




|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Linda Cardozo MD FRCOG
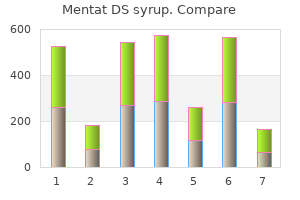
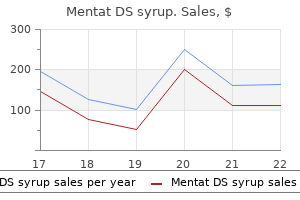
The previously discussed protocols for detoxifica tion from all substances of abuse appear ade Physical Detoxification Services for Withdrawal From Specific Substances tion to alcohol ingestion can include nausea treatment norovirus purchase 100 ml mentat ds syrup overnight delivery, dizziness 97140 treatment code generic mentat ds syrup 100 ml free shipping, headache medicine numbers mentat ds syrup 100ml cheap, fast heartbeat medicine technology generic mentat ds syrup 100 ml on line, and anx iety (Caetano et al medications 24 purchase mentat ds syrup 100 ml without prescription. Chinese patients seem to require lower doses of codeine medicine the 1975 cheap mentat ds syrup 100 ml online, since the slower metabolism leads to a higher concen tration of codeine in the blood (Smith and Lin 1996). This may result in the need for lower doses, since they report greater sedative effects with a typical dose (Lesser et al. It also may be that a lower body fat, which is typical of AsianAmerican individuals, can lead to differences in the pharmacokinetics of lipophilic drugs (Lesser et al. In contrast, Asians may metabolize phenelzine faster, resulting in the need for a higher dose relative to that which would be appropriate for Caucasians (Pi and Gray 1999). Thus, they may need to smoke less frequently and take in less nicotine to achieve the same nicotine levels as do Hispanics/Latinos and Caucasians. American Indians There are currently more than 500 federally recognized AmericanIndian tribes, and there is among them great variability in appear ance, dress, values, religious beliefs, prac tices, and traditions. Of all ethnic and racial groups, American Indians have the greatest rates of alcohol and illicit drug use (Office of Applied Studies 2002a). An early study of treatment utilization by American Indians found that there was a sig nificant association between involvement in society and treatment outcomes. Those involved in either the traditional Indian soci ety or both the traditional Indian society and Caucasian society had more than a 70 percent success rate, whereas those involved in nei ther society had a 23 percent success rate (Ferguson 1976). At a 10year followup, those who had reported greater Indian culture affil iation and more severe liver dysfunction at baseline had better alcohol treatment out comes (Westermeyer and Neider 1984). When engaging an American Indian in the process of detoxification, moving through the process too quickly or abruptly can be per ceived as showing a lack of caring and is con sidered contrary to trust building (Brems 1998). The pace of conversation is important; a slower pace is more agreeable than a rapid conversation. Moreover, a confrontational approach also is not advised with this popula tion (Abbott 1998). American Indians may want a close and involved relationship with their therapists and often want the clinician to be a friend or relative (Brems 1998). The Talking Circle is a native 116 Chapter 4 tradition that can be helpful in the treatment process (Canino et al. The previously discussed protocols for detoxi fication from all substances of abuse appear adequate for the detoxification of American Indians. For instance, it is important that the treatment staff understand the role of the family. The functional family can be extended and should take into account people who have daytoday contact with and a role in the family (Markarian and Franklin 1998). Hispanics/Latinos are likely to view drug dependency as moral failing or personal weakness. The previ Hispanics/Latinos ously discussed pro tocols for detoxifica are now the tion from alcohol, opioids, benzodi largest ethnic azepines, stimulants, solvents, nicotine, minority group in marijuana, anabolic steroids, and club America. Language is one of the most difficult barriers to treatment entry and success for Hispanics/Latinos. However, simply knowing Approximately 5 to 33 percent of all les understanding bian and gay individ uals are estimated to substance abuse have a substance abuse problem patterns. A contributing factor may be the stress and anxiety associated with the social stigma attached to homosexuality. Further, alcohol and drugs may serve as an escape and ease social interactions at social settings such as bars. The previously discussed protocols for detoxifica 117 Physical Detoxification Services for Withdrawal From Specific Substances tion appear adequate for gay and lesbian patients. Since numerous misconceptions and stereotypes exist concerning gay and lesbian individuals, it is important for the clinician to assess his beliefs and take care not to impose them on the patient. Incarcerated/Detained Persons Substance use disorders are common among inmate populations. At the time of arrest and detention, it has been estimated that 70 to 80 percent of all inmates in local jails and State and Federal prisons had regular drug use or had committed a drug offense, and 34 to 52 percent of these inmates were intoxicated at the time of their arresting offense (Federal Bureau of Prisons 2000; Mumola 1999). Persons who are incarcerated or detained in holding cells or other locked areas should be screened for physical dependence on alcohol, opioids, and benzodiazepines and provided with needed detoxification and treatment. The duration of detention will affect what detoxification ser vices can be provided, and many facilities will not be able to provide detoxification or con tinuing care services. There are some special considerations for the detoxification of this population: · Abrupt withdrawal from alcohol can be life threatening. Chapter 4 Adolescents the previously discussed protocols for detoxifi cation from all substances of abuse appear ade quate for the detoxification of adolescents; however, there are several additional aspects to consider: · Physical dependence generally is not as severe, and response to detoxification is more rapid than in adults. In one study, among those who reported specific drug use, over 90 percent of their friends reported using the same drug (Dinges and Oetting 1993). Detoxifica tion from steroids does not typically require specific pharmacological intervention unless 118 · Abrupt withdrawal from opioids or benzo diazepines is not lifethreatening but can cause severe withdrawal signs and symp toms and great distress. If the incarcera tion is 30 days or less, the individual should be maintained on her usual dosage. If the incarceration is longer, the individual may be appropriate for gradual dose tapering. Physical Detoxification Services for Withdrawal From Specific Substances 119 5 CoOccurring Medical and Psychiatric Conditions In this Chapter. General Principles of Care for Patients With Co Occurring Medical Conditions Treatment of CoOccurring Psychiatric Conditions Standard of Care for CoOccurring Psychiatric Conditions Patients undergoing detoxification frequently present with medical and psychological conditions that can greatly affect their overall well being and the process of detoxification. These may simply be pre existing medical conditions not related to substance use or the direct outcome of the substance abuse. In either case, the detoxification pro cess can negatively affect the cooccurring disorder or vice versa. Furthermore, people who abuse substances often present with medical conditions in advanced stages or in a medical crisis. Cooccurring mental disorders also are likely to be exacerbated by substance abuse. This chapter is intended primarily for medical personnel treating patients in detoxification settings, though nonmedical staff may find it informative as well. This chapter is not meant to take the place of authoritative sources from internal medicine. Rather, it presents a cursory overview of special conditions, modifications in protocols, and the use of detoxification medications in patients with cooccurring conditions or disorders. Overall treatment of specific conditions is not addressed unless modification of such treatment is needed. In most cases, the management of the medical condition in the patient with a sub stance use disorder diagnosis does not differ from that of any other patient. However, the medication used for detoxification and the actual detoxification protocol may need to be modified to minimize potentially harmful effects relevant to the cooccurring condition. Detoxification staff providing support should be familiar with the signs and symptoms of common cooccurring medical disorders. The setting in which detoxification is carried out should be appropriate for the medical conditions present and should be adequate to provide the degree of monitoring needed to ensure safety. Acute, lifethreatening conditions need to be addressed concurrently with the withdrawal process and intensive care unit monitoring may be indicated. Clinicians should keep in mind that consulta tion with specialists in infectious diseases, cardiology, pulmonary medicine, hematology, neurology, and surgery may be warranted. Attending medical staff should be aware that cooccurring medical conditions present an opportunity to engage patients. By focusing on the adverse effects of the substance abuse 122 on the overall health of patients, staff mem bers are in a position to help patients see the importance of engaging in treatment for their substance use disorders. Patients should have appointments for followup care made prior to detoxification discharge for all chronic medi cal conditions, conditions needing further evaluation, and substance abuse treatment. This section highlights the conditions most frequently seen in individuals who abuse sub stances, though it is not inclusive. Where special considerations are needed for a patient presenting with a given disorder in a detoxification setting they are listed following the heading "Special Considerations. Cocaine use, for example, can result in various gas trointestinal complications, including gastric ulcerations, retroperitoneal fibrosis, visceral infarction, intestinal ischemia, and gastroin testinal tract perforations (Linder et al. Since symptoms can be vague and patients are not always able to articulate the specific problem, diagnosis can be difficult. MalloryWeiss Syndrome MalloryWeiss Syndrome is caused by torn mucosa of the esophagus at the gastro esophageal junction due to protracted or vio lent vomiting. Patients medical conditions presenting with this condition complain of present an acute epigastric pain (83 percent of opportunity to patients), vomiting (79 percent), and shortness of breath engage patients in (39 percent) as the predominant, nonspe treatment for cific symptoms. This lack of specificity can their substance delay making the cor rect diagnosis (Brauer use disorders. Typical symptoms include burning in the epi gastric or retrosternal area (commonly called "heartburn" or "indigestion"). Esophageal bleeding can result from reflux esophagitis and esophageal varices (resulting from portal hypertension). Gastritis Gastritis is described as the disruption of the gastric mucus lining that allows gastric acid to contact the mucosa with resultant inflammation and possible bleeding. Alcohol increases gastric acid secretion and reduces the mucosal cell barrier, 123 Special