




|
STUDENT DIGITAL NEWSLETTER ALAGAPPA INSTITUTIONS |

|
Nelson Jen An Chao, MD
https://medicine.duke.edu/faculty/nelson-jen-chao-md
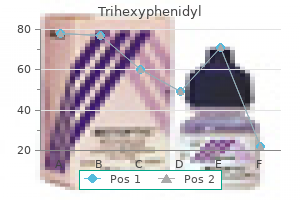
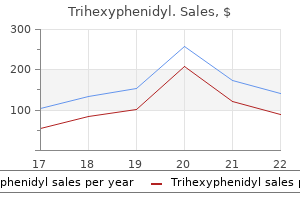
Generic equivalent medications for brands listed as a step 2 agent will also be targeted when available pain treatment diverticulitis order 2 mg trihexyphenidyl free shipping. Class 1: Super Potent Class 2: Potent Class 5: Lower Mid-Strength Class 6: Mild Step 2 medications -Ultravate (halobetasol propionate 0 a better life pain treatment center flagstaff az buy generic trihexyphenidyl 2 mg on-line. Guidelines of care for the management and treatment of psoriasis with topical therapies ocean view pain treatment center discount 2mg trihexyphenidyl mastercard. Indications Drug Name: Upneeq (oxymetazoline) Blepharoptosis Indicated for the treatment of acquired blepharoptosis in adults pain tmj treatment purchase trihexyphenidyl 2mg with visa. Notes Product Name: Upneeq [a] Approval Length Therapy Stage Guideline Type 12 month(s) Reauthorization Prior Authorization Page 740 Approval Criteria 1 - Documentation of positive clinical response to therapy Notes [a] State mandates may apply treatment for shingles pain mayo clinic generic trihexyphenidyl 2 mg visa. Background Benefit/Coverage/Program Information Background: Upneeq (oxymetazoline) 0 pain treatment center of illinois new lenox discount trihexyphenidyl 2mg fast delivery. Criteria Product Name: Vascepa* [a] Diagnosis Cardiovascular Risk Reduction Page 743 Approval Length Therapy Stage Guideline Type 12 month(s) Initial Authorization Prior Authorization Approval Criteria 1 - Vascepa will be approved based on all of the following criteria: 1. Product Name: Vascepa* [a] Diagnosis Approval Length Therapy Stage Guideline Type Cardiovascular Risk Reduction 12 month(s) Reauthorization Prior Authorization Approval Criteria 1 - Vascepa will be approved based on all of the following criteria: 1. Any federal regulatory requirements an d the member specific benefit plan coverage may also impact coverage Page 747 criteria. Revision History Date 4/6/2021 Notes Modified pre-treatment triglyceride levels for cardiovascular risk reducti on. Indications Drug Name: Vecamyl (mecamylamine) Moderately Severe to Severe Essential Hypertension Indicated for the management of moderately severe to severe essential hypertension and uncomplicated cases of malignant hypertension. Criteria Product Name: Vecamyl Diagnosis Approval Length Therapy Stage Hypertension 12 month(s) Initial Authorization Page 750 Guideline Type Notification Approval Criteria 1 - One of the following: 1. Background Benefit/Coverage/Program Information Background: Vecamyl (mecamylamine) is indicated for the management of moderately severe to severe essential hypertension and uncomplicated cases of malignant hypertension. The product was withdrawn in September 2009; withdrawal was not due to safety concerns. Indications Drug Name: Veregen (sinecatechins) Warts Indicated for the treatment of external genital and perianal warts in immunocompetent patients. Criteria Product Name: Veregen [a] Approval Length Guideline Type 4 month(s) Step Therapy Page 753 Approval Criteria 1 - Patient has a history of failure, contraindication, or intolerance to one of the following: · · Imiquimod (generic Aldara) Podofilox (generic Conylox) [a] State mandates may apply. Background Benefit/Coverage/Program Information Background: Veregen (sinecatechins) is indicated for the treatment of external genital and perianal warts in immunocompetent patients. This program requires a member to try imiquimod or podofilox prior to receiving coverage for Veregen. Verquvo has a boxed warning for embryo-fetal toxicity and should not be used during pregnancy. Use of automated approval and re-approval processes varies by program and/or therapeutic class. Criteria Product Name: Vyleesi Approval Length Therapy Stage 2 month(s) Initial Authorization Page 763 Guideline Type Prior Authorization Approval Criteria 1 - Diagnosis of one of the following: 1. Background Benefit/Coverage/Program Information Background: Anti-obesity agents are indicated in the management of obesity as an adjunct to lifestyle modifications including diet, exercise and behavioral modification. Medication therapy may provide modest weight reduction in conjunction with lifestyle modifications and therapy selection may be based on a specific medications side effects and warnings. National Institutes of Health, National Heart, Lung, and Blood Institute, and North American Association for the Study of Obesity. The Practical Guide: Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. Expert Committee Recommendations Regarding the Prevention, Assessment, and Treatment of Child and Adolescent Overweight and Obesity: Summary Report. