


|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Ramanathan Kandasamy DA FRCA FCARCS
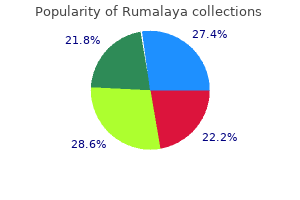
Other systems based on patterns of infiltration of predominant and secondary 3 tumor patterns have been proposed but have not been widely adopted symptoms 8 dpo purchase rumalaya 60pills on-line. Margins the nonperitonealized surface of the uncinate process (uncinate margin) constitutes the inferior-posterior retroperitoneal margin of pancreaticoduodenectomy specimensure 2) and should be inked; sections through 5 the tumor at its closest approach to this margin should be submitted medications known to cause nightmares purchase rumalaya 60pills mastercard. This margin has also been referred to as retroperitoneal margin and superior mesenteric artery margin treatment 0 rapid linear progression cheap rumalaya 60 pills. Posterior view of tumor arising in the pancreatic head medications rights purchase 60pills rumalaya amex, with dotted line indicating the location of the confluence of the portal and superior mesenteric veins. Because local recurrences of invasive pancreatic adenocarcinoma arise in the pancreatic bed corresponding to the uncinate margin and vascular groove of, Inking of the vascular groove corresponding to portal and superior mesenteric veins and submission of sections through the tumor at its closest approach to this surface is recommended. Reporting of tumor involvement of anterior and non-uncinate posterior surfaces is recommended, but not required. The vascular groove, anterior surface and the non-uncinate posterior surface are not considered 1,5 as resection margins. When dealing with an intraductal tumor, the pancreatic (neck/parenchymal) resection margin and the common bile duct margin (Whipple resection) are the most critical. Complete en face sections through the pancreatic resection margin and the common bile duct margin should be taken. Margin status can be reported as negative (R0, no residual disease), R1 1 (positive, microscopic residual disease) and R2 (positive, macroscopic residual disease). Treatment Effect Response of tumor to previous chemotherapy or radiation therapy should be reported. Several scoring systems 8 have been described, and a modified Ryan scheme is recommended, as below: Modified Ryan Scheme for Tumor Regression Score Description No viable cancer cells (complete response) 8 Tumor Regression Score 0 1 2 3 Single cells or rare small groups of cancer cells (near complete response) Residual cancer with evident tumor regression, but more than single cells or rare small groups of cancer cells (partial response) Extensive residual cancer with no evident tumor regression (poor or no response) Sizable pools of acellular mucin may be present after chemoradiation but should not be interpreted as representing residual tumor. The size of the viable tumor should be used to assign the ypT category, and requires a combined assessment of gross and microscopic findings. Multiple foci of viable tumor within the same tumor mass can be added to obtain the maximum linear dimension for staging. Venous/Lymphatic Vessel Invasion 13,14 Venous as well as lymphatic (small vessel) invasion has been shown to be an adverse prognostic factor. Perineural Invasion 14,15 Perineural invasion has been shown to be an adverse prognostic factor. Pathologic staging is usually performed after surgical resection of the primary tumor. Pathologic staging depends on pathologic documentation of the anatomic extent of disease, whether or not the primary tumor has been completely removed. If a biopsied tumor is not resected for any reason (eg, when technically infeasible) and if the highest T and N categories or the M1 category of the tumor can be confirmed microscopically, the criteria for pathologic classification and staging have been satisfied without total removal of the primary cancer. Although they do not affect the stage grouping, they indicate cases needing separate analysis. The "y" prefix indicates those cases in which classification is performed during or after initial multimodality therapy (ie, neoadjuvant chemotherapy, radiation therapy, or both chemotherapy and radiation therapy). The "y" categorization is not an estimate of tumor before multimodality therapy (ie, before initiation of neoadjuvant therapy). This applies only to grossly recognizable, synchronous primary carcinomas and not to a single, grossly detected tumor with multiple separate microscopic foci. The T categories T1-T3 are defined by tumor size as it provides better prognostic stratification than classification 17-21 Tumor size is determined by measurement of the gross lesion based on extension into peripancreatic tissue. For invasive carcinoma associated with intraductal papillary mucinous neoplasms, intraductal tubulopapillary neoplasms and mucinous cystic neoplasms, only the size of the invasive component should be used to determine the T category. The synoptic report is not required for intraductal papillary mucinous neoplasms, intraductal tubulopapillary neoplasms and mucinous cystic