considerations Several drugs used in typical protocols, such as beta blockers and calcium channel blockers, CoOccurring Medical and Psychiatric Conditions allowing backdiffusion of the gastric acid into the mucosa. This frequently causes an occur rence of erosive gastritis in the individual with an alcohol use disorder (Fenster 1982). Special considerations Aspirin and nonsteroidal medications should be avoided in the withdrawal protocols. Liver disorders Liver disease can range from fairly benign fatty liver, which presents usually as an asymptomatic enlargement of the liver associ ated with mild elevation of the serum liver enzymes, to a broad spectrum of viral infec tions and the toxic consequences of alcohol and other drug use. The presentation is one of liver tenderness, jaundice, fever, ascites, and an enlarged liver. Pancreatitis Pancreatitis can be caused by many fac tors, although stud Detoxification ies suggest that alco hol may be a factor staff providing in anywhere from 5 to 90 percent of all support should be cases (Apte et al. The acute condition pre mon cooccurring sents with abdomi nal pain, which is medical conditions. Presenting symptoms and signs can include abdominal tenderness, decreased bowel sounds, lowgrade fever, tachycardia, nausea, and vomiting. Pancreatitis can proceed to a chronic condition where pancreatic calcifica tion, diabetes mellitus, malabsorption, and chronic abdominal pain occur. Special considerations Alcoholic hepatitis usually needs acute medi cal treatment to prevent electrolyte imbalance and dehydration. Portal hypertension Portal hypertension is a frequent conse quence of liver disease. If elevation of the portal pressure goes untreated, esophageal varices develop and hemorrhage can ensue. Initial therapy should include prompt and adequate intravascular volume replacement, correction of severe anemia and coagulopathies, and adequate airway management. Special considerations Propranolol or isosorbide therapy is effective in the prophylaxis of variceal bleeding (Trevillyan and Carroll 1997), though beta blockers can interfere with measuring the true heart rate that determines the content of many detoxification protocols. If bleeding is Special considerations There may be a need to forbid oral intake of food and medications, necessitating a change of route of administration of both food and medications to intravenous forms. In alcohol withdrawal protocols, Ativan might be consid 124 Chapter 5 present, changeover to intravenous medica tion protocols is recommended, as the patient will not be able to take oral medications. Cardiovascular Disorders the presentation of chest pain or discomfort remains one of the most difficult differential diagnoses to sort through, as disorders of sev eral systems can cause this single complaint. A normal resting electrocardiogram does not rule out the presence of organic heart disease and the presence of nonspecific changes does not necessarily mean that heart disease is pre sent. Final diagnoses can range from reflux to myocardial infarction brought about by underlying ischemic heart disease or the use of cocaine. The consensus panel believes that this condi tion should never be overlooked or minimized and it is imperative that an especially prompt diagnosis be made and treatment be under taken to ensure patient safety. Underlying cardiac illness could be worsened by the presence of autonomic arousal (elevat ed blood pressure, increased pulse and sweat ing) as seen in alcohol, sedative, and opioid withdrawal. Thus prompt attention to these findings and aggressive withdrawal treatment is indicated. Special considerations for the treatment of specific cardiac conditions are outlined below. Cirrhosis Cirrhosis, or the formation of fibrous tissue in the liver, leads to a state of increased resis tance in the hepatic venous circulation. The inability of blood to flow freely gives rise to portal hypertension with ensuing esophageal varices, splenomegaly, ascites, dilatation of superficial veins, peripheral edema, and hem orrhoids. Liver necrosis can be seen in patients who use inhalants, particularly chronic use of benzene and carbon tetrachloride. African Americans and Hispanics/Latinos have higher mortality rates from cirrhosis of the liver resulting from alcohol abuse than do Caucasians and Asians and Pacific Islanders (Sutocky et al. Liver function test abnormality and jaundice can occur in individuals who use anabolic steroids, but this usually resolves on cessation of the drugs. Studies in the elderly show that 1year mortality was 50 percent among patients over age 60 with cirrhosis, versus 7 percent for those under age 60 (Potter and James 1987). Great care needs to be used when giving diuretics to elderly patients with cirrhosis, since their total body water may already be decreased, making them more sus ceptible to fluid and electrolyte depletion (Scott 1989). Alcoholrelated hepatic injury is seen in a higher proportion of women due to a possible potentiation (strengthening) of this effect by estrogen (Brady and Randall 1999). Evaluation should include a complete history to determine if the elevated blood pressure predated the present with drawal status. Propranolol (Inderal), labetalol (Trandate) and metoprolol (Lopressor) are the beta blockers of choice for treating hypertension during pregnancy (McElhatton 2001), howev er, the impact of using them for alcohol detoxification during pregnancy is unclear.
The subgroups met and began delibera tions related to the guidelines in their respective topic areas treatment 6th february buy generic mentat ds syrup 100ml. Effective tools and practical strategies for primary care set tings were considered medications requiring central line mentat ds syrup 100ml amex. This approach was considered optimal because a number of structures of the brain are affected versus a single medicine guide generic mentat ds syrup 100ml otc, isolated structure treatment urticaria purchase 100ml mentat ds syrup otc. This generalized nature of damage from prenatal alcohol exposure can result in a wide array of neurodevelopmental outcomes bad medicine discount 100ml mentat ds syrup free shipping. In addition medicine hat horse mentat ds syrup 100 ml on-line, the clinicians were also asked to identify three to five specific behaviors that could be used as examples of each of the five areas of deficit. Each domain is presented so as to include exem plars from direct observation or parent report that can be documented through standardized test ing. Medical diagnostic criteria are generally evaluated in two ways: (1) the criteria must be reliable and; (2) the criteria must be as valid as possible. The criteria that appear in these diagnostic guidelines meet both of these requirements. The framework was developed to provide an overview of the entire identification, referral, diagnosis, and treatment process. Initial recognition that a child or older individual has a potential problem can come from many sources. School systems, including Head Start and daycare staff, interact with a large number of children and often recognize when someone is having difficulty. It is assumed that triggers, such as facial abnormalities, growth delay, develop mental problems, or maternal alcohol use, will emerge from the contact. Recognition of a potential problem should lead the provider, regardless of specific profession, to facilitate getting the person and his or her family to the appropriate next step. The referral process is initiated at the point a clinician starts to have suspicions of an alcohol-related disorder for a child. Examples of triggers are presented later, in the Referral section of these guidelines. These data will assist the provider in making the decision to diagnose the child or to refer the child to a multidisci plinary evaluation team for a confirmed diagnosis. In addition, these data could be forwarded to the multidisciplinary evaluation team to guide the diagnostic process. Once a diagnosis is made, an intervention plan would be developed using a multidisciplinary team approach. A variety of specialists could contribute to the multidisciplinary team, including dysmor phologists, developmental pediatricians, psychiatrists, psychologists, social workers, and educational specialists. In many rural and less populated regions, these clinicians must make the diagnosis for many types of birth defects and developmental 8 Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis disabilities. Many of these evaluation services are available within the community setting, for exam ple school systems could provide neurocognitive assessments. Human congenital malformations are referred to as dysmorphic features or dysmor phia (55). Dysmorphia occurs when normal morphogenesis is interrupted, creating a particular fea ture which is shaped, sized, or positioned outside the normal range of development. Alcohol is a teratogen that results in dysmorphia through interference with nerve cell development and func tioning, alterations in the ability of cells to grow and survive, increased formation of cell-damaging free radicals, altered pathways of biochemical signals within cells, and altered expression of certain genes and genetic information. In short, alcohol has been shown to interfere with fetal nerve cell development and function in a variety of ways (56-57). However, other features also were noted for some patients, including altered palmar fexional crease patterns. Over the next 30 years, additional features described included: micro cephaly, short nose, smooth philtrum with thin vermillion border, cleft lip, micrognathia, protrud ing auricles, short or webbed neck, vertebra and rib anomalies, short metacarpal bones, menigomyelocele, hydrocephalus, and hypoplastic labia majora (43). Despite the heterogeneity of expression for dysmorphic features related to prenatal exposure to alco hol, core facial dysmorphia have emerged through human and animal studies. Using anthropomorphic measurements of all facial features, clinical researchers have confirmed the midline feature abnormalities (59). Cross-sectional and longitudinal studies indicate that many features can change with age or development. For example, the 1999 version of University of Washington 4-digit code system uses the same philtrum and vermillion border criteria (as noted by reference to its Lip-Philtrum Guide), but uses a cutoff of the 3rd percentile (2 or more standard deviations below the norm) for palpebral fissures, which is a more conservative cutoff (50). Thus, the checklists tend to be more inclusive than the current guidelines, with greater potential for false-positive diagnoses. Even rare defects or certain clusters of dysmorphic features can appear in a variety of syndromes. As can be seen from Table 1, none of the syndromes with single overlapping features (except for Toluene embryopathy) have the full constellation of small palpebral fissures, thin vermillion border, and smooth philtrum. These syndromes should be considered in particular when completing the differential diagnosis. Table 2 lists these syndromes, along with the overlapping and differentiating features. Thus, children with growth retarda 10 Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis Table 1. As noted previously in the dys morphia section, use of the 10th percentile strikes a balance among criteria used in other diagnostic