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Pharmacological Management of Obesity: An Endocrine Society Clinical Practice Guideline. Indications Drug Name: Winlevi (clascoterone) Acne Vulgaris Indicated for the topical treatment of acne vulgaris in patients 12 years of age and older. Background Benefit/Coverage/Program Information Background: Winlevi (clascoterone) is an androgen receptor inhibitor indicated for the topical treatment of acne vulgaris in patients 12 years of age and older. Guidelines from the American Academy of Dermatology recommend topical therapies including retinoids, antibiotics in combination with benzoyl peroxide, azelaic acid and dapsone for mild to moderate acne. Systemic antibiotics are first-line in moderate to severe acne with concomitant topical therapy of benzoyl peroxide or a retinoid. Hepatic encephalopathy Indicated for the risk reduction of hepatic encephalopathy recurrence in adults. Off Label Uses: Inflammatory bowel diseases There is some limited data to support the off label use of Xifaxan for the treatment of inflammatory bowel diseases. Product Name: Xifaxan [a] Diagnosis Approval Length Therapy Stage Guideline Type Hepatic Encephalopathy 12 month(s) Reauthorization Prior Authorization Approval Criteria 1 - Documentation of positive clinical response to Xifaxan therapy Notes [a] State mandates may apply. Any federal regulatory requirements an d the member specific benefit plan coverage may also impact coverage Page 785 criteria. Product Name: Xifaxan [a] Diagnosis Approval Length Therapy Stage Guideline Type Inflammatory Bowel Disease. Notes Product Name: Xifaxan [a] Diagnosis Approval Length Therapy Stage Guideline Type Inflammatory Bowel Disease. There is some limited data to support the off label use of Xifaxan for the treatment of inflammatory bowel diseases. Pimentel H, Lembo A, Chey W, et al: Rifaximin therapy for patients with Irritable Bowel Syndrome without constipation. American Gastroenterological Association Institute Guideline on the Pharmacological Management of Irritable Bowel Syndrome. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Any federal regulatory requirements and the member specific benefit pl an coverage may also impact coverage criteria. Use of automated approval and re-approval processes varies by program and/or therapeutic class *Brand Singulair tablets and chewable tablets are typically excluded from coverage. Global Initiative for Asthma: Global Strategy for Asthma Management and prevention. Revision History Date 3/23/2021 Notes Modified step to require a failure of one or a contraindication or intolera nce to both step one medications. Indications Drug Name: Zilxi (minocycline) Rosacea with Inflammatory Lesions Indicated for the treatment of inflammatory lesions of rosacea in adults. Criteria Product Name: Zilxi [a] Approval Length Therapy Stage Guideline Type 12 month(s) Initial Authorization Prior Authorization Page 792 Approval Criteria 1 - Diagnosis of rosacea with inflammatory lesions. Notes Product Name: Zilxi [a] Approval Length Therapy Stage Guideline Type 12 month(s) Reauthorization Prior Authorization Approval Criteria 1 - Documentation of a positive clinical response to therapy Notes [a] State mandates may apply. This formulation of minocycline has not been evaluated in the treatment of infections. To reduce the development of drug-resistant bacteria as well as to maintain the effectiveness of other antibacterial drugs, Zilxi should be used only as indicated. Zilxi is a tetracycline-class drug indicated for the treatment of inflammatory lesions of rosacea in adults. Step therapy programs are utilized to encourage use of lower cost alternatives for certain therapeutic classes. This program requires a member to a trial of lower cost rosacea medications before providing coverage for Zilxi. Revision History Date 4/21/2021 Notes 02/2021 P&T - Updated criteria to trial of one. Indications Drug Name: Zomig (zolmitriptan) nasal spray Migraine Indicated for the acute treatment of migraine with or without aura in adults and pediatric patients 12 years of age and older. Background Benefit/Coverage/Program Information Background Zomig (zolmitriptan) nasal spray is indicated for the acute treatment of migraine with or without aura in adults and pediatric patients 12 years of age and older. Zomig nasal spray is not intended for the prophylactic therapy of migraine attacks or for the treatment of cluster headache. This program requires a member to try generic triptans before providing coverage for Zomig nasal spray. Use of automated approval and re-approval processes varies by Page 796 program and/or therapeutic class. Because of rapid advances in the medical sciences, we recommend that the independent verification of diagnoses and drug dosages be made. No part of this book may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without written permission from the publisher. Highway 1, Suite 307 North Palm Beach, Florida 33408 Printed and bound in the United States of America Table of Contents Preface. Delayed Radiation Injuries (Soft Tissue and Bony Necrosis) and Potential for Future Research. He observed that pressurized patients were not as cyanotic after the use of nitrous oxide during induction of anesthesia as compared to patients anesthetized at atmospheric pressure. Lorrain-Smith6 showed that oxygen under pressure had potentially deleterious consequences on the human body with side effects that included central nervous system and pulmonary toxicity. The efforts of Churchill-Davidson and Boerema in the 1950s and 1960s spurred the modern scientific use of clinical hyperbaric medicine. In 1967, the Undersea Medical Society was founded by six United States Naval diving and submarine medical officers with the explicit goal of promoting diving and undersea medicine. In short order, this society