neoplasms in the absence of an invasive component. It is currently not clear whether size of the largest tumor focus or combined size of all invasive foci determines tumor outcome. Both measurements can be included in the pathology report, and the the maximum linear dimension of the largest invasive focus is used for staging. Extension beyond the pancreas may include invasion of peripancreatic soft tissue, peritoneum (including mesocolon, greater/lesser omentum), extrapancreatic biliary system, and/or duodenum (including the ampulla of Vater) for pancreatic head tumors, while stomach, spleen, left adrenal, and peritoneum can be involved by direct extension of body/tail tumors. Tumor extension in these areas does not affect staging, but should be noted in the pathology report. Invasion of the portal vein does not affect staging, but has been shown to be an independent 22 prognostic factor. T4 tumors are characterized by involvement of superior mesenteric artery, celiac axis and/or common hepatic artery. In most instances, these tumors are considered unresectable and hence T4 category is determined by radiologic studies and is not usually assigned by pathologists. T1 (left of dotted line) is defined as tumor measuring 2 cm or less in greatest dimension and limited to the pancreas. T2 (right of dotted line) is defined as tumor measuring more than 2 cm in greatest dimension and less than 4 cm in 33 greatest dimension. T4 tumor involves the celiac axis (above dotted line) or the superior mesenteric artery (below dotted line). T4 tumors 33 are considered unresectable and are rarely encountered in surgical pathology specimens. N Category Considerations the regional lymph nodes for head and neck cancers include lymph nodes along common bile duct, common hepatic artery, portal vein, pyloric, anterior and posterior pancreaticoduodenal arcades, superior mesenteric vein and right lateral wall of superior mesenteric arteryures 5 and 6). The regional lymph nodes for the pancreatic body and tail cancers include lymph nodes along common hepatic artery, celiac axis, splenic artery, and splenic hilum. Anatomic division of lymph nodes is not necessary, but separately submitted lymph nodes should be individually reported. Microscopic evaluation of at least Lymph node metastasis is an independent adverse prognostic factor. Regional lymph nodes of the pancreas (anterior view with pancreatic body removed to reveal retroperitoneal 32 vessels and lymph nodes). M Category Considerations 1,16 Peritoneal seeding or positive peritoneal cytology is considered M1. The most recent consensus recommends a 2-tier grading scheme for 31 better reproducibility and for better alignment of the grades with treatment options. Other Findings In addition to the examination of other tissues and organs that are part of pancreaticoduodenectomy specimens, pathologic evaluation may also include examination of the gastric antrum for gastritis (eg, Helicobacter pylori gastritis or chemical gastritis) and the duodenum for duodenitis, peptic ulcer disease, and ampullitis. A proposal for a new and more practical grading scheme for pancreatic ductal adenocarcinoma. Whipple made simple for surgical pathologists: orientation, dissection, and sampling of pancreaticoduodenectomy specimens for a more practical and accurate evaluation of pancreatic, distal common bile duct, and ampullary tumors. Classification of R1 resections for pancreatic cancer: the prognostic relevance of tumour involvement within 1 mm of a resection margin. Pathological response following long-course neoadjuvant chemoradiotherapy for locally advanced rectal cancer. Preoperative chemoradiation and pancreaticoduodenectomy for adenocarcinoma of the pancreas. Neoadjuvant chemoradiotherapy for adenocarcinoma of the pancreas: treatment variables and survival duration. Histologic grading of the extent of residual carcinoma following neoadjuvant chemoradiation in pancreatic ductal adenocarcinoma: a predictor for patient outcome. Validation of a proposed tumor regression grading scheme for pancreatic ductal adenocarcinoma after neoadjuvant therapy as a prognostic indicator for survival. Tumour characteristics predictive of survival following resection for ductal adenocarcinoma of the head of pancreas. Predicting patient survival after pancreaticoduodenectomy for malignancy: histopathological criteria based on perineural infiltration and lymphovascular invasion. Perineural and intra-neural invasion in posttherapy pancreaticoduodenectomy specimens predicts poor prognosis in patients with pancreatic ductal adenocarcinoma. Prognostic factors following curative resection for pancreatic adenocarcinoma: a population-based, linked database analysis of 396 patients. Predicting survival after surgical resection for pancreatic ductal adenocarcinoma. Multi-institutional validation study of the American Joint Commission on Cancer (8th Edition) changes for T and N staging in patients with pancreatic adenocarcinoma. Prognostic significance of pathologic nodal status in patients with resected pancreatic cancer.