systems. Again, the 1999 edition of the University of Washington 4-digit code takes a conservative approach, using the 3rd percentile as the cutoff. Checklist systems often do not specify a particular level of growth retardation and some do not specify which growth parameters should be considered. Wide mouth with full lips, stellate pattern of the iris, periorbital fullness, and connective tissue disor ders. The primary issue that emerged in the discussion of timing of growth retardation was whether growth retardation needs to be present at the time of the diagnosis, or whether it could have occurred previously and been resolved. This is particularly important when including prenatal growth retardation or early growth problems due to failure to thrive. The committee noted that the examin er should make sure that the single point in time when the growth deficit was present does not cor relate with a point in time when the child was nutritionally deprived. Growth retardation and growth deficiencies occur in chil dren, adolescents, and adults for a great many reasons. This could be a particular problem for infants with poor sucking responses who experience failure to thrive. Prenatal growth retardation can be due to a variety of factors, including maternal smoking or other behaviors leading to hypoxia, poor maternal nutrition, or genetic disorders. Clinically significant brain abnormalities observable through imaging techniques. Early brain damage is usually generalized rather than specific, with increased specificity of abnormalities revealed as development progresses. The functional abilities affected by prenatal exposure to alcohol vary greatly from person to person, depending on the amount of alcohol exposure, timing of exposure, and pattern of exposure. Despite this inherent variation in effects, several areas of significant functional vul nerability have been observed consistently by clinicians and clinical researchers with particular damage to corresponding structures reported. Variability in exposure impact results in variability of structural, neurological, or function al deficits, or a combination thereof in affected individuals. For functional deficits, it is generally accepted that multiple locations in the brain (and correspon ding functional capability) are affected by prenatal exposure to alcohol. Decreased per formance on a standardized measure of cognition/intelligence or development assumes deficits in multiple domains. In the absence of such a measure, several specific domains need to be assessed individually to determine that multiple functional domains have been affected. It should 14 Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis be noted that for each of the following specific domains described, other agents and environmental factors can produce deficits or outcomes similar to prenatal alcohol exposure, making care differen tial diagnosis essential. Finally, these descriptions are intended to be suggestive and examples of likely and possible problems a clinician might encounter then need to assess using psychometric instruments. The exemplars are not intended to be exhaustive, or to present a necessary list of behaviors to be used as a checklist without reliable and valid assessment. It is important to note that global deficits or delays can leave the child scoring in the normal range of development, but below what would be expected for his or her environment and background (61,95-99). In addition to formal testing (either through records or current testing), behaviors that may be observed (or reported) in the clinical setting that suggest cognitive deficits or developmental delays that should be assessed by standardized testing include but are not limited to specific learning disabilities (espe cially math and/or visual-spatial deficits); uneven profile of cognitive skills; poor academic achievement; discrepancy between verbal and nonverbal skills; and slowed movements or reac tion to people and stimuli. Visual-motor/visual-spatial coordination is a particularly vulner able area of functioning (99,112-113). Behaviors that can be seen (or reported) in the clinical set ting that indicate motor problems that should be assessed by standardized testing include, but are not limited to delayed motor milestones; difficulty with writing or drawing; clumsiness; bal ance problems; tremors; and poor dexterity. Behaviors that can be observed (or reported) in the clinical setting that indicate these types of social difficulties that should be assessed by standardized testing include, but are not limited to lack of stranger fear; often scape-goated; naivetй and gullibility; easily taken advantage of; inappropriate choice of friends; preferring younger friends; immaturity; superfi cial interactions; adaptive skills significantly below cognitive potential; inappropriate sexual behaviors; difficulty understanding the perspective of others; poor social cognition; and clini cally significant inappropriate initiations or interactions. Social functioning is a multifac eted domain that can require several areas of assessment. In addition to these five most often cited prob lem areas, deficits and problems to be assessed by standardized testing can present in several other areas, including sensory problems. Several statistical thresholds have been suggested to operationally define performance substantially below expected levels. Ideally, functional deficits should be established through appropriate standardized neuropsychologi cal testing by a trained professional. Clinicians are strongly encouraged to supplement their observations by obtaining standardized testing through early intervention programs, public schools, and psychologists in private practice. In addition, such testing will facilitate the development of individualized and appropriate treatment plans for diagnosed individ uals. The 1999 version of the University of Washington 4-digit code and the guidelines developed by Health Canada requires performance below the 3rd percentile (2 standard deviations below the mean on standardized test ing) in three separate domains in which global deficits count as one domain. Some health systems might find this approach useful in situations in which resources for standardized testing are readily available. Commonly co-occurring mental health issues (excluding attention problems) reported by clinicians and cited in the scientific literature to date, include conduct disorders, oppositional defiant disorders, anxiety disorders, adjustment disorders, sleep disorders, and depression (81,95,131134). There are considerable animal, human, and clinical studies that document attention deficits for many individuals with prenatal exposure to alcohol (117). In addition, decreased adaptive skills and increased problems with daily living abili ties have been consistently documented, although further research is needed. Such problems include dependent living conditions, disrupted school experiences, poor employment records and encounters with law enforcement (including incarceration; 95). It is important to determine that the observed functional deficits are not better explained by other causes. In addition to other organic syndromes that produce deficits in one or more of the previously cited domains. Documentation and confirmation of prenatal alcohol exposure can be extremely challenging. For birth mothers, admission of alcohol use during pregnancy can be very stigmatizing. The situation can be further complicated if the woman is still using alcohol, especially at high consumption rates. In this situation, information about alcohol use might need to be obtained from other reliable informants, such as a relative. It must be noted that simple denials of alcohol use might or might not be credible and corroborating evidence should be obtained whenever possible. Confirmed prenatal alcohol exposure requires documentation of the alcohol consumption patterns of the birth mother during the index pregnancy based on clinical observation; selfreport; reports of heavy alcohol use during pregnancy by a reliable informant; medical records documenting positive blood alcohol levels, or alcohol treatment; or other social, legal, or medical problems related to drinking during the index pregnancy. Unknown prenatal alcohol exposure indicates that there is neither a confirmed presence nor a confirmed absence of exposure. Examples include: the child is adopted and prenatal exposure(s) is unknown; the birth mother is an alcoholic, but confirmed evidence of exposure during pregnancy does not exist; and conflicting reports about exposure exist that cannot be reliably resolved. It should be noted that confirmed prenatal alcohol use can strengthen the evidence for diagnosis, but is not necessary in the presence of all the previous findings. As would be expected for any congenital syn drome, presentation of the diagnostic features can change over development. With regards to facial features (small palpebral fissures, smooth philtrum, and thin vermillion border), it has generally been accepted that these features are most evident during infancy and the early preschool years. However, longitudinal data that specifically address this issue are not available currently. One also might expect growth parameters to change (and generally normalize) with development. This might especially be the case for children who receive nutritional or other interventions. While structural abnormalities would remain consistent, neurological and functional deficits could resolve or change presentation at various stages of development. During the newborn and infancy periods, difficulty with arousal or behavior regulation might be observed. For example, simple planning or organization skills are learned, as well as understanding the physical and mental perspective of others. During adolescence and through adulthood, the pattern of deficits continues to be present and in addition, lifelong conse 19 Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis Table 3: Brief Outline of Diagnostic criteria for Fetal Alcohol Syndrome Facial dysmorphia Based on racial norms, individual exhibits all three characteristic facial features: · Smooth philtrum (University of Washington Lip-Philtrum Guide rank 4 or 5) · Thin vermillion border (University of Washington Lip-Philtrum Guide rank 4 or 5) · Small palpebral fissures (at or below 10th percentile) Growth problems Confirmed prenatal or postnatal height or weight, or both, at or below the 10th percentile, documented at any one point in time (adjusted for age, sex, gestational age, and race or ethnici ty). As future data and science are avail able, these guidelines can be refined and expanded to delineate other conditions resulting from pre natal alcohol exposure. For biological families, there may be social stigma associated with any evaluation concerning prenatal alcohol exposure. In other families, direct information about alcohol use during pregnancy may not be available or only sus pected. Thus, the following guidelines were developed to provide assistance in making the referral decision, although, it is recognized that each case must be evaluated individually. Further, these guidelines were developed with the idea that when in doubt, it was preferable to refer for full evalu ation by a multidisciplinary team with experience in evaluating prenatal alcohol exposure.