expanded to include those interested in clinical hyperbaric medicine. In recognition of the dual interest by members in both diving and clinical applications of compression therapy, the society was renamed the Undersea and Hyperbaric Medical Society in 1986. It remains the leading not for profit organization dedicated to reporting scientifically and medically efficacious and relevant information pertaining to hyperbaric and undersea medicine. In 1972, an ad hoc Medicare committee was formed to evaluate the efficacy of hyperbaric oxygen therapy for specified medical conditions. The focus was to determine if this treatment modality showed therapeutic benefit and merited insurance coverage. The growth of the body of scientific evidence that had developed over the preceding years supported this endeavor and recognition for the field. The report is usually published every three to five years and was last published in 2014. Additionally, this document continues to be used by the Centers for Medicare and Medicaid Services and other third party insurance carriers in determining payment. The report, currently in its 14th edition, has grown in size and depth to reflect the evolution of the literature. The Undersea and Hyperbaric Medical Society continues to maintain its reputation for its expertise on hyperbaric therapy. With leading experts authoring chapters in their respective fields, this publication continues to provide the most current and up to date guidance and support for scientists and practitioners of hyperbaric oxygen therapy. Aero-Chalinos or a register for the air for the better preservation of health and cure of diseases, after a new method. Compressed Air as a Therapeutic Agent in the Treatment of Consumption, Asthma, Chronic Bronchitis and Other Diseases. Over the intervening years, the interests of the Society have enlarged to include clinical hyperbaric oxygen therapy. The society has grown to over 2,000 members and has established the largest repository of diving and hyperbaric research collected in one place. The results of ongoing research and clinical aspects of undersea and hyperbaric medicine are reported annually at scientific meetings and in Undersea and Hyperbaric Medicine published bi-monthly. Previously the society supported two journals, Undersea Biomedical Research and the Journal of Hyperbaric Medicine. In certain circumstances hyperbaric oxygen therapy represents the primary treatment modality while in others it is an adjunct to surgical or pharmacologic interventions. Class C Animal, no human occupancy Clinical treatments can be carried out in either a Class A (multi) or B (mono) chamber system. A Class A system holds two or more people (patients, observers, and/or support personnel); the chamber is pressurized with compressed air while the patients breathe near 100% oxygen via masks, head hoods, or endotracheal tubes. It is important to note that Class B systems can and are pressurized with compressed air while the patients breathe near 100% oxygen via masks, head hoods, or endotracheal tubes. Extensive research on oxygen toxicity was undertaken to establish safe limits, overall safety, and medical and physiologic aspects of the compressed gas environment. Class A x ~ Hyperbaric Oxygen Therapy Indications Copyright © 2019 Undersea and Hyperbaric Medical Society, Inc. To achieve this goal, the multispecialty committee is comprised of practitioners and scientific investigators in the fields of internal medicine, infectious diseases, pharmacology, emergency medicine, general surgery, orthopedic surgery, trauma surgery, thoracic surgery, otolaryngology, oral and maxillofacial surgery, anesthesiology, pulmonology, critical care, radiation oncology and aerospace medicine. From the 28 indications for which third-party reimbursement was recommended in the 1976 and 1979 reports, the number of recognized indications has been refined to 14 in the current report. These indications are those for which in vitro and in vivo pre-clinical research data as well as extensive positive clinical experience and study have become convincing. Evidence considered by the Committee includes sound physiologic rationale; in vivo or in vitro studies that demonstrate effectiveness; controlled animal studies, prospective controlled clinical studies; and extensive clinical experience from multiple, recognized hyperbaric medicine centers. Studies in progress will continue to clarify mechanisms of action, optimal oxygen dosage, duration of exposure times, frequency of treatments, and patient selection criteria. The Committee also reviews cost effectiveness and has established guidelines for each entity. However, the Committee recommends that each individual hyperbaric facility, whether monoplace or multiplace, establish its own charges consistent with the actual local costs of providing such service. Hyperbaric Oxygen: Definition ~ xi Copyright © 2019 Undersea and Hyperbaric Medical Society, Inc. Such review should involve discussion of the clinical case with another qualified hyperbaric medicine physician from an outside institution. This consideration can be initiated from within the Committee itself or may result in response to a written request by a non-Committee member. Two members of the Hyperbaric Oxygen Committee review the position paper and each writes a critique.