Myxedema coma almost always occurs in the elderly and is usually precipitated by factors that impair respiration symptoms 9dpo bfp cheap rumalaya 60pills, such as drugs (especially sedatives medicine encyclopedia cheap rumalaya 60 pills on-line, anesthetics medications54583 buy rumalaya 60 pills free shipping, and antidepressants) treatment 7 purchase 60pills rumalaya fast delivery, pneumonia, congestive heart failure, myocardial infarction, gastrointestinal bleeding, or cerebrovascular accidents. Hypoventilation, leading to hypoxia and hypercapnia, plays a major role in pathogenesis; hypoglycemia and dilutional hyponatremia also contribute to the development of myxedema coma. This treatment has been advocated because T4 T3 conversion is impaired in myxedema coma. Supportive therapy should be provided to correct any associated metabolic disturbances. Parenteral hydrocortisone (50 mg every 6 h) should be administered, as there is impaired adrenal reserve in profound hypothyroidism. Any precipitating factors should be treated, including the early use of broad-spectrum antibiotics, pending the exclusion of infection. Ventilatory support with regular blood gas analysis is usually needed during the first 48 h. Indirect evidence suggests that stress is an important environmental factor, presumably operating through neuroendocrine effects on the immune system. Orbital fibroblasts may be particularly sensitive to cytokines, perhaps explaining the anatomic localization of the immune response. The increase in intraorbital pressure can lead to proptosis, diplopia, and optic neuropathy. The disorder rarely begins before adolescence and typically occurs between 20 and 50 years of age, but it also occurs in the elderly. In the elderly, features of thyrotoxicosis may be subtle or masked, and patients may present mainly with fatigue and weight loss, a condition known as apathetic thyrotoxicosis. Thyrotoxicosis may cause unexplained weight loss, despite an enhanced appetite, due to the increased metabolic rate. Other prominent features include hyperactivity, nervousness, and irritability, ultimately leading to a sense of easy fatigability in some patients. Insomnia and impaired concentration are common; apathetic thyrotoxicosis may be mistaken for depression in the elderly. Fine tremor is a frequent finding, best elicited by having patients stretch out their fingers while feeling the fingertips with the palm. Common neurologic manifestations include hyperreflexia, muscle wasting, and proximal myopathy without fasciculation. Thyrotoxicosis is sometimes associated with a form of hypokalemic periodic paralysis; this disorder is particularly common in Asian males with thyrotoxicosis. The most common cardiovascular manifestation is sinus tachycardia, often associated with palpitations, occasionally caused by supraventricular tachycardia. The high cardiac output produces a bounding pulse, widened pulse pressure, and an aortic systolic murmur and can lead to worsening of angina or heart failure in the elderly or those with preexisting heart disease. Treatment of the thyrotoxic state alone converts atrial fibrillation to normal sinus rhythm in about half of patients, suggesting the existence of an underlying cardiac problem in the remainder. The skin is usually warm and moist, and the patient may complain of sweating and heat intolerance, particularly during warm weather. Palmar erythema, onycholysis, and, less commonly, pruritus, urticaria, and diffuse hyperpigmentation may be evident. Hair texture may become fine, and a diffuse alopecia occurs in up to 40% of patients, persisting for months after restoration of euthyroidism. Gastrointestinal transit time is decreased, leading to increased stool frequency, often with diarrhea and occasionally mild steatorrhea. Women frequently experience oligomenorrhea or amenorrhea; in men, there may be impaired sexual function and, rarely, gynecomastia. The direct effect of thyroid hormones on bone resorption leads to osteopenia in longstanding thyrotoxicosis; mild hypercalcemia occurs in up to 20% of patients, but hypercalciuria is more common. There is a small increase in fracture rate in patients with a previous history of thyrotoxicosis. There may be a thrill or bruit due to the increased vascularity of the gland and the hyperdynamic circulation. Lid retraction, causing a staring appearance, can occur in any form of thyrotoxicosis and is the result of sympathetic overactivity. The earliest manifestations of ophthalmopathy are usually a sensation of grittiness, eye discomfort, and excess tearing. About a third of patients have proptosis, best detected by visualization of the sclera between the lower border of the iris and the lower eyelid, with the eyes in the primary position. In severe cases, proptosis may cause corneal exposure and damage, especially if the lids fail to close during sleep. The most serious manifestation is compression of the optic nerve at the apex of the orbit, leading to papilledema, peripheral field defects, and, if left untreated, permanent loss of vision. Although most frequent over the anterior and lateral aspects of the lower leg (hence the