The differential diagnosis of sleep-wake complaints necessitates a multidimensional approach symptoms testicular cancer buy 100ml mentat ds syrup amex, with consideration of possibly coexisting medical and neurological conditions medications management buy 100ml mentat ds syrup fast delivery. Sleep disturbances furnish a clinically useful indicator of medical and neurological conditions that often coexist with depression and other common mental disorders treatment 5th metatarsal fracture buy mentat ds syrup 100ml cheap. Prominent among these comorbidities are breathing-related sleep disorders 340b medications generic mentat ds syrup 100 ml on line, disorders of the heart and lungs medications in checked baggage order mentat ds syrup 100 ml free shipping. These disorders not only may disturb sleep but also may themselves be worsened during sleep symptoms appendicitis buy mentat ds syrup 100 ml with visa. The weight of available evidence supports the superior performance characteristics (interrater reliability, as well as convergent, discriminant, and face validity) of simpler, lessdifferentiated approaches to diagnosis of sleep-wake disorders. Insomnia Disorder Diagnostic Criteria with one (or more) of the following symptoms: 1. Difficulty maintaining sleep, characterized by frequent awakenings or problems re turning to sleep after awakenings. The sleep disturbance causes clinically significant distress or impairment in social, oc cupational, educational, academic, behavioral, or other important areas of functioning. The insomnia is not better explained by and does not occur exclusively during the course of another sleep-wake disorder. Coexisting mental disorders and medical conditions do not adequately explain the pre dominant complaint of insomnia. Specify if: With non-sleep disorder mental comorbidity, including substance use disorders With other medical com orbidity With other sleep disorder Coding note: the code 780. A predominant complaint of dissatisfaction witli sleep quantity or quality, associated relevant associated mental disorder, medical condition, or other sleep disorder imme diately after the code for insomnia disorder in order to indicate the association. The diagnosis of insomnia disorder is given whether it occurs as an independent condition or is comorbid with another mental disorder. For instance, insomnia may develop its own course with some anxiety and depres sive features but in the absence of criteria being met for any one mental disorder. Insomnia may also manifest as a clinical feature of a more predominant mental disorder. Persistent insomnia may even be a risk factor for depression and is a common residual symptom af ter treatment for this condition. With comorbid insomnia and a mental disorder, treatment may also need to target both conditions. Given these different courses, it is often impossi ble to establish the precise nature of the relationship between these clinical entities, and this relationship may change over time. Therefore, in the presence of insomnia and a co morbid disorder, it is not necessary to make a causal attribution between the two condi tions. Rather, the diagnosis of insomnia disorder is made with concurrent specification of the clinically comorbid conditions. A concurrent insomnia diagnosis should only be con sidered when the insomnia is sufficiently severe to warrant independent clinical attention; otherwise, no separate diagnosis is necessary. Diagnostic Features the essential feature of insomnia disorder is dissatisfaction with sleep quantity or quality with complaints of difficulty initiating or maintaining sleep. The sleep complaints are ac companied by clinically significant distress or impairment in social, occupational, or other important areas of functioning. The sleep disturbance may occur during the course of an other mental disorder or medical condition, or it may occur independently. Different manifestations of insomnia can occur at different times of the sleep period. Sleeponset insomnia (or initial insomnia) involves difficulty initiating sleep at bedtime. Sleep mainte nance insomnia (or middle insomnia) involves frequent or prolonged awakenings throughout the night. Late insomnia involves early-morning awakening with an inability to return to sleep. Difficulty maintaining sleep is the most common single symptom of insomnia, followed by difficulty falling asleep, while a combination of these symptoms is the most common presen tation overall. Individuals who complain of difficulty falling asleep at one time may later complain of difficulty maintaining sleep, and vice versa. Nonrestorative sleep, a complaint of poor sleep quality that does not leave the individual rested upon awakening despite adequate duration, is a common sleep complaint usually occurring in association with difficulty initiating or maintaining sleep, or less frequently in isolation. Aside from the frequency and duration criteria required to make the diagnosis, addi tional criteria are useful to quantify insomnia severity. These quantitative criteria, while arbitrary, are provided for illustrative purpose only. For instance, difficulty initiating sleep is defined by a subjective sleep latency greater than 20-30 minutes, and difficulty maintain ing sleep is defined by a subjective time awake after sleep onset greater than 20-30 min utes. Although there is no standard definition of early-morning awakening, this symptom involves awakening at least 30 minutes before the scheduled time and before total sleep time reaches hours. It is essential to take into account not only the final awakening time but also the bedtime on the previous evening. Such a symptom may also reflect an age-dependent decrease in the ability to sus tain sleep or an age-dependent shift in the timing of the main sleep period. Insomnia disorder involves daytime impairments as well as nighttime sleep difficulties. These include fatigue or, less commonly, daytime sleepiness; the latter is more common among older individuals and when insomnia is comorbid with another medical condition. Impairment in cognitive performance may include difficulties with attention, concentration and memory, and even with performing simple manual skills. Associated mood disturbances are typically described as irritability or mood lability and less commonly as depressive or anxiety symptoms. Not all individuals with nighttime sleep disturbances are distressed or have functional impairment. For example, sleep continuity is often interrupted in healthy older adults who nevertheless identify themselves as good sleepers. A diagnosis of insomnia disorder should be reserved for those individuals with significant daytime distress or impairment related to their nighttime sleep difficulties. Associated Features Supporting Diagnosis Insomnia is often associated with physiological and cognitive arousal and conditioning factors that interfere with sleep. A preoccupation with sleep and distress due to the inabil ity to sleep may lead to a vicious cycle: the more the individual strives to sleep, the more frustration builds and further impairs sleep. Thus, excessive attention and efforts to sleep, which override normal sleep-onset mechanisms, may contribute to the development of in somnia. Individuals with persistent insomnia may also acquire maladaptive sleep habits. Engaging in such activities in an environment in which the individual has frequently spent sleepless nights may further compound the con ditioned arousal and perpetuate sleep difficulties. Some individuals also report better sleep when away from their own bedrooms and their usual routines. Insomnia may be accompanied by a variety of daytime complaints and symptoms, in cluding fatigue, decreased energy, and mood disturbances. Symptoms of anxiety or de pression that do not meet criteria for a specific mental disorder may be present, as well as