




|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Barbara McClaskey, PhD, MN, RNC, ARNP
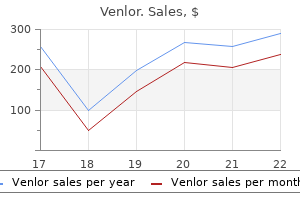
An adverse reaction cannot be considered immunological until there is proof of an immune-mediated mechanism anxiety symptoms lasting all day discount venlor 75mg mastercard. The term food intolerance should be used to describe all abnormal but reproducible reactions to food when the causative mechanism is unknown (Table 4 anxiety symptoms mimic heart attack venlor 75mg discount. The phrase anxiety girl meme 75 mg venlor, food allergic disease should be used only when the abnormal reaction is proved to be immunologically mediated anxiety symptoms for no reason 75mg venlor. The public perception of their illnesses being caused by food has been shown to be over 10 times greater than the proven prevalence of food intolerance anxiety in relationships venlor 75 mg on-line. Nearly threequarters of patients present with immediate gastrointestinal symptoms anxiety symptoms one side of body buy venlor 75mg amex. Food intolerance must be considered to be a rare/unproven cause of symptoms that occur remote from gut (such as attention deficit disorders, arthritis or enuresis); patients apparently benefiting from dietary manipulation have been from highly selected groups. Most reports of proven food intolerance in adults incriminate nuts, milk, eggs, fish, wheat and chocolate, where a direct nonimmunological mechanism is suspected (section 4. On the other hand allergy to peanuts is IgE mediated and is becoming more common (Box 4. A minute quantity of peanut antigen can cause a life-threatening reaction, as in Case 4. Food intolerance Gut related 75% of reactions in children Remote sites 90% of reactions in adults + + - Immediate Mouth ulceration Angioedema Abdominal pain Vomiting Anaphylaxis Late (> 2h) Diarrhoea Bloating Malabsorption Rhinitis Asthma Urticaria Eczema? Some atopic children and adults report itching and swelling of the mouth, tongue and soft palate after eating fresh fruit, typically apples, pears, cherries, plums and peaches (see Case 4. This occurs in patients allergic to birch tree pollen because of allergic cross-reactivity between pollen and certain fruits. The allergens are heat-labile and destroyed by cooking, so patients can tolerate cooked fruit or jams. The oral allergy syndrome does not normally progress to cause systemic anaphylaxis. For the previous 4 years he had noticed that eating certain fruits, particularly apples, pears and peaches, produced tingling, burning and swelling of his lips and gums. These symptoms occurred within seconds of starting to eat these fruits and lasted about 30 min, but were never associated with vomiting, urticaria, bronchospasm or circulatory collapse. He was worried that these reactions heralded an increasing potential to develop anaphylaxis to fruit. He was skin-prick tested to a variety of allergens: he showed strongly positive reactivity to tree pollen and peach but a negative reaction to the commercial apple solution. At the age of 5 years, she vomited about 1 min after eating a bar of chocolate containing nuts. Three years later, she developed marked angioedema of her face, lips and tongue, followed by tightness of her throat and vomiting: this occurred 23 min after friends of her brother decided to test her allergic status by pushing peanuts into her mouth and holding her jaws shut! Within seconds, she developed angioedema of her lips and tongue, difficulty in breathing, and felt light-headed. Following an emergency call, she was injected with intramuscular adrenaline (and intravenous hydrocortisone inappropriately) by the paramedical service, and admitted to hospital overnight. Her parents later recalled that one ice-cream scoop was used by the vendor to dispense all flavours: the customer immediately before the patient had been served a nut-flavoured ice cream. She was advised to wear a medical alert bracelet as a warning to emergency personnel of a possible cause of sudden collapse, and to carry with her at all times a self-injectable form of epinephrine (adrenaline). These include irritant, toxic, pharmacological or metabolic effects of foods, enzyme deficiencies, or even the release of substances produced by fermentation of food residues in the bowel. For instance, some foods contain pharmacologically active substances (such as tyramine or phenylethylamine) that may act directly on blood vessels in sensitive subjects to produce symptoms such as migraine. Salicylates, for instance, inhibit synthesis of prostaglandins and cause release of mast cell mediators. Elimination and challenge diets form the basis of the diagnosis of food allergic disease. A food challenge must be carefully monitored and conducted under double-blind conditions in an expert specialist centre. Testing the blood or skin of a patient clearly does not always reflect what is happening at the level of the gut mucosa. When evaluated under double-blind conditions, this method lacked validity: