advised to do so. The on-duty Shift Commander shall be notified by dispatch of any Soft Lockdowns within their response areas.
Buy cheap keppra 250 mg online. Atlas Genius "Symptoms".
It is used in children above 5 years and in younger children in place of triple antigen when pertussis vaccine is contraindicated symptoms 6 days after conception 500mg keppra otc. Pentavalent vaccine It contains toxoids of tetanus and diphtheria along with pertussis vaccine treatment stye proven keppra 500 mg, hepatitis B vaccine and Haemophilus influenzae type b (Hib) vaccine medications with aspirin order keppra 500mg. Used in place to triple antigen for primary immunization of infants medicine in ancient egypt discount keppra 500mg, it affords protection against two additional common infections symptoms neck pain order keppra 500mg online, and reduces the total number of injections that the infant receives for protection against these 5 infections medications prescribed for anxiety cheap keppra 250mg amex. Pentavalent vaccine has been used in many countries, and now Government of India is introducing it in a phased manner in its universal immunization programme for infants and children. However, recently few infant deaths have been reported, though the relationship between these and the vaccine is not clear. At 10 years At 16 years It is the preparation of choice for primary active immunization against the 3 diseases in children below 5 years age. A positive test contraindicates administration but a negative test does not completely rule out systemic sensitivity. These may be nonspecific (normal) or specific (hyperimmune) against a particular antigen. However, large doses and repeated injections do increase risk; adrenaline should be available. It is especially valuable in agammaglobulinemia, premature infants and in patients of leukemia or those undergoing immunosuppression. It can augment the response to antibiotics in debilitated patients with bacterial infections. Tetanus (a) Tetanus immune globulin (human) It is indicated for prophylaxis in non-immunized persons receiving a contaminated wound who are at high risk of developing tetanus. If tetanus toxoid is given at the same time (but at a different site), development of primary immune response to the toxoid is not interfered with. It has also been used for the treatment of clinical tetanus, but the efficacy is variable. It is indicated promptly after suspected exposure and is given simultaneously with rabies vaccine to nonimmunized individuals. In case of viper bite some serum should also be infiltrated around the site to prevent venom induced gangrene. The antitoxin neutralizes the exotoxin released at the site of Allergic reactions, including anaphylactic shock, to the serum are possible. When time permits, sensitivity test should be done; otherwise adrenaline may be injected s. Chapter 69 Drug Interactions Drug interaction refers to modification of response to one drug by another when they are administered simultaneously or in quick succession. The possibility of drug interaction arises whenever a patient concurrently receives more than one drug, and the chances increase with the number of drugs taken. More commonly, multiple drugs are used to treat a patient who is suffering from two or more diseases at the same time. The chances of unintended/adverse drug interactions are greater in this later situation, because an assortment of different drugs may be administered to a patient depending on his/her diseases/symptoms. Several drug interactions are desirable and deliberately employed in therapeutics. These are well-recognized interactions and do not pose any undue risk to the patient. The focus of attention in this chapter are drug interactions which may interfere with the therapeutic outcome or be responsible for adverse effects, or may even be fatal (bleeding due to excessive anticoagulant action). More importantly, a large section of patients may be receiving one or several drugs for their chronic medical conditions like hypertension, diabetes, arthritis, etc. The physician may prescribe certain drugs which may interact with those already being taken by the patient and result in adverse consequences. It is, therefore, imperative for the doctor to elicit a detailed drug history of the patient and record all the medication that he/she is currently on. The list of potential adverse drug interactions is already quite long and constantly growing. It is practically impossible for anyone to know/remember all possible drug interactions. Fortunately, the clinically important and common drug interactions that may be encountered in routine practice are relatively few. More exhaustive Regular medication drugs (Likely to be involved in drug interactions) 1. Certain types of drugs (see box) can be identified that are most likely to be involved in clinically important drug interactions. The physician may take special care and pay attention to the possibility of drug interactions when the patient is receiving one or more of such medications, or when the doctor intends to prescribe any of such drugs. In certain cases, however, the mechanisms are complex and may not be well understood. Few interactions take place even outside the body when drug solutions are mixed before administration. Pharmacokinetic interactions these interactions alter the concentration of the object drug at its site of action (and consequently the intensity of response) by affecting its absorption, distribution, metabolism or excretion. Absorption Absorption of an orally administered drug can be affected by other concurrently ingested drugs. This is mostly due to formation of insoluble and poorly absorbed complexes in the gut lumen, as occurs between tetracyclines and calcium/iron salts, antacids or sucralfate. Ketoconazole absorption is reduced by H2 blockers and proton pump inhibitors because they decrease gastric acidity which promotes dissolution and absorption of ketoconazole. Antibiotics like ampicillin, tetracyclines, cotrimoxazole markedly reduce gut flora that normally deconjugates oral contraceptive steroids secreted in the bile as glucuronides and permits their enterohepatic circulation. Several instances of contraceptive failure have been reported with concurrent use of these antibiotics due to lowering of the contraceptive blood levels. Alteration of gut motility by atropinic drugs, tricyclic antidepressants, opioids and prokinetic drugs like metoclopramide or cisapride can also affect drug absorption. Distribution Interactions involving drug distribution are primarily due to displacement of one drug from its binding sites on plasma proteins by another drug. Another requirement is that the