term pretibial myxedema), skin changes can occur at other sites, particularly after trauma. The typical lesion is a noninflamed, indurated plaque with a deep pink or purple color and an "orange-skin" appearance. Nodular involvement can occur, and the condition can rarely extend over the whole lower leg and foot, mimicking elephantiasis. Laboratory Evaluation Investigations used to determine the existence and cause of thyrotoxicosis are summarized in. The converse state of T4 toxicosis, with elevated total and unbound T4 and normal T3 levels, is occasionally seen when hyperthyroidism is induced by excess iodine, providing surplus substrate for thyroid hormone synthesis. Associated abnormalities that may cause diagnostic confusion in thyrotoxicosis include elevation of bilirubin, liver enzymes, and ferritin. Clinical features of thyrotoxicosis can mimic certain aspects of other disorders, including panic attacks, mania, pheochromocytoma, and weight loss associated with malignancy. The clinical course of ophthalmopathy does not follow that of the thyroid disease. However, the course is more fulminant in up to 5% of patients, requiring intervention in the acute phase if there is optic nerve compression or corneal ulceration. Diplopia may appear late in the disease due to fibrosis of the extraocular muscles. Some studies suggest that radioiodine treatment for hyperthyroidism worsens the eye disease in a small proportion of patients (especially smokers). Antithyroid drugs or surgery have no adverse effects on the clinical course of ophthalmopathy. Antithyroid drugs are the predominant therapy in many centers in Europe and Japan, whereas radioiodine is more often the first line of treatment in North America. These differences reflect the fact that no single approach is optimal and that patients may require multiple treatments to achieve remission. The main antithyroid drugs are the thionamides, such as propylthiouracil, carbimazole, and the active metabolite of the latter, methimazole. These drugs also reduce thyroid antibody levels by mechanisms that remain unclear, and they appear to enhance rates of remission. However, this effect is of minor benefit, except in the most severe thyrotoxicosis, and is offset by the much shorter half-life of this drug (90 min) compared to methimazole (6 h).
The character symptoms 6 days post embryo transfer generic rumalaya 60 pills, distribution medicine uses cheap rumalaya 60 pills amex, pathology medicine cabinet buy 60 pills rumalaya with visa, and progressive course of symptoms are vital for directing workup and treatment new medicine cheap 60 pills rumalaya free shipping. Many disorders selectively attack specific fiber types, while others indiscriminately affect all types. Sensory nerves: Paresthesias (burning, numbness, tingling) are common initial symptoms, with overt sensory loss occurring with progression of disease. Produces the classic "stocking-glove" distribution of symmetric involvement of all four distal extremities. Mononeuritis multiplex: A unique syndrome in which multiple individual peripheral nerves are progressively injured in an asymmetric and asynchronous fashion. As they involve direct injury to the nerve, recovery is often more limited and slow. Demyelinating neuropathies are often inflammatory and thus treatable; as the neuron itself is not directly injured, recovery is often the rule as remyelination occurs. Acute Polyneuropathies Acute-onset, rapidly progressive polyneuropathies, particularly those with motor or autonomic involvement, can produce life-threatening complications 540 over days to weeks. Given the decline of polio, it is now the most common cause of acute flaccid paralysis. Weakness severity can range from mild to complete quadriplegia with respiratory failure. Autonomic symptoms are prominent, and cardiac instability can be life-threatening. A unique variant, Miller-Fisher syndrome, produces symptoms of ophthalmoplegia, ataxia, and areflexia, with little weakness of the extremities. Vasculitic infarction of individual peripheral nerves occurs in an asynchronous and asymmetric fashion, producing a multifocal neuropathy involving both sensory and motor fibers; this random involvement of multiple individual peripheral nerves is called mononeuritis multiplex. Tx: Requires aggressive treatment with both steroids and an immunomodulator such as cyclophosphamide or methotrexate. Chronic Polyneuropathies Most polyneuropathies are indolent in onset and progression, with symptoms noted gradually and advancing over months to years. Its prevalence is 1 in 2500, making it the most common inherited neurologic disorder. Sx/Exam: Symptoms begin in the first and second decades, usually with distal weakness in the legs. Patients have high-arched feet (pes cavus) and hammer toes; progressive atrophy and weakness of the hands and feet; distal sensory loss; and reduced or absent reflexes. Life expectancy is typically normal, but significant morbidity results from progressive weakness. Sx/Exam: this "length-dependent" neuropathy affects the longest nerves first, initially producing paresthesias and pain in the feet; progression leads to