the high frequency of positive responses to the extracts appeared to be due to suggestion and chance. Other methods, such as hair analysis, are more a matter of gullibility and faith than evidence-based medicine. Recognition of the offending food and its elimination from the diet is the cornerstone of treatment of truly allergic patients. Some patients know that a certain food, such as peanuts, regularly produces their symptoms; this food must be avoided a simple elimination diet. Coeliac disease involves T cells sensitized to the dietary antigens of gluten and can be considered a type of allergy since an extrinsic antigen is involved, as shown by the clinical improvement following gluten withdrawal. However, since the autoantibodies to tissue transglutaminase and endomysium are also a feature, it is more commonly considered with the autoimmune diseases. Urticaria refers to transient episodes of demarcated, oedematous, erythematous, pruritic lesions with a raised edge. It has such a distinctive appearance that clinical diagnosis is usually easy; the difficult task is finding the cause, since laboratory tests are unhelpful. Angioedema is a similar process occurring in the deep dermis, subcutaneous tissues or mucous membranes. Urticaria and angioedema commonly coexist, except in hereditary angioedema in which urticaria plays no part. Any sudden increase in local vascular permeability in the dermis will cause urticaria. Mast cells in the dermis are an important source of the vasoactive mediators and since a number of mediators are involved. Acute urticaria is short-lived, although the cause is identified in only 50% of cases. Episodes caused by an IgE-mediated reaction to extrinsic antigens, such as foods, are usually obvious from the history and can be confirmed by skin-prick testing. Chronic urticaria is conventionally defined as the occurrence of widespread urticarial wheals on a daily or almost daily basis for at least 6 weeks (Case 4. It affects over one in 200 of the population at some time during their lives and can be very disabling. In patients with physical urticarias, itching and wheals are provoked by physical stimuli such as scratching the skin (dermographism), rapid cooling (cold urticaria), sun exposure (solar urticaria), water (aquagenic urticaria) or exercise, heat or emotion (cholinergic urticaria). Once the physical urticarias and urticarial vasculitis are eliminated, chronic urticaria is divided into autoimmune chronic urticaria (45%) and idiopathic chronic urticaria (55%). Avoidance of triggering factors is an obvious step and elimination of Helicobacter pylori infection has been associated with remission of chronic urticaria in some patients. Low-sedation anti-H1 antihistamines, which have a low incidence of adverse effects, are the mainstay of treatment, often in high doses. Montelukast is helpful but systemic steroids are not indicated in chronic urticaria because of the high doses required, the development of intolerance and the problems of steroid toxicity. For patients with severe autoimmune disease, high-dose ciclosporin therapy is effective. Despite treatment, about 20% of patients still have chronic urticaria 10 years following presentation. In infants, the dermatitis often appears on the face first, followed by the flexural aspects of the arms and legs (Fig 4. In older children and adults, the flexures are frequently involved, with thickening, lichenification and scaling of the epidermis, which tends to crack and weep. Spontaneous resolution occurs in many patients; about half clear by the age of 7 years and 90% by their late teens but, in the remainder, eczema persists into adult life. The commonest complication is superadded bacterial infection, but some children may develop ocular complications, such as cataracts, psychological problems or side effects from prolonged treatment (particularly with corticosteroids). Although atopic children handle most viruses normally, superadded infection with herpes simplex virus is life threatening. The diagnosis of atopic eczema is based on the clinical features, usually with a personal or family history of atopy. The concordance rate is up to 85% in monozygotic twins compared with 30% in dizygotic twins. This is in part due to disease causing mutations in filaggrin, found to be the cause of ichthyosis vulgaris in 2006 and a strong genetic risk factor for atopic eczema. Since then large-scale genome-wide association studies have confirmed this and identified further susceptibility genes that suggest that both changes in the epidermal barrier and in immunity play a role in the pathogenesis of this disease. Filaggrin monomers become part of the lipid envelope responsible for skin barrier function as well as assisting positively in water retention. Mutations that result in loss of functioning filaggrin result in dehydration of the epidermis and defects in the barrier allow exposure to allergens and microbes, resulting in Th2 polarized lymphocyte responses and subsequent chronic skin