an excessive focus on the perceived effects of sleep loss on daytime functioning. Individuals with insomnia may have elevated scores on self-report psychological or personality inventories with profiles indicating mild depression and anxiety, a worrisome cognitive style, an emotion-focused and internalizing style of conflict resolution, and a so matic focus. Patterns of neurocognitive impairment among individuals with insomnia dis order are inconsistent, although there may be impairments in performing tasks of higher complexity and those requiring frequent changes in performance strategy. Individuals with insomnia often require more effort to maintain cognitive performance. Prevalence Population-based estimates indicate that about one-third of adults report insomnia symp toms, 10%-15% experience associated daytime impairments, and 6% -10% have symptoms that meet criteria for insonmia disorder. Insomnia is a more prevalent complaint among fe males than among males, with a gender ratio of about 1. Although insomnia can be a symptom or an independent disorder, it is most frequently observed as a comorbid con dition with another medical condition or mental disorder. For instance, 40%-50% of indi viduals with insomnia also present with a comorbid mental disorder. Development and Course the onset of insomnia symptoms can occur at any time during life, but the first episode is more common in young adulthood. In women, new-onset insomnia may occur during menopause and persist even after other symptoms. Insomnia may have a late-life onset, which is often associated with the onset of other health-related conditions. Situational or acute insomnia usu ally lasts a few days or a few weeks and is often associated with life events or rapid changes in sleep schedules or environment. For some individuals, perhaps those more vulnerable to sleep disturbances, in somnia may persist long after the initial triggering event, possibly because of conditioning factors and heightened arousal. For example, an individual who is bedridden with a painful injury and has difficulty sleeping may then develop negative associations for sleep. A similar course may develop in the context of an acute psychological stress or a mental disorder. For instance, insomnia that occurs during an episode of major depressive disorder can become a focus of attention, with consequent negative conditioning, and persist even after resolution of the depressive episode. In some cases, insomnia may also have an insidious onset without any identifi able precipitating factor. The course of insomnia may also be episodic, with recurrent episodes of sleep difficul ties associated with the occurrence of stressful events. Many individuals with insomnia have a history of "light" or easily disturbed sleep prior to onset of more persistent sleep problems. The type of insomnia symptom changes as a function of age, with difficulties initiating sleep being more common among young adults and problems maintaining sleep occurring more fre quently among middle-age and older individuals. Difficulties initiating and maintaining sleep can also occur in children and adolescents, but there are more limited data on prevalence, risk factors, and comorbidity during these developmental phases of the lifespan. Insomnia in adolescence is often triggered or exacerbated by irregular sleep sched ules. In both children and adolescents, psychological and medical fac tors can contribute to insomnia. The increased prevalence of insomnia in older adults is partly explained by the higher incidence of physical health problems with aging. Changes in sleep patterns associated with the normal developmental process must be differentiated from those exceeding age-related changes. Although polysomnography is of limited value in the routine evaluation of in somnia, it may be more useful in the differential diagnosis among older adults because the etiologies of insomnia. Risk and Prognostic Factors While the risk and prognostic factors discussed in this section increase vuhierability to in somnia, sleep disturbances are more likely to occur when predisposed individuals are ex posed to precipitating events, such as major life events. Most individuals resume normal sleep patterns after the initial triggering event has disappeared, but others-perhaps those more vulnerable to insomnia-continue experiencing persistent sleep difficulties. Perpetuating factors such as poor sleep habits, irregular sleep scheduling, and the fear of not sleeping feed into the in somnia problem and may contribute to a vicious cycle that may induce persistent insomnia. Anxiety or worry-prone personality or cognitive styles, increased arousal predisposition, and tendency to repress emotions can increase vulnerability to insomnia. Noise, light, uncomfortably high or low temperature, and high altitude may also increase vulnerability to insomnia. Female gender and advancing age are associated with in creased vulnerability to insomnia. The prevalence of insomnia is higher among monozygotic twins relative to dizygotic twins; it is also higher in first-degree family members compared with the general population. The extent to which this link is inherited through a genetic predisposition, learned by observations of parental models, or established as a by-product of another psy chopathology remains undetermined. Gender-Reiated Diagnostic issues Insomnia is a more prevalent complaint among females than among males, with first onset often associated with the birth of a new child or with menopause. Despite higher preva lence among older females, polysomnographic studies suggest better preservation of sleep continuity and slow-wave sleep in older females than in older males. Diagnostic iVlaricers Polysomnography usually shows impairments of sleep continuity. Quantitative electroencephalographic analyses may indicate that individuals with insom nia have greater high-frequency electroencephalography power relative to good sleepers both around the sleep onset period and during non-rapid eye movement sleep, a feature suggestive of increased cortical arousal. Individuals with insomnia disorder may have a lower sleep propensity and typically do not show increased daytime sleepiness on objec tive sleep laboratory measures compared with individuals without sleep disorders. Other laboratory measures show evidence, although not consistently, of increased arousal and a generalized activation of the hypothalamic-pituitary-adrenal axis. In general, findings are consistent with the hypothesis that increased physiological and cognitive arousal plays a significant role in insomnia disorder. Individuals with insomnia disorder may appear either fatigued or haggard or, con versely, overaroused and "wired. There may be an increased incidence of stress- related psychophysiological symptoms. Functional Consequences of Insomnia Disorder Interpersonal, social, and occupational problems may develop as a result of insomnia or excessive concern with sleep, increased daytime irritability, and poor concentration. De creased attention and concentration are common and may be related to higher rates of ac cidents observed in insomnia. Persistent insomnia is also associated with long-term consequences, including increased risks of major depressive disorder, hypertension, and myocardial infarction; increased absenteeism and reduced productivity at work; reduced quality of life; and increased economic burden. Some individuals who require little sleep ("short sleepers") may be concerned about their sleep duration. Short sleepers differ from individuals with insomnia disorder by the lack of difficulty falling or staying asleep and by the absence of characteristic daytime symptoms. However, some short sleepers may desire or attempt to sleep for a longer period of time and, by prolonging time in bed, may create an insomnia-like sleep pattern.