a stocking-glove distribution of sensory and motor deficits. Sensory, motor, and autonomic nerves can be affected, with sensory symptoms predominating. Sx: Classic symptoms include progressive wrist pain; awakening at night with hand numbness; and paresthesias and weakness of the thumb and index finger. Exam: Findings include atrophy of the thenar eminence (the palmar muscle bulk at the base of the thumb), weakness of thumb opposition, and sensory abnormalities of the thumb and index finger. Patients with carpal tunnel syndrome often have symptoms at night that are relieved by shaking or wringing their hands. Sx/Exam: the most prominent symptom is "wrist drop" due to paralysis of the wrist extensor muscles; weakness of elbow extension (triceps) is also common. Surgical release or transposition of the nerve near the elbow is often tried but is not always beneficial. Tx: Involves identifying the risk factors for compression, initiating physical therapy, and using an ankle-foot orthosis; surgery is occasionally needed when a local mass is identified as the etiology of compression. Sx/Exam: the upper and lower halves of one-half of the face are affected, resulting in inability to fully close the eye or move the mouth on that side. In most cases, the etiology remains unclear, although an infectious or postinfectious cause is considered likely. Ramsay Hunt syndrome, in which unilateral facial paralysis is associated with herpetic blisters in the external auditory canal, supports this hypothesis. Eye protection (artificial tears; use of an eye patch at night) is crucial for preventing corneal abrasions. Patients typically complain of difficulty reaching above their heads, combing their hair, rising from a chair, or walking up and down stairs. Major types are polymyositis, dermatomyositis, and inclusion body myositis, each of which has distinctive patterns of muscle weakness, associated symptoms, and muscle pathology. Sx/Exam: Typically presents as slowly progressive, symmetric weakness in the proximal extremities and the neck flexors. Muscle biopsy reveals a characteristic pattern and distribution of inflammation that can help distinguish polymyositis from dermatomyositis and inclusion body myositis. Patients who fail to respond require more aggressive treatment with immunomodulators such as azathioprine or methotrexate. Sx/Exam: An inflammatory myopathy characterized by progressive proximal weakness associated with multiple distinct skin changes. These include the following: Periorbital edema and a purplish discoloration (heliotrope rash) of the upper eyelids, nose, and cheeks. Muscle biopsy shows a distinct pattern of inflammation characteristic of dermatomyositis, helping distinguish it from polymyositis and inclusion body myositis. In children, it is often associated with systemic vasculitis; in adults, it is occasionally the result of a paraneoplastic process from an underlying malignancy. Tx: the treatment of idiopathic dermatomyositis is the same as that of polymyositis. Sx: Preferentially affects the finger and forearm flexors of the upper extremities and the quadriceps of the lower extremities. Onset is insidious, with most patients complaining of difficulty with finger dexterity and grip strength as well as buckling of the knees while walking. Exam: Presents with prominent wasting of the finger and forearm flexors and quadriceps. Muscle biopsy reveals inflammatory changes as well as the presence of rimmed vacuoles (inclusion bodies) within abnormal muscle fibers. Tx: Despite its apparent inflammatory nature, inclusion body myositis does not respond well to either steroids or immunomodulators, and most patients lose the ability to ambulate within 10 years of diagnosis. These abnormalities are usually reversible with correction of the thyroid abnormality. Toxic Myopathies Many medications are associated with toxic myopathies, and the condition is usually reversible upon withdrawal of the offending toxin. As with other myopathies, the usual pattern is one of progressive, symmetric proximal muscle weakness. Most paraneoplastic syndromes result either from substances produced by tumor cells or from autoimmune complications of the response of the innate immune system to the cancer. Neurologic paraneoplastic syndromes appear to be caused by antibodies that cross-react with specific neuronal populations (see Table 13. Symptom onset is gradual, occurring over weeks to months; constitutional symptoms of the underlying tumor often lag by many months. Neurologic symptoms often become prominent even when the underlying tumor is difficult to detect. Thus, early identification of a neurologic paraneoplastic syndrome provides an opportunity to search for and aggressively treat the underlying tumor. Subacute Cerebellar Degeneration Associated with ovarian or breast cancer and anti-Yo antibodies (which cross-react specifically with cerebellar Purkinje cells). Most patients are middle-aged women who experience subacute-onset, progressive slurred speech as well as ataxia and limb incoordination.
Discount rumalaya 60pills with amex. Heart Sounds | S1 S2 S3 S4 and Murmurs Nursing Assessment.
Diseases