inflammation. Filaggrin polymorphisms may be involved in other atopic conditions with leaky barriers. Familial aggregation analysis shows a stronger clustering of atopic eczema between siblings than between siblings and parents, suggesting that environmental factors are also important. Exposure to the triggers in atopic eczema is often via the skin, such triggers probably being infections or irritants. House dust mite is one provoking factor and reduction in the house dust mite allergen load in the home may result in significant clinical improvement. The role of food intolerance is controversial: controlled studies of dietary manipulation in children suggest that it is an uncommon trigger, particularly in older children (see Table 4. Staphylococcus aureus colonization and infection is found in over 90% of patients with atopic eczema and is the most likely source of exacerbation of the skin inflammation by acting as a superantigen (section 2. T lymphocytes migrating into the skin are highly enriched for cutaneous lymphoid antigen-expressing memory Th2 cells. The most measurable immunological abnormality is a raised serum IgE level in up to 90% of patients. Since IgE production is under T-cell control, the abnormal Chapter 4: Anaphylaxis and Allergy / 103 Box 4. Th1 cell response with interferon- production) · Occurrence of eczema in primary immunodeficiency diseases. Atopic dermatitis is due to an itch that, when scratched, results in a rash, and even bleeding if the scratching is severe. Current management of atopic eczema is directed at the elimination of exacerbating factors including allergens, infection and irritants, and the reduction of cutaneous inflammation. Bland emollients, which soothe the skin, and rehydration are crucial to provide some symptomatic relief of itching, resulting in an artificial barrier against further triggers. Topical corticosteroids suppress inflammation and also help to reduce itching; they are the most successful agents currently available to treat eczema. Long-term use of potent steroids may lead to atrophy of the dermis and epidermis and may even be accompanied by significant systemic absorption if they are applied in excess. There is limited and conflicting evidence regarding the efficacy of bed covers impermeable to mite allergens and other measures to reduce any potential triggers. A number of therapeutic approaches are now directed at modulating signal transduction in Th2 lymphocytes. Ciclosporin has proved safe and effective as a short-term treatment for severe, refractory atopic eczema. A 38-year-old woman presented with a 2-year history of abdominal bloating, cramping abdominal pains and loose stools. One attack occurred about 8 h after a meal of pasta in a local restaurant and led her to believe her symptoms were food-related. She initially eliminated wheat-based products from her diet and then, because the attacks continued, dairy products as well. She was referred to a gastroenterologist and investigated extensively: gastroduodenal endoscopy, duodenal biopsy, barium meal, colonoscopy and pancreatic function tests were all normal. She continued to believe her symptoms were food related: vague muscular pains, headaches, poor concentration and fatigue were attributed to other foods, which were then eliminated from her diet. Physical examination showed an undernourished woman with no other abnormal findings. She had no detectable antibodies to tissue transglutaminase, endomysium or gliadin (see Chapter 19). The report listed 24 foods to which she was allergic, many of which she had felt able to tolerate previously. Her diet had become increasingly restricted: expert dietetic assessment showed her diet to be nutritionally unsound, with deficient intake of protein, fat, fat-soluble vitamins and trace elements. The diagnosis was that of psychological food aversion and irritable bowel syndrome. The lesions appeared suddenly and lasted from 6 to 12 h, to be replaced by new lesions at other sites. In addition, he had experienced four episodes of sudden swelling of lips that took 48 h to subside. He was unaware of any triggering factors and there was no personal or family history of atopy. On examination, the lesions consisted of raised, red, irregular patches, some with white centres, and were typically urticarial. Laboratory investigations showed a normal haemoglobin and white cell count, with no eosinophilia. His complement C4 and C1 inhibitor levels were normal, excluding hereditary angioedema (see Case 11. The urticaria was fairly well controlled by a long-acting antihistamine (levocetirizine) but he was reluctant to take these tablets on a long-term basis. Three years later, his urticarial lesions are still present, although less severe; their cause is unknown. At the age of 4 weeks, he was admitted with a 2-day history of screaming attacks, loose motions and rectal bleeding. He was treated conservatively, but 3 days after discharge his symptoms recurred, together with patches of eczema on his arms and trunk.