Providing infor mation about the common withdrawal symp toms of the specific drugs of abuse may reduce discomfort and the likelihood that the individu al will leave detoxification services prematurely (for a list of withdrawal symptoms medications made from plants mentat ds syrup 100ml discount, see chapter 4) medicine nobel prize buy 100ml mentat ds syrup. Settings that routinely encounter individu als in withdrawal should have written materials available on drug effects and withdrawal from specific drugs medications metabolized by cyp2d6 100 ml mentat ds syrup visa, and have staff who are well versed in the signs and symptoms of withdraw al treatment goals for anxiety buy generic mentat ds syrup 100 ml on line. An additional consideration is providing such information to nonEnglishspeaking patients and their families symptoms 4 dpo order 100ml mentat ds syrup with amex. Interventions that assist the client in identify ing and managing urges to use also may be helpful in retaining the client in detoxification and ensuring initiation of rehabilitation medications 123 buy cheap mentat ds syrup 100ml online. These interventions may include cognitive behavioral approaches that help the individu al identify thoughts or urges to use, the devel opment of an individualized plan to resist these urges, and use of medications such as naltrexone to reduce craving (Anton 1999; Miller and Gold 1994). Considerations for Chronic Relapsers A patient who recently relapsed after a period of extended abstinence may feel especially hopeless and vulnerable (an abstinence viola tion effect). In this situation, clinicians can acknowledge progress that had been made prior to relapse and reassure the patient that the internal gains from past recovery work have not all been lost (despite the feeling at the moment that they have), perhaps reframing the severity of emotional pain as an indicator of how important recovery is to the patient. Strategies for Engaging and Retaining Patients in Detoxification It is essential to keep patients who enter detoxi fication from "falling through the cracks" (Kertesz et al. It is essen tial that all clinicians who have contact with patients in withdrawal continually offer hope and the expectation of recovery. An atmo sphere that conveys comfort, relaxation, clean liness, availability of medical attention, and security is beneficial to patients experiencing the discomforts of the withdrawal process. Throughout the detoxification experience, detoxification staff should be unified in their message that detoxification is only the begin ning of the substance abuse treatment process and that rehabilitation and maintenance activi ties are critical to sustained recovery. Use Support Systems the use of client advocates to intervene with clients wishing to leave early often can be an effective strategy for promoting retention in detoxification. Visitors should be instructed about the importance of supporting the individ ual in both detoxification and substance abuse treatment. If available, and if the patient is sta ble, he or she can attend onsite 12Step or other support group meetings while receiving detoxification services. These activities rein force the need for substance abuse treatment An Overview of Psychosocial and Biomedical Issues During Detoxification 33 and maintenance activities and may provide a critical recoveryoriented support system once detoxification services are completed. Maintain a DrugFree Environment Maintaining a safe and drugfree environment is essential to retaining clients in detoxifica tion. Providers should be alert to drugseek ing behaviors, including bringing alcohol or other drugs into the facility. Visiting areas should be easy for the staff to monitor closely, and staff may want to search visiting areas and other public areas periodically to reduce the opportunities for acquiring substances. It is important to note, however, that personnel should be respectful in their efforts to main tain a drugfree environment. It is important to explain to patients (prior to treatment) and visitors why substances are not allowed in the facility. Use of these techniques in the detoxification setting increases the likelihood that patients will seek treatment by helping them understand the adverse consequences of continued substance use. In addition, the detoxification team can lever age the relationship the patient has with sig nificant others. Although the effectiveness of alter native treatments in detoxification and treat ment has not been validated in wellcontrolled clinical trials, if an alternative therapy brings patients into detoxification and keeps them there, it may have utility beyond whatever spe cific therapeutic value it may have (Trachtenberg 2000). Other treatments that reside outside the Western biomedical system, typically grouped together under the heading of Complementary or Alternative Medicine, also may be useful for retaining patients. Indeed, given the great cultural diversity in the United States, other culturally appropriate practices should be considered. Enhancing Motivation Motivational enhancements are particularly wellsuited to accomplishing the detoxification 34 assist the patient in preparing for change in a nonthreatening, nonconfrontational manner. The consensus panel does not recommend that clinicians use direct confrontation in helping a person with a substance use disor der begin the process of detoxification and subsequent substance abuse treatment. Techniques that involve purposefully con fronting patients about their substance use behavior, such as the Johnson Intervention, where significant others are taught to con front the individuals using substances (Liepman 1993), have been shown to be high ly effective when significant others implement them. However, subsequent studies of clini cians, groups, and programs that rely on con frontational techniques have yielded poor outcomes (Miller et al. Moreover, the vast majority of significant others do not wish to use these techniques, and for that reason these techniques are not recommended (Miller et al. Care should be taken to ensure that any sig nificant other who is involved in motivating the patient for therapy is appropriate for this task. Only significant others who have been appropriately introduced to the intervention by a clinician should participate. The pres ence of a trained facilitator is recommended, either for coaching or for facilitating the intervention. It also is important to have the recommended treatment option readily avail able so if the patient agrees, admission can be swift and seamless. Furthermore, if the patient places consider able value on her or his relationships with these significant others, success is more likely (Longabaugh et al. According to the Clinicians, model, a client is considered to be at groups, and one of five stages of readiness to change programs that his substanceabus ing behavior, each rely on stage being progres sively closer to sus tained recovery. Rather, moti vation to change can be influenced by others, including detoxification treatment staff. In general, the basic concept is to try to move patients to the next stage of change. Tailoring Motivational Intervention to Stage of Change Perhaps the most wellknown and empirically validated model of "readiness to change" that has been applied to substance abuse is the An Overview of Psychosocial and Biomedical Issues During Detoxification 35 Figure 35 the Transtheoretical Model (Stages of Change) Source: DiClemente and Prochaska 1998. In the precontemplation stage, the individual is not considering any change in substance using behavior in the foreseeable future. Typically, a patient in this stage either is unaware that his substance use is a problem or is unwilling or too discouraged to make a change. Often, a person in the precontempla tion stage has not experienced serious conse quences from substance use. During the pre contemplation stage, the clinician should be attentive for and seize upon any ambivalence expressed by the patient toward substance related behaviors. Such ambivalence may be more likely to emerge during initial detoxifi cation, before the patient has returned to a relative zone of comfort and greater denial. For patients who are determined to remain in the precontemplation stage, the main goal is to get the patient to begin to consider chang ing. In the contemplation stage, the individual has some awareness that substance use presents a problem. In this stage, the patient may express a desire or willingness to change, but has no definite plans to do so in the near future, which generally is considered to be the next 2 to 6 months. Whether it is explicit ly stated or not, it is thought that most indi viduals in this stage are ambivalent about changing. That is, sidebyside with any desire to change is a desire to continue the current behavior. For patients in the contem plation stage, clinicians are advised to use "decisional balancing strategies" to help the patient move to the action stage (Carey et al. In this approach, the clinician helps the patient to consider the positive and nega tive aspects of her substance abuse and has the patient weigh them against each other with the expectation that the scale of balance tips in favor of adopting new behavior. Psychoeducation on the interaction of sub stance abuse with other problems, including health, legal, employment, parenting, and mental illness, can be part of this procedure. Helping the patient understand that ambiva lent feelings about changing substance use behaviors are normal and expected can be particularly useful at this stage. In the preparation stage, the patient is aware that his substance use presents a significant problem and desires change. Moreover, the patient has made a conscious decision to com mit himself to a behavior change. This stage is defined as one in which the individual pre pares for the upcoming change in specific ways, such as deciding whether a formal treatment program is needed and, if so, which one. This stage is characterized by goal set ting and making commitments to stop using, such as informing coworkers, friends, and family of treatment plans. It is criti cal that the clinician respond quickly to any requests for treatment to capitalize on this motivation before it wanes. One of the most critically important roles the clinician can play in this stage is to assist the patient in developing a plan of action or a behavioral contract, taking into account the individual needs of the patient. As part of this process the clinician should help the patient enlist social support. Finally, because of the common ly experienced difficulty in accessing treat ment, the clinician should discuss with the patient ways of maintaining motivation for change during a possible wait for entry into a treatment program, should the patient be placed, for example, on a waiting list. In the action stage, the patient is taking active steps to change substance use behav iors. This includes making modifications to his habits and environment, such as not spending time in places or with people associ ated with drug taking behavior. These changes may even continue to be made 3 to 6 months after substance abuse has ceased. In the maintenance stage, the patient is work ing to maintain the changes initiated in the action phase. Fostering a Therapeutic Alliance the therapeutic alliance refers to the quality