During the fifth week pain medication for dogs after dental surgery cheap 2mg trihexyphenidyl mastercard, peripheral nerves grow from the developing limb plexuses (brachial and lumbosacral) into the mesenchyme of the limb pain treatment for rheumatoid arthritis generic trihexyphenidyl 2 mg mastercard. The spinal nerves are distributed in segmental bands anterior knee pain treatment exercises discount trihexyphenidyl 2 mg visa, supplying both dorsal and ventral surfaces of the limb pain treatment in hindi order 2mg trihexyphenidyl with amex. A dermatome is the area of skin supplied by a single spinal nerve and its spinal ganglion; however pain medication for dogs dose 2 mg trihexyphenidyl, cutaneous nerve areas and dermatomes show considerable overlapping pain medication for dogs tramadol cheap trihexyphenidyl 2 mg free shipping. As the limbs elongate, the cutaneous distribution of the spinal nerves migrates along the limbs and no longer reaches the surface in the distal part of the limbs. Although the original dermatomal pattern changes during growth of the limbs, an orderly sequence of distribution can still be recognized in the adult. In the upper limb, observe that the areas supplied by C5 and C6 adjoin the areas supplied by T2, T1, and C8, but the overlap between them is minimal at the ventral axial line. Dorsal (A) and plantar (B) views of the right foot of a human embryo, Carnegie stage 19 (approximately 48 days). The toe buds (arrowheads in A) and the heel cushion and metatarsal tactile elevation (asterisks in B) have just appeared. Dorsal (C) and distal (D) views of the right foot of human embryos, Carnegie stage 22 (approximately 55 days). Note the dorsiflexion of the metatarsus and toes (C) as well as the thickened heel cushion (D). C and D, Paraffin sections of the tarsus and metatarsus of a young human fetus, stained with hematoxylin and eosin. The separation of the interosseous muscles (im) and short flexor muscles of the big toe (sfh) is clearly seen. The plantar crossing (cr) of the tendons of the long flexors of the digits and hallux is shown in D. If the dorsal root supplying the area is cut, the dermatomal patterns indicate that there may be a slight deficit in the area indicated. Because there is overlapping of dermatomes, a particular area of skin is not exclusively innervated by a single segmental nerve. The limb dermatomes may be traced progressively down the lateral aspect of the upper limb and back up its medial aspect. A comparable distribution of dermatomes occurs in the lower limbs, which may be traced down the ventral aspect and then up the dorsal aspect of the lower limbs. When the limbs descend, they carry their nerves with them; this explains the oblique course of the nerves arising from the brachial and lumbosacral plexuses. All regions of the limbs are apparent and the digits of the hands and feet are separated. The primordial vascular pattern consists of a primary axial artery and its branches. The vascular patterns change as the limbs develop, chiefly by angiogenesis (sprouting from existing vessels). The primary axial artery becomes the brachial artery in the arm and the common interosseous artery in the forearm, which has anterior and posterior interosseous branches. As the digits (fingers) form, the marginal sinus breaks up and the final venous pattern, represented by the basilic and cephalic veins and their tributaries, develops. In the thigh, the primary axial artery is represented by the deep artery of the thigh (Latin, profunda femoris artery). In the leg, the primary axial artery is represented by the anterior and posterior tibial arteries. Although these anomalies are usually of no serious medical consequence, they may serve as indicators of more serious anomalies and may be part of a recognizable pattern of birth defects. A, Approximately 48 days, showing the limbs extending ventrally and the hand- and footplates facing each other. B, Approximately 51 days, showing the upper limbs bent at the elbows and the hands curved over the thorax. Figure 16-10 Illustrations of the development of the dermatomal patterns of the limbs. B and E, Similar views later in the fifth week showing the modified arrangement of dermatomes. The primordial dermatomal pattern has disappeared but an orderly sequence of dermatomes can still be recognized. F, Note that most of the original ventral surface of the lower limb lies on the back of the adult limb. This results from the medial rotation of the lower limb that occurs toward the end of the embryonic period. In the upper limb, the ventral axial line extends along the anterior surface of the arm and forearm. In the lower limb, the ventral axial line extends along the medial side of