Diseases
You can now sign in with the email address and password you used when you created your VitalSource Bookshelf Account anxiety symptoms lingering discount 75mg venlor mastercard. CourseSmart also offers instructors an immediate anxiety 7 weeks pregnant buy venlor 75mg with mastercard, efficient anxiety symptoms signs order venlor 75mg with mastercard, and environmentally-friendly way to review this textbook for your course anxiety 300mg 75mg venlor with visa. With CourseSmart anxiety uncertainty management theory 75 mg venlor with amex, you can create lecture notes quickly with copy and paste anxiety zone breast cancer buy 75 mg venlor with mastercard, and share pages and notes with your students. Access your CourseSmart digital textbook from your computer or mobile device instantly for evaluation, class preparation, and as a teaching tool in the classroom. Image not available in this digital edition We hope you enjoy using your new textbook. Individuals with markedly deficient immune responses, if untreated, succumb to infections in early life. There is, therefore, a selective evolutionary pressure for a really efficient immune system. Although innate systems are fast in response to pathogens, the evolution to adaptive responses provided greater efficiency. However a parallel evolution in pathogens means that all species, plants, insects, fish, birds and mammals, have continued to improve their defence mechanisms over millions of years, giving rise to some redundancies as well as resulting in apparent complexity. The aim of this chapter is to provide an initial description of the molecules involved, moving onto the role of each in the immune processes rather than the more traditional sequence of anatomical structure, cellular composition and then molecular components. It is hoped that this gives a sense of their relationship in terms of immediacy and dependency as well as the parallel evolution of the two immune systems. Innate immunity, though phylogenetically older and important in terms of speed of a response, is less efficient. Humoral components (soluble molecules in the plasma) and cells in blood and tissues are involved. Such responses are normally accompanied by inflammation and occur within a few hours of stimulation (Table 1. Adaptive humoral responses result in the generation of antibodies reactive with a particular antigen. Good examples of cellular immune responses are the rejection of a graft by lymphoid cells as well as graft-versus-host disease, where viable transferred cells attack an immunologically compromised recipient that is unable to fight back. Antibody-producing lymphocytes, which are dependent on the bone marrow, are known as B cells. Cellular immune responses are dependent on an intact thymus, so the lymphocytes responsible are known as thymus-dependent (T) cells. It involves professional cells, known as classical dendritic cells, that recognize general pathogen features or specific antigenic molecules, process the antigens and present antigen fragments to the other cells of the immune systems as well as initiating non-specific inflammation to the pathogen. In terms of disease, like other organs, the immune system may fail (immunodeficiency), may be come malignant (lymphoid malignancies) or produce aberrant responses (such as in autoimmunity or allergy). This chapter describes the normal immune system in order to lay the basis for discussing these ways in which it can go wrong and so cause disease. Phagocytic cells also recognize particular patterns associated with potentially damaging materials, such as lipoproteins and other charged molecules or peptides. Some low-molecular-weight molecules, called haptens, are unable to provoke an immune response themselves, although they can react with existing antibodies. Such substances need to be coupled to a carrier molecule in order to have sufficient epitopes to be antigenic. Pure lipids and nucleic acids are poor antigens, although they do activate the innate system and can be inflammatory. Thymus-dependent antigens require T-cell participation to provoke the production of antibodies; most proteins are examples. Endotoxin, another thymus-independent antigen, not only causes specific B-cell activation and antibody production but also acts as a stimulant for all B cells regardless of specificity. Factors other than the intrinsic properties of the antigen can also influence the quality of the immune response (Table Table 1. The use of adjuvants in humans, important in vaccines against infective agents and tumours, is discussed in section 7. Self-antigens are not recognized by dendritic cells, so inflammation and co-stimulation of T cells (see section 1. There are mechanisms to control any aberrant adaptive responses to self-antigens, by prevention of production of specific receptors and regulation of the response if the immune system is fooled into responding (see Chapter 5, Autoimmunity). Mature myeloid dendritic cells Antigen presentation to immature T cells for specific differentiation ++ ++ ++ - Antigen capture Absent or low Absent or low Absent or low ++ Very rapid Reduced (approx. These are evolutionarily conserved proteins found on macrophages, dendritic cells and neutrophils. The variable regions of the alpha () and beta () chains make up the T idiotype, i. Antigenic epitopes, having been processed by dendritic cells, are recognized by cells of the adaptive system by means of specific receptors. However, these molecules are known to play a fundamental role in immunity by presenting antigenic peptides to T cells. The detailed structure of class I antigens was determined by X-ray crystallography. It has a folded structure similar to class I antigens