of the relationship between a patient and his care providers and is the "nonspecific factor" that predicts successful therapy outcomes across a variety of different therapies (Horvath and Luborsky 1993). A therapeutic alliance should be developed in the context of an ability to form an alliance to a group of helping individu als-such as a healthy support network or therapeutic community. A clinically appropri ate relationship between the clinician and patient that is supportive, empathic, and non judgmental is the hallmark of a strong thera peutic alliance. An Overview of Psychosocial and Biomedical Issues During Detoxification 37 Readiness to change predicts a positive thera peutic alliance (Connors et al. Strong alliances, in turn, have been associated with positive outcomes in patients who are depen dent on alcohol (Connors et al. Emphasis also should be given to the alliance with a social support network, which can be a powerful predictor of whether the patient stays in treatment (Luborsky 2000). Given the importance of the therapeutic alliance and the fact that detoxification often is the entry point for patients into substance abuse treatment services, work on establish ing a therapeutic alliance ideally will begin upon admission. Many of the guidelines listed above for enhancing motivation apply to establishing this rapport. Newman (1997) makes some additional recommendations for developing the therapeutic alliance, such as discussing the issue of confidentiality with patients and acknowledging that the road to recovery is difficult. He also advises being consistent, dependable, trustworthy, and available, even when the patient is not. The clinician should remain calm and cool even if the patient becomes noticeably upset. Practitioners should be confident yet humble and should set limits in a respectful manner without engaging in a power struggle. See Figure 36 for a list of characteristics most valuable to a clinician in strengthening the therapeutic alliance. Referrals and Linkages Once an individual passes through the most severe of the withdrawal symptoms and is safe and medically stable, the focus of the psychoso cial interventions shifts toward actively prepar ing her for substance abuse treatment and maintenance activities. Many patients believe that once they have eliminat ed the substance or substances of abuse from their bodies, they have achieved abstinence. Moreover, some insurance policies may not cover treatment, or only offer partial cover age. The patient may have to go through cum bersome channels to determine if treatment is covered, and if so, how much. Preparation should focus on eliminating administrative barriers to entering substance abuse treatment prior to discussing treatment options with the patient. Recovery/Living Environment Due to the limited time patients stay in detoxifi cation settings, it is challenging for programs to conduct a complete assessment of the rehabili tation needs of the individual. With this in mind, detoxification programs should focus on those areas that are essential to make an appropriate linkage to substance abuse treat ment services. The assessment of the psychoso cial needs affecting the rehabilitation process itself may have to be left to the professionals providing substance abuse treatment. The levels of treatment services range from communitybased early intervention groups to medically managed intensive inpa tient services. As noted in chapter 2, providers need to make a placement decision based on six dimensions: 1. Readiness to Change An Overview of Psychosocial and Biomedical Issues During Detoxification Figure 37 Recommended Areas for Assessment To Determine Appropriate Rehabilitation Plans Domain Medical Conditions and Complications Motivation/Readiness to Change Physical, Sensory, or Mobility Limitations Relapse History and Potential Substance Abuse/Dependence Developmental and Cognitive Issues Family and Social Support CoOccurring Psychiatric Disorders Description Infectious illnesses, chronic illnesses requiring intensive or specialized treat ment, pregnancy, and chronic pain Degree to which the client acknowledges that substance use behaviors are a problem and is willing to confront them honestly Physical conditions that may require specially designed facilities or staffing Historical relapse patterns, periods of abstinence, and predictors of absti nence; client awareness of relapse triggers and craving Frequency, amount, and duration of use; chronicity of problems; indicators of abuse or dependence Ability to participate in confrontational treatment settings, and benefit from cognitive interventions and group therapy Degree of support from family and significant others, substancefree friends, involvement in support groups Other psychiatric symptoms that are likely to complicate the treatment of the substance use disorder and require treatment themselves, concerns about safety in certain settings (note that assessment for cooccurring disorders should include a determination of any psychiatric medications that the patient may be taking for the condition) Custody of dependent children or caring for noncustodial children and options for care of these children during rehabilitation Current domestic violence that affects the safety of the living environment, co occurring posttraumatic stress disorder or trauma history that might compli cate rehabilitation Prior successful and unsuccessful rehabilitation experiences that might influ ence decision about type of setting indicated Cultural identity, issues, and strengths that might influence the decision to seek culturally specific rehabilitation programs, culturally driven strengths or obstacles that might dictate level of care or setting Unique strengths and resources of the client and his or her environment Language or speech issues that make it difficult to communicate or require an interpreter familiar with substance abuse Chapter 3 Dependent Children Trauma and Violence Treatment History Cultural Background Strengths and Resources Language 40 and family factors. Administering these instruments requires varying degrees of sophistication on the part of the clinician. All instruments should be considered for their cultural, linguistic, level of cognitive compre hension, and developmental appropriateness for each patient. As a general rule, patients will stay at a residential treatment facility for 7 to 30 days. They tend to provide highly intensive counseling services and rely on peer sup port and confrontation to shape behaviors of clients. Patients in these programs often are working and par ticipate in counseling and peer support dur ing the evening and weekend hours. Patients receive 6 to 9 hours of counseling services each week in two or three contacts. They include 12 Step and other support groups aimed at maintaining the gains accomplished in treat Settings for Treatment Just as with settings for detoxification, set tings where substance abuse treatment is pro vided often are confused with the level of intensity of the services. It is increasingly clear that although level of intensity of ser vices and setting are both critical to success ful recovery, they are two separate dimen sions to be considered when linking clients to treatment. This process has been called "de linking" or "unbundling" and generally involves determining the need for social ser vices independently from the clinical intensity (Gastfriend and McLellan 1997; McGee and MeeLee 1997). These include settings specifically designed to deliver sub stance abuse treatment, such as freestanding substance abuse treatment centers, as well as settings operating for other purposes, includ ing mental health centers, jails and prisons, and community corrections facilities.
Cheap mentat ds syrup 100 ml line. How To Know if a Girl Likes You - 10 Signs She's Interested.
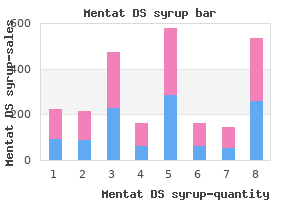
In hypersomnolence disorder symptoms 6 dpo buy cheap mentat ds syrup 100 ml on line, the mean sleep latency is typically less than 10 minutes and frequently 8 minutes or less schedule 8 medications victoria cheap 100 ml mentat ds syrup with visa. Functional Consequences of Hypersomnoience Disorder the low level of alertness that occurs while an individual fights the need for sleep can lead to reduced efficiency 606 treatment syphilis buy mentat ds syrup 100 ml without a prescription, diminished concentration 9 medications that cause fatigue order mentat ds syrup 100 ml overnight delivery, and poor memory during daytime activ ities symptoms 3dpo cheap mentat ds syrup 100 ml otc. Hypersomnoience can lead to significant distress and dysfunction in work and social relationships symptoms 0f pregnancy generic 100ml mentat ds syrup mastercard. Prolonged nocturnal sleep and difficulty awakening can result in difficulty in meeting morning obligations, such as arriving at work on time. Unintentional daytime sleep episodes can be embarrassing and even dangerous, if, for instance, the individual is driving or operating machinery when the episode occurs. If social or occupational demands lead to shorter nocturnal sleep, daytime symptoms may appear. In hypersomnoience disorder, by contrast, symptoms of excessive sleepiness occur regard less of nocturnal sleep duration. An inadequate amount of nocturnal sleep, or behaviorally induced insufficient sleep syndrome, can produce symptoms of daytime sleepiness very similar to those of hypersomnoience. An average sleep duration of fewer than 7 hours per night strongly suggests inadequate nocturnal sleep, and an average of more than 9-10 hours of sleep per 24-hour period suggests hypersomnoience. Individuals with inadequate noctur nal sleep typically "catch up" with longer sleep durations on days when they are free from social or occupational demands or on vacations. Unlike hypersomnoience, insufficient nocturnal sleep is unlikely to persist unabated for decades. A diagnosis of hypersomno ience disorder should not be made if there is a question regarding the adequacy of noctur nal sleep duration. A diagnostic and therapeutic trial of sleep extension for 10-14 days can often clarify the diagnosis. Hypersomnoience disorder should be distinguished from excessive sleepiness related to insufficient sleep quantity or quality and fatigue. Excessive sleepiness and fatigue are difficult to differentiate and may overlap considerably. Individuals with hypersomnoience and breathingrelated sleep disorders may have similar patterns of excessive sleepiness. Breathing- related sleep disorders are suggested by a history of loud snoring, pauses in breathing during sleep, brain injury, or cardiovascular disease and by the presence of obesity, oro pharyngeal anatomical abnormalities, hypertension, or heart failure on physical examina tion. Polysomnographie studies can confirm the presence of apneic events in breathingrelated sleep disorder (and their absence in hypersomnolence disorder). Circadian rhythm sleep-wake disorders are often characterized by daytime sleepiness. A history of an abnormal sleep-wake schedule (with shifted or irregular hours) is present in individuals with a circadian rhythm sleepwake disorder. Parasomnias rarely produce the prolonged, undisturbed nocturnal sleep or daytime sleepiness characteristic of hypersomnolence disorder. Hypersomnolence disorder must be distinguished from mental disorders that include hypersomnolence as an essential or associated feature. In