displacing drug should bind to the same sites on the plasma proteins with higher affinity. Displacement of bound drug will initially raise the concentration of the free and active form of the drug in plasma that may result in toxicity. However, such effects are usually brief, because the free form rapidly gets distributed, metabolized and excreted, so that steady-state levels are only marginally elevated. Quinidine has been shown to reduce the binding of digoxin to tissue proteins as well as its renal and biliary clearance by inhibing the efflux transporter P-glycoprotein, resulting in nearly doubling of digoxin blood levels and toxicity. They may thus affect the bioavailability (if the drug undergoes extensive first pass metabolism in liver) and the plasma half-life of the drug (if the drug is primarily eliminated by metabolism). A number of drugs induce microsomal drug metabolizing enzymes and enhance biotransformation of several drugs (including their own in many cases). Barbiturates, phenytoin, carbamazepine, rifampin, cigarette smoking, chronic alcoholism and certain pollutants are important microsomal enzyme inducers. Instances of failure of antimicrobial therapy with metronidazole, doxycycline or chloramphenicol have occurred in patients who are on long-term medication with an inducing drug. Contraceptive failure and loss of therapeutic effect of many other drugs have occurred due to enzyme induction. On the other hand, the toxic dose of paracetamol is lower in chronic alcoholics and in those on enzyme inducing medication, because one of the metabolites of paracetamol is responsible for its overdose hepatotoxicity. Excretion Interaction involving excretion are important mostly in case of drugs actively secreted by tubular transport mechanisms. Aspirin blocks the uricosuric action of probenecid and decreases tubular secretion of methotrexate. Change in the pH of urine can also affect excretion of weakly acidic or weakly basic drugs. Pharmacodynamic interactions these interactions derive from modification of the action of one drug at the target site by another drug, independent of a change in its concentration. This may result in an enhanced response (synergism), an attenuated response (antagonism) or an abnormal response. The phenomena of synergism and antagonism are described in Chapter 4, and are deliberately utilized in therapeutics for various purposes. Of clinical significance are the inadvertent concurrent administration of synergistic or antagonistic pair of drugs with adverse consequences. Allopurinol Penicillin Ampicillin Cephalosporins Ampicillin 6-Mercaptopurine Azathioprine Warfarin Theophylline Aspirin and other antiplatelet drugs Oral anticoagulants Phenytoin Warfarin Sulfonylureas Thiazide diuretics Oral contraceptives 7. Inhibition of tubular secretion prolongation of antibiotic action; Desirable interaction utilized for single dose therapy. Perturbation of surface receptors on platelets additive platelet inhibition risk of bleeding; Avoid concurrent use. Displacement$ + inhibition of metabolism phenytoin toxicity; Avoid concurrent use. Interruption of enterohepatic circulation of the estrogen failure of contraception; Advise alternative contraception. Possibly accumulation of acetaldehyde disulfiram-like or bizarre reactions; Warn the patient not to drink alcohol. Inhibition of metabolism toxicity of object drug; Monitor and reduce dose of object drug. Tetracyclines Likely interaction and comments Increased risk of myopathy; Caution in concurrent use. Rise in plasma Li+ level due to decreased excretion; Avoid use of tetracycline or monitor and reduce dose of lithium. Antianabolic effect of tetracycline increases urea production which is retained by the diuretic; Avoid concurrent use. Decreased excretion-rise in Li+ level-toxicity; Reduce dose of lithium and monitor level. Hypokalaemia caused by diuretic increases digoxin toxicity; Give K+ sparing diuretic/K+ supplements. Bactericidal action of penicillins and cephalosporins may be antagonized by the bacteriostatic antibiotics; Avoid concurrent use. Mutual antagonism of antibacterial action due to proximal binding sites on bacterial ribosomes; Avoid concurrent use. Diuretics Tetracyclines Fluoroquinolones Minocycline Aminoglycoside antibiotics Tetracycline Lithium Digoxin 16. Phenobarbitone Phenytoin Carbamazepine Rifampin Induction of metabolism loss of efficacy of object drug; Avoid concurrent use or increase dose of object drug with monitoring. Enhanced risk of bleeding due to antiplatelet action and gastric mucosal damage; Avoid concurrent use. Reduced K+ conserving action due to decreased tubular secretion of canrenone (active metabolite of spironolactone); Avoid concurrent use. Reduced hepatic clearance of lidocaine; Ceiling amount used in local anaesthesia is reduced. Exaggerated cardiac depression, precipitation of arrhythmias; Avoid concurrent use. Pronounced and asymptomatic hypoglycaemia can occur when propranolol is administered to diabetics receiving insulin/ sulfonylureas, due to blockade of adreno- ceptors which contribute to recovery from hypoglycaemia as well as some hypoglycaemic symptoms. Additive prolongation of prothrombin time and bleeding by administration of ceftriaxone or cefoperazone to a patient on oral anticoagulants. Excessive platelet inhibition resulting in bleeding due to simultaneous use of aspirin/ ticlopidine/clopidogrel and carbenicillin. Increased risk of bleeding due to concurrent use of antiplatelet drugs (aspirin, clopidogrel) with anticoagulants (warfarin). Additive ototoxicity due to use of an aminoglycoside antibiotic in a patient receiving furosemide. Antagonism of bactericidal action of -lactam antibiotic by combining it with a bacteriostatic drug like tetracycline, erythromycin or clindamycin. Reduction in antihypertensive action of clonidine by chlorpromazine and imipramine, possibly due to blockade of central action of clonidine. Blunting of K+ conserving action of spironolactone by aspirin, because it inhibits the tubular secretion of canrenone (an active metabolite of spironolactone). Blockade of antiparkinsonian action of levodopa by neuroleptics and metoclopramide having antidopaminergic action. Abnormal responses sometimes result from pharmacodynamic interaction between certain drugs. Drug interactions before administration Certain drugs react with each other and get inactivated if their solutions are mixed before administration. In combined oral or parenteral formulations, the manufacturers take care that such incompatibilities do not take place. In practice situations, these in vitro interactions occur when injectable drugs are mixed in the same syringe or infusion bottle.