with the peptide-binding groove found between the and chains. The amino (N) terminal domains of the heavy and light chains include the antigen-binding site. The amino acid sequences of these N-terminal domains vary between different IgM J chain IgM IgM IgM IgM. Most of these differences reside in three hypervariable areas of the molecule, each only 610 amino acid residues long. In the folded molecule, these hypervariable regions in each heavy and light chain come together to form, with their counterparts on the other pair of heavy and light chains, the antigen-binding site. The structure of this part of the antibody molecule is unique to that molecule and is known as the idiotypic determinant. In any individual, approximately 106107 different antibody molecules could be made up by 103 different heavy chain variable regions associating with 103 different light chain variable regions, though there are even more epitopes due to further variation during the later processing (see section 1. The heavy chains determine the isotype of the antibody and the ultimate physiological function of the particular antibody molecule. Once the antigen-binding site has reacted with its antigen, the molecule undergoes a change in the conformation of its heavy chains in order to take part in effector reactions, depending on the isotype of the molecule. Like those coding for other macromolecules, the genes are broken up into coding segments (exons) with intervening silent segments (introns). The heavy chain gene set on chromosome 14 is made up of small groups of exons representing the constant regions of the heavy chains [e. They have to be able to recognize these targets and distinguish them from normal cells. The major purpose of the complement pathways is to provide a means of removing or destroying antigens, regardless of whether or not these are coated with antibody. This requires that complement components recognize damaging material such as immune complexes (antigen combined with antibodies) or foreign antigens. Each accessory molecule has a particular ligand a corresponding protein to which it binds. These ligands are present on all cells which require close adhesion for functioning; for example, there are those on T cells for each of the many cell types that can activate or respond to T cells (antigen-presenting cells, endothelial cells, etc. There are several families of accessory molecules, but the most important appear to be the immunoglobulin supergene family of adhesion molecules, which derives its name from the fact that its members contain a common immunoglobulin- Chapter 1: Basic Components: Structure and Function / 11 like structure. Members of their family strengthen the interaction between antigen-presenting cells and T cells. Adhesion molecules, for binding leucocytes (both lymphocytes and polymorphonuclear leucocytes) to endothelial cells and tissue matrix cells, are considered in section 1. Several of the same mechanisms are used in both types of immune responses, especially in killing of target cells, suggesting that evolution of immune responses has been conservative in terms of genes, though with much redundancy to ensure the life-preserving nature of the immune systems in the face of rapid evolution of pathogenic microbes. Antibodies Antibodies are the best described effector mechanisms in adaptive immunity. They are the effector arm of B cells and are secreted as soluble molecules by plasma cells in large quantities, to be carried in the blood and lymph to distant sites. IgM is a large molecule whose major physiological role is intravascular neutralization of organisms (especially viruses). IgM has five complement-binding sites, resulting in excellent complement activation and subsequent removal of the antigen antibodycomplement complexes by complement receptors on phagocytic cells or complement-mediated lysis of the organism (see section 1. Of the four subclasses, IgG1 and IgG3 activate complement most efficiently and are responsible for clearing most protein antigens, including the removal of microorganisms by phagocytic cells (see section 1. IgG2 and IgG4 react predominantly with carbohydrate antigens (in adults) and are relatively poor opsonins. IgM has five complement-binding sites, which results in excellent activation of the classical complement pathway. It is the only immunoglobulin to provide immune protection to the neonate (Table 1. IgE is produced by plasma cells but is taken up by specific IgE receptors on mast cells and basophils. IgE then provides an antigen-sensitive way of expelling intestinal parasites by increasing vascular permeability and inducing chemotactic factors via mast cell degranulation (see section 1. For this reason, therapeutic targeting of individual cytokines in disease has had limited success so far (effects of deletion of individual cytokine genes are listed in Table 1. Cytokines and chemokines Cytokines are soluble mediators secreted by macrophages or monocytes (monokines) or lymphocytes (lymphokines). These mediators act as stimulatory or inhibitory signals between cells; those between cells of the immune system were known as interleukins, (a phrase that has fallen out of general usage since the range of soluble molecules has widened so tremendously, though the individual names persist to avoid confusion). Cytokines that induce chemotaxis of leucocytes are referred to as chemokines, a name derived from chemo + kine, i. Some cytokines and interleukins have been redefined as chemokines as their function becomes clearer. Chemokines are structurally similar proteins of small molecule size (810 kDa), which are able to diffuse from the site of production to form a local concentration gradient