particular, complaints of daytime sleepiness may occur in a major depressive episode, with atypical fea tures, and in the depressed phase of bipolar disorder. Assessment for other mental disorders is essential before a diagnosis of hypersomnolence disorder is considered. A diagnosis of hyper somnolence disorder can be made in the presence of another current or past mental disorder. Comorbidity H)ersomnolence can be associated with depressive disorders, bipolar disorders (during a depressive episode), and major depressive disorder, with seasonal pattern. Many individu als with hypersomnolence disorder have symptoms of depression that may meet criteria for a depressive disorder. This presentation may be related to the psychosocial consequences of persistent increased sleep need. Individuals with hyper somnolence disorder are also at risk for substance-related disorders, particularly related to self-medication with stimulants. This general lack of specificity may contribute to very heterogeneous profiles among indi viduals whose symptoms meet the same diagnostic criteria for hypersomnolence disorder. Recurrent periods of an irrepressible need to sleep, lapsing into sleep, or napping oc curring within the same day. These must have been occurring at least three times per week over the past 3 months. Episodes of cataplexy, defined as either (a) or (b), occurring at least a few times per month: a. In individuals with long-standing disease, brief (seconds to minutes) episodes of sudden bilateral loss of muscle tone with maintained consciousness that are precipitated by laughter or joking. In children or in individuals within 6 months of onset, spontaneous grimaces or jaw-opening episodes with tongue thrusting or a global hypotonia, without any obvious emotional triggers. Moderate: Cataplexy once daily or every few days, disturbed nocturnal sleep, and need for multiple naps daily. Severe: Drug-resistant cataplexy with multiple attacks daily, nearly constant sleepi ness, and disturbed noctumal sleep. Subtypes In narcolepsy without cataplexy but with hypocretin deficiency, unclear 'cataplexy-like" symptoms may be reported. Seizures, falls of other origin, and conversion disorder (functional neurological symptom disorder) should be excluded. In other cases, the destruction of hypocretin neurons may be secondary to trauma or hypothalamic surgery. Diagnostic Features the essential features of sleepiness in narcolepsy are recurrent daytime naps or lapses into sleep. Sleepiness typically occurs daily but must occur at a minimum three times a week for at least 3 months (Criterion A). Narcolepsy generally produces cataplexy, which most commonly presents as brief episodes (seconds to minutes) of sudden, bilateral loss of mus cle tone precipitated by emotions, typically laughing and joking. Muscles affected may include those of the neck, jaw, arms, legs, or whole body, resulting in head bobbing, jaw dropping, or complete falls. To meet Criterion Bl(a), cataplexy must be triggered by laughter or joking and must occur at least a few times per month when the condition is untreated or in the past. Cataplexy should not be confused with 'weakness" occurring in the context of athletic activities (physiological) or exclusively after unusual emotional triggers such as stress or anxiety (suggesting possible psychopathology). Episodes lasting hours or days, or those not triggered by emotions, are unlikely to be cataplexy, nor is rolling on the floor while laugh ing hysterically. In children close to onset, genuine cataplexy can be atypical, affecting primarily the face, causing grimaces or jaw opening with tongue thrusting ("cataplectic faces"). Alter natively, cataplexy may present as low-grade continuous hypotonia, yielding a wobbling walk. Criterion Bl(b) can be met in children or in individuals within 6months of a rapid onset. Narcolepsy-cataplexy nearly always results from the loss of hypothalamic hypocretin (orexin)-producing cells, causing hypocretin deficiency (less than or equal to one-third of control values, or 110 pg/mL in most laboratories). These tests must be performed after the individual has stopped all psychotropic medications, following 2 weeks of adequate sleep time (as documented with sleep diaries, actigraphy). Associated Features Supporting Diagnosis When sleepiness is severe, automatic behaviors may occur, with the individual continuing his or her activities in a semi-automatic, hazelike fashion without memory or conscious ness. Approximately 20%-60% of individuals experience vivid hypnagogic hallucinations before or upon falling asleep or hypnopompic hallucinations just after awakening. These hallucinations are distinct from the less vivid, nonhallucinatory dreamlike mentation at sleep onset that occurs in normal sleepers. Approximately 20%-60% of indi viduals experience sleep paralysis upon falling asleep or awakening, leaving them awake but unable to move or speak. However, many normal sleepers also report sleep paralysis, especially with stress or sleep deprivation. Nocturnal sleep disruption with frequent long or short awakenings is common and can be disabling. Individuals may appear sleepy or fall asleep in the waiting area or during clinical ex amination. During cataplexy, individuals may slump in a chair and have slurred speech or drooping eyelids. If the clinician has time to check reflexes during cataplexy (most attacks are less than 10 seconds), reflexes are abolished-an important finding distinguishing gen uine cataplexy from conversion disorder. Development and Course Onset is typically in children and adolescents/young adults but rarely in older adults. Severity is highest when onset is abrupt in children, and then decreases with age or with treatment, so that symptoms such as cataplexy can oc casionally disappear. Abrupt onset in young, prepubescent children can be associated with obesity and premature puberty, a phenotype more frequently observed since 2009. Onset in adults is often unclear, with some individuals reporting having had excessive sleepiness since birth. In 90% of cases, the first symptom to manifest is sleepiness or increased sleep, followed by cataplexy (within 1 year in 50% of cases, within 3 years in 85%). Excessive sleep rapidly progresses to an inability to stay awake during the day, and to maintain good sleep at night, without a clear increase in total 24-hour sleep needs. Sleep paralysis usually develops around puberty in children with prepubertal onset. Exacerbations of symptoms suggest lack of compliance with medications or devel opment of a concurrent sleep disorder, notably sleep apnea. Young children and adolescents with narcolepsy often develop aggression or behav ioral problems secondary to sleepiness and/or nighttime sleep disruption. Workload and social pressure increase through high school and college, reducing available sleep time at night. After retirement, indi viduals typically have more opportunity for napping, reducing the need for stimulants. Group A streptococcal throat infection, influenza (notably pandemic H lN l 2009), or other winter infections are likely triggers of the autoimmune process, pro ducing narcolepsy a few months later. The prevalence of narcolepsy is l% -2% in first-degree relatives (a 10- to 40-fold increase overall). Polymorphisms within the T-cell receptor alpha gene and other immune modulating genes also modulate risk slightly. Culture-Related Diagnostic issues Narcolepsy has been described in all ethnic groups and in many cultures. Among African Americans, more cases present without cataplexy or with atypical cataplexy, complicating diagnosis, especially in the presence of obesity and obstructive sleep apnea. Diagnostic Markers Functional imaging suggests impaired hypothalamic responses to humorous stimuli. Additional polysomnographic findings often include frequent arousals, decreased sleep efficiency, and increased stage 1 sleep. Periodic limb movements (found in about 40% of individuals with narcolepsy) and sleep apnea are often noted. The test is particularly useful in individuals with suspected conversion disorder and those without typical cataplexy, or in treatment-refractory cases. The diagnostic value of the test is not affected by medications, sleep deprivation, or circadian time, but the find ings are uninteretable when the individual is severely ill with a concurrent infection or head trauma or is comatose. Functional Consequences of Narcolepsy Driving and working are impaired, and individuals with narcolepsy should avoid jobs that place themselves. Once the narcolepsy is controlled with therapy, patients can usually drive, al though rarely long distances alone. Untreated individuals are also at risk for social isola tion and accidental injury to themselves or others. Social relations may suffer as these individuals strive to avert cataplexy by exerting control over emotions. Hypersomnolence and narcolepsy are similar with respect to the degree of daytime sleepiness, age at onset, and stable course over time but can be distin guished based on distinctive clinical and laboratory features. Individuals with hypersom nolence typically have longer and less disrupted nocturnal sleep, greater difficulty awakening, more persistent daytime sleepiness (as opposed to more discrete "sleep at tacks" in narcolepsy), longer and less refreshing daytime sleep episodes, and little or no dreaming during daytime naps. Sleep deprivation and insufficient nocturnal sleep are common in adolescents and shift workers. In adolescents, difficulties falling asleep at night are common, causing sleep deprivation. Because obstructive sleep apnea is more frequent than narcolepsy, cataplexy may be over looked (or absent), and the individual is assumed to have obstructive sleep apnea unre sponsive to usual therapies. Atypical features, such as long-lasting cataplexy or unusual triggers, may be present in conversion disorder (functional neurological symptom disorder). Full-blown, long-lasting pseudocataplexy may occur during consultation, allowing the examining physician enough time to verify reflexes, which remain intact. In children and adolescents, sleepiness can cause behavioral problems, including aggressiveness and in attention, leading to a misdiagnosis of attention-deficit/hyperactivity disorder. Seizures are not conmionly triggered by emotions, and when they are, the trigger is not usually laughing or joking. Sei zures characterized by isolated atonia are rarely seen in isolation of other seizures, and they also have signatures on the electroencephalogram. In young children, cataplexy can be misdiagnosed as chorea or pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections, especially in the context of a strep throat infection and high antistreptolysin O antibody levels. Some children may have an overlapping movement disorder close to on set of the cataplexy. In the presence of florid and vivid hypnagogic hallucinations, individuals may think these experiences are real-a feature that suggests schizophrenia. If cataplexy is present, the clinician should first assume that these symptoms are secondary to narcolepsy before con sidering a co-occurring diagnosis of schizophrenia. Comorbidity Narcolepsy can co-occur with bipolar, depressive, and anxiety disorders, and in rare cases with schizophrenia. Narcolepsy is also associated with increased body mass index or obe sity, especially when the narcolepsy is untreated.
References