the thigh and knee to the posteromedial aspect of the leg to the heel. This statement is based on clinical studies of infants exposed to thalidomide, a potent human teratogen, during the embryonic period. Exposure to this teratogen before day 33 may cause severe limb defects, such as amelia, the absence of limbs. Consequently, a teratogen that could cause amelia of the limbs or parts of them must act before 36 days, the end of the critical period of limb development. Many severe limb anomalies occurred from 1957 to 1962 as a result of maternal ingestion of thalidomide. This drug, widely used as a sedative and antinauseant, was withdrawn from the market in December 1961. Because thalidomide is now used for the treatment of leprosy and several other disorders, it must be emphasized that thalidomide is absolutely contraindicated in women of child-bearing age. Several unrelated congenital anomalies of the lower limb were found to be associated with a similar aberrant arterial pattern, which might be of some importance in the pathogenesis of these defects. A, Sketch of the primordial cardiovascular system in a 4week embryo, approximately 26 days. Causes of Limb Anomalies Anomalies or defects of the limbs originate at different stages of development. Suppression of limb bud development during the early part of the fourth week results in absence of the limbs, amelia. Arrest or disturbance of differentiation or growth of the limbs during the fifth week results in various types of meromelia. A reduced quantity of amniotic fluid (oligohydramnios) is commonly associated with limb deformations; however, the significance of in utero mechanical influences on congenital postural deformation is still open to question. Note also that the right leg is shortened and the femur and tibia are bowed and hypoplastic. C, Radiograph showing partial absence and fusion of the lower ends of the tibia and fibula in a 5-year-old child. The hand or foot is divided into two parts that oppose each other like lobster claws. The hand deviates laterally (radially), and the ulna bows with the concavity on the lateral side of the forearm. This anomaly results from failure of the mesenchymal primordium of the radius to form during the fifth week of development. Brachydactyly Shortness of the digits (fingers or toes) is the result of reduction in the length of the phalanges. This anomaly is usually inherited as a dominant trait and is often associated with shortness of stature. Polydactyly the term supernumerary digits refers to the presence of more than the usual number of fingers or toes. Often the extra digit is incompletely formed and lacks normal muscular development. If the hand is affected, the extra digit is most commonly medial or lateral rather than central. Cutaneous syndactyly (simple webbing between digits) is the most common limb anomaly. Cutaneous syndactyly results from failure of the webs to degenerate between two or more digits. Osseous syndactyly (fusion of the bones- synostosis) occurs when the notches between the digital rays fail to develop; as a result, separation of the digits does not occur. Syndactyly is most frequently observed between the third and fourth fingers and between the second and third toes. Congenital Clubfoot Any deformity of the foot involving the talus (ankle bone) is called talipes or clubfoot. Clubfoot is a relatively common anomaly, occurring approximately once in 1000 births. It is characterized by an abnormal position of the foot that prevents normal weight bearing. Clubfoot is bilateral in approximately 50% of cases, and it occurs approximately twice as frequently in males. Clubfoot appears to follow a multifactorial pattern of inheritance; hence, any intrauterine position that results in abnormal positioning of the feet may cause clubfeet if the fetus is genetically predispositioned to this deformity. Congenital Dislocation of the Hip this deformity occurs approximately once in 1500 newborn infants and is more common in females than in males. The joint capsule is very relaxed at birth, and there is underdevelopment of the acetabulum of the hip bone and the head of femur. Generalized joint laxity is often a dominantly inherited condition that appears to be associated with congenital dislocation of the hip, which follows a multifactorial pattern of inheritance. The tissues of the limb buds are derived from two main sources: mesoderm and ectoderm. Apoptosis (programmed cell death) is an important mechanism in limb development, for example, in the formation of the notches between the digital rays. Limb muscles are derived from mesenchyme (myogenic precursor cells) originating in the somites. Most blood vessels of the limb buds arise as buds from