along which granulocytes and lymphocytes can migrate towards the stimulus. There are two types of movement: migration of leucocytes to sites of inflammation and that of differentiating cells moving to a specific activation site (see section 1. There is little free IgD or IgE in serum or normal body fluids, since both act as surface receptors on mature B cells or mast cells respectively. Once V, D and J region rearrangement has taken place, further variation is introduced when antibodies are made, by the introduction of point mutations in the V region genes. Somatic hypermutation helps to increase the possible number of combinations and accounts for the enormous diversity of antibody specificities (1014), which by far exceeds the number of different B cells in the body (1010). Molecules for lysis and killing the other major sets of effector molecules are the cytolytic molecules, though less is known about their diversity or mechanisms of action. These cell types also secrete granzymes, enzymes that induce apoptosis in target cells (Table 1. The duplication of the functions of this essential phylogenetically ancient protein during evolution underlines the continued development of mammalian immunity to keep up with microbial invaders. There are other structurally similar cytokine receptors, leading to the classification of these receptors into five families of similar types of receptors, many of which have similar or identical functions, providing a safety net (redundancy) for their functions, which are crucial for both the innate and adaptive immune systems. Chemokine receptors from a family of G protein coupled receptors meaning that they are transmembrane and able to Chapter 1: Basic Components: Structure and Function / 15 activate internal signalling pathways. There are also FcRn involved in the transfer of IgG across the placenta and these receptors are also involved in IgG recirculation and catabolism. IgE receptors are found on mast cells, basophils and eosinophils for triggering degranulation of these cells. IgA receptors ensure the transport of polymeric IgA across the mucosal cells and other, possibly important, functions are slowly being defined. Complement receptors for fragments of C3 produced during complement activation also provide a mechanism for phagocytosis and are found on macrophages and neutrophils. Adhesion molecules are grouped into two major families: (i) integrins and (ii) selectins (Table 1. Depending on the structure of the subunit, integrins are subdivided into five families (1 to 5 integrins). Examples in other systems include 3 to 5 integrins mediate cell adhesion to extracellular matrix proteins such as fibronectin and vitronectin in the skin and laminin receptor in muscle. The selectin family is composed of three glycoproteins designated by the prefixes E (endothelial), L (leucocyte) and P (platelet) to denote the cells on which they were first described. Selectins bind avidly to carbohydrate molecules on leucocytes and endothelial cells and regulate the homing of the cells to sites of inflammation (see sections 1. To reach the site of invasion and destroy the pathogens, the components of the immune systems have to know where to go and to how to breach the normal barriers, such as the endothelial cells of the vascular system. Humoral factors (such as antibodies and complement) are carried in the blood and enter tissues following an increase in permeability associated with inflammation. Non-specific immunity is older, in evolutionary terms, than antibody production and antigen-specific T cells. The major cells involved in the innate system are phagocytic cells (macrophages and polymorphonuclear leucocytes), which remove antigens including bacteria, and dendritic cells which are the first cells to react to invaders. The major humoral components of the four complement pathways can either directly destroy an organism or initiate/facilitate its phagocytosis. Immunologically, endothelial cells are intimately involved in interactions with leucocytes prior to leaving the circulation to enter sites of tissue damage. The endothelium also plays an important role in regulating the turnover of IgG, through the presence of FcRn, a receptor that prevents IgG from undergoing lysosomal degradation (see sections 1. They synthesize and express adhesion receptors so they can stick to , and migrate out of, blood vessels into the tissues. Lymphoid and myeloid cells are derived from closely related stem cells in the bone marrow. Polymorphonuclear leucocytes develop in the bone marrow and emerge only when mature. Monocytes circulate for only a few hours before entering the tissues, where they may live for weeks or months as mature macrophages or dendritic cells.
Generic venlor 75mg with amex. Over 100 Anxiety Symptoms.
Laboratory screening for the diagnosis of children with primary immunodeficiencies anxiety 24 hours a day generic 75mg venlor with visa. Laboratory diagnosis of specific antibody deficiency to pneumococcal capsular polysaccharide antigens anxiety feels like venlor 75mg overnight delivery. Assessment of the antibody response to pneumococcal vaccine in high-risk populations anxiety attack symptoms quiz 75mg venlor overnight delivery. Estimating the protective concentration of anti-pneumococcal capsular polysaccharide antibodies anxiety 34 weeks pregnant discount venlor 75 mg fast delivery. Serotype-specific anti-pneumococcal IgG and immune competence: critical differences in interpretation criteria when different methods are used anxiety symptoms breathing purchase 75 mg venlor. Immunologic reconstitution following bone marrow transplantation for X-linked hyper IgM syndrome anxiety vs depression purchase venlor 75 mg mastercard. Analysis of in vitro lymphocyte proliferation as a screening tool for cellular immunodeficiency. Gene therapy for primary immunodeficiencies: looking ahead, toward gene correction. Severe phenotype of chronic granulomatous disease presenting in a female with a de novo mutation in gp91-phox and a non familial, extremely skewed X chromosome inactivation. Andreu N, Pujol-Moix N, Martinez-Lostao L, Oset M, Muniz-Diaz E, Estivill X, et al. Female agammaglobulinemia due to the Bruton tyrosine kinase deficiency caused by extremely skewed X-chromosome inactivation. Retrospective diagnosis of X-linked hyper-IgM syndrome in a family with multiple deaths of affected males. Pathogenesis, diagnosis, and management of primary antibody deficiencies and infections. Improving cellular therapy for primary immune deficiency diseases: recognition, diagnosis, and management. Use of intravenous immunoglobulin in human disease: a review of evidence by members of the Primary Immunodeficiency Committee of the American Academy of Allergy, Asthma and Immunology. Use of intravenous immunoglobulin and adjunctive therapies in the treatment of primary immunodeficiencies: a working group report of and study by the Primary Immunodeficiency Committee of the American Academy of Allergy Asthma and Immunology. B-cell function in severe combined immunodeficiency after stem cell or gene therapy: a review. The role of anti-IgA antibodies in causing adverse reactions to gamma globulin infusion in immunodeficient patients: a comprehensive review of the literature. Hyperimmune globulins and same-day thrombotic adverse events as recorded in a large healthcare database during 2008-2011. Immune globulins and same-day thrombotic events as recorded in a large health care database during 2008 to 2012. Hemolytic anemia following intravenous immunoglobulin therapy in patients treated for Kawasaki disease: a report of 4 cases. Catheter fracture and cardiac migration: a rare complication of totally implantable venous devices. Longitudinal decline in lung function in patients with primary immunoglobulin deficiencies. Antibiotics for the prevention of acute and chronic suppurative otitis media in children. Antibiotic prophylaxis for bacterial infections in afebrile neutropenic patients following chemotherapy. Recognition, clinical diagnosis and management of patients with primary antibody deficiencies: a systematic review. Allogeneic hematopoietic cell transplantation for primary immune deficiency diseases: current status and critical needs. Excellent survival after sibling or unrelated donor stem cell transplantation for chronic granulomatous disease. Update on gene therapy for adenosine deaminasedeficient severe combined immunodeficiency. Induction of tolerance to parental parathyroid grafts using allogeneic thymus tissue in patients with DiGeorge anomaly. Neonatal diagnosis of severe combined immunodeficiency leads to significantly improved survival outcome: the case for newborn screening. Tandem mass spectrometry, but not T-cell receptor excision circle analysis, identifies newborns with late-onset adenosine deaminase deficiency. Recommendations for live viral and bacterial vaccines in immunodeficient patients and their close contacts. Live viral vaccines in patients with partial DiGeorge syndrome: clinical experience and cellular immunity. The actin regulator coronin 1A is mutant in a thymic egress-deficient mouse strain and in a patient with severe combined immunodeficiency. Gene therapy for severe combined immunodeficiency due to adenosine deaminase deficiency. New insights into the pathogenesis of adenosine deaminasesevere combined immunodeficiency and progress in gene therapy. Human adenylate kinase 2 deficiency causes a profound hematopoietic defect associated with sensorineural deafness. Moshous D, Pannetier C, Chasseval Rd R, Deist Fl, Cavazzana-Calvo M, Romana S, et al. Partial T and B lymphocyte immunodeficiency and predisposition to lymphoma in patients with hypomorphic mutations in Artemis. Cernunnos, a novel nonhomologous end-joining factor, is mutated in human immunodeficiency with microcephaly. Cernunnos influences human immunoglobulin class switch recombination and may be associated with B cell lymphomagenesis. Novel mutations and diverse clinical phenotypes in recombinase-activating gene 1 deficiency. Recombinase-activating gene 1 immunodeficiency: different immunological phenotypes in three siblings. Early defects in human T-cell development severely affect distribution and maturation of thymic stromal cells: possible implications for the pathophysiology of Omenn syndrome. Clinical and immunologic consequences of a somatic reversion in a patient with Xlinked severe combined immunodeficiency. Felgentreff K, Perez-Becker R, Speckmann C, Schwarz K, Kalwak K, Markelj G, et al. Clinical and immunological manifestations of patients with atypical severe combined immunodeficiency. Human syndromes of immunodeficiency and dysregulation are characterized by distinct defects in T-cell receptor repertoire development. Optimizing outcomes of hematopoietic stem cell transplantation for severe combined immunodeficiency. Respiratory syncytial virus infection in patients with hematological diseases: single-center study and review of the literature. Hematopoietic stem cell gene therapy for adenosine deaminase-deficient severe combined immunodeficiency leads to long-term immunological recovery and metabolic correction. Hematopoietic stem cell transplantation for severe combined immunodeficiency in the neonatal period leads to superior thymic output and improved survival. Hematopoietic stem-cell transplantation for the treatment of severe combined immunodeficiency. High-definition mapping of retroviral integration sites identifies active regulatory elements in human multipotent hematopoietic progenitors. Purine nucleoside phosphorylase deficiency presenting as severe combined immune deficiency. Pachlopnik Schmid J, Lemoine R, Nehme N, Cormier-Daire V, Revy P, Debeurme F, et al. Reversible severe combined immunodeficiency phenotype secondary to a mutation of the proton-coupled folate transporter. Granulocyte colony-stimulating factor: key (f)actor or innocent bystander in the development of secondary myeloid malignancy? Martinez Ibanez V, Espanol T, Matamoros N, Iglesias J, Allende H, Lucaya T, et al. Relapse of sclerosing cholangitis after liver transplant in patients with hyper-Ig M syndrome. A large kindred with X-linked neutropenia with an I294T mutation of the Wiskott-Aldrich syndrome gene. Advances in our understanding of the molecular basis of disorders of platelet function. Wiskott-Aldrich syndrome: diagnosis, clinical and laboratory manifestations, and treatment. Long-term outcome following hematopoietic stem-cell transplantation in Wiskott-Aldrich syndrome: collaborative study of the European Society for Immunodeficiencies and European Group for Blood and Marrow Transplantation. Long-term outcome and lineage-specific chimerism in 194 patients with Wiskott-Aldrich syndrome treated by hematopoietic cell transplantation in the period 1980-2009: an international collaborative study. The cellular ataxia telangiectasia-mutated kinase promotes Epstein-Barr virus lytic reactivation in response to multiple different types of lytic reactivation-inducing stimuli. Autopsy study of cerebellar degeneration in siblings with ataxia-telangiectasia-like disorder. Hematopoietic stem cell transplantation corrects the immunologic abnormalities associated with immunodeficiency-centromeric instability-facial dysmorphism syndrome. Promising therapy results for lymphoid malignancies in children with chromosomal breakage syndromes (Ataxia teleangiectasia or Nijmegen-breakage syndrome): a retrospective survey. The dynamics of T-cell receptor repertoire diversity following thymus transplantation for DiGeorge anomaly. The cutaneous manifestations of atypical complete DiGeorge syndrome: a histopathologic and immunohistochemical study. Autoimmunity in a cohort of 130 pediatric patients with partial DiGeorge syndrome. Cervera C, Fernandez-Aviles F, de la Calle-Martin O, Bosch X, Rovira M, Plana M, et al. Molecular assessment of thymic capacities in patients with Schimke immuno-osseous dysplasia. Marked variability in the radiographic features of cartilage-hair hypoplasia: case report and review of the literature. Hypoplastic anemia in cartilage-hair hypoplasia-balancing between iron overload and chelation. Reduced thymic output, cell cycle abnormalities, and increased apoptosis of T lymphocytes in patients with cartilage-hair hypoplasia. Fatal adult-onset antibody deficiency syndrome in a patient with cartilage hair hypoplasia. Clinical and immunologic outcome of patients with cartilage hair hypoplasia after hematopoietic stem cell transplantation. Diagnostic approach to the hyper-IgE syndromes: immunologic and clinical key findings to differentiate hyper-IgE syndromes from atopic dermatitis. Intermediate phenotypes in patients with autosomal dominant hyper-IgE syndrome caused by somatic mosaicism. Severe eczema and Hyper-IgE in Loeys-Dietz-syndrome-contribution to new findings of immune dysregulation in connective tissue disorders. Loss of desmoglein 1 associated with palmoplantar keratoderma, dermatitis and multiple allergies. Desmoglein 1 deficiency results in severe dermatitis, multiple allergies and metabolic wasting. Diffuse large Bcell lymphoma in a patient with hyper-IgE syndrome: Successful treatment with risk-adapted rituximab-based immunochemotherapy. Eczematous dermatitis in the setting of hyper-IgE syndrome successfully treated with omalizumab. Role of omalizumab in a patient with hyper-IgE syndrome and review dermatologic manifestations. Curative treatment of autosomal-recessive hyper-IgE syndrome by hematopoietic cell transplantation. Successful engraftment of donor marrow after allogeneic hematopoietic cell transplantation in autosomal-recessive hyper-IgE syndrome caused by dedicator of cytokinesis 8 deficiency. Goussetis E, Peristeri I, Kitra V, Traeger-Synodinos J, Theodosaki M, Psarra K, et al. Successful long-term immunologic reconstitution by allogeneic hematopoietic stem cell transplantation cures patients with autosomal dominant hyper-IgE syndrome. Dyskeratosis congenita: a combined immunodeficiency with broad clinical spectrum-a single-center pediatric experience. Update on transcobalamin deficiency: clinical presentation, treatment and outcome. Impact of folate therapy on combined immunodeficiency secondary to hereditary folate malabsorption. Mutations in tetratricopeptide repeat domain 7A result in a severe form of very early onset inflammatory bowel disease. Clinical characteristics and genotype-phenotype correlation in 62 patients with X-linked agammaglobulinemia. Pyoderma gangrenosum-like ulcer in a patient with X-linked agammaglobulinemia: identification of Helicobacter bilis by mass spectrometry analysis. Bacteremia caused by a novel helicobacter species in a 28-year-old man with Xlinked agammaglobulinemia. Successful approach to treatment of Helicobacter bilis infection in X-linked agammaglobulinemia. Campylobacter jejuni bacteremia and Helicobacter pylori in a patient with X-linked agammaglobulinemia. Search for poliovirus long-term excretors among patients affected by agammaglobulinemia.
B12 (Vitamin B12). Venlor.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96890