the intersegmental arteries and drain into the cardinal veins. Initially, the developing limbs are directed caudally; later they project ventrally, and finally, they rotate on their longitudinal axes. The majority of limb anomalies are caused by genetic factors; however, many limb defects probably result from an interaction of genetic and environmental factors (multifactorial inheritance). This condition results from formation of one or more extra digital rays during the embryonic period. Cutaneous syndactyly (C) is the most common form of this condition and is probably due to incomplete programmed cell death (apoptosis) in the tissues between the digital rays during embryonic life. Kabak S, Boizow L: Organogenese des Extremitätenskeletts und der Extremitätengelenke beim Menschenembryo. Zuniga A: Globalisation reaches gene regulation: the case for vertebrate limb development. It is the notochord and paraxial mesenchyme that induce the overlying ectoderm to differentiate into the neural plate. Formation of the neural folds, neural tube, and neural crest from the neural plate is illustrated in Figures 17-1B to F and 17-2. Neurulation-formation of the neural plate and neural tube-begins during stage 10 of development (2223 days) in the region of the fourth to sixth pairs of somites. At this stage, the cranial two thirds of the neural plate and tube, as far caudal as the fourth pair of somites, represent the future brain, and the caudal one third of the neural plate and tube represents the future spinal cord. Fusion of the neural folds and formation of the neural tube proceeds in cranial and caudal directions until only small areas of the tube remain open at both ends. Here the lumen of the neural tube-neural canal-communicates freely with the amniotic cavity. The cranial opening, the rostral neuropore, closes on approximately the 25th day and the caudal neuropore 2 days later. Closure of the neuropores coincides with the establishment of a blood vascular circulation for the neural tube. The neural canal forms the ventricular system of the brain and the central canal of the spinal cord. Nonclosure of the Neural Tube the current hypothesis is that there are multiple, possibly five, closure sites involved in the formation of the neural tube. Failure of closure of site 1 results in spina bifida cystica; meroencephaly (anencephaly) results from failure of closure of site 2; craniorachischisis results from failure of sites 2, 4, and 1 to close; and site 3 nonfusion is rare. It has been suggested that the most caudal region may have a fifth closure site from the second lumbar vertebra to the second sacral vertebra and that closure inferior to the second sacral vertebra is by secondary neurulation. The lateral walls of the neural tube thicken, gradually reducing the size of the neural canal until only a minute central canal of the spinal cord is present at 9 to 10 weeks. Initially, the wall of the neural tube is composed of a thick, pseudostratified, columnar neuroepithelium. These neuroepithelial cells constitute the ventricular zone (ependymal layer), which gives rise to all neurons and macroglial cells (macroglia) in the spinal cord. Macroglial cells are the larger members of the neuroglial family of cells, which includes astrocytes and oligodendrocytes. Soon a marginal zone composed of the outer parts of the neuroepithelial cells becomes recognizable. This zone gradually becomes the white matter (substance) of the spinal cord as axons grow into it from nerve cell bodies in the spinal cord, spinal ganglia, and brain. Some dividing neuroepithelial cells in the ventricular zone differentiate into primordial neurons-neuroblasts. These embryonic cells form an intermediate zone (mantle layer) between the ventricular and marginal zones.
The vestibulocerebellum is also critical in learning new relationships between eye movements and visual displacement st john pain treatment center purchase trihexyphenidyl 2mg without prescription. Lesions of the vestibulocerebellum cause ocular dysmetria (inability to perform accurate saccades) pain and spine treatment center dworkin order 2mg trihexyphenidyl amex, ocular flutter (rapid to-andfro eye movements) midwest pain treatment center beloit wi generic trihexyphenidyl 2mg with visa, and opsoclonus (chaotic eye movements) pain management utilization cheap trihexyphenidyl 2mg online. The abducting eye shows horizontal gaze-evoked nystagmus (slow phase toward the midline tailbone pain treatment yoga trihexyphenidyl 2 mg cheap, rapid jerks laterally) best pain medication for shingles order trihexyphenidyl 2 mg line, while the adducting eye stops in the midline (if the lesion is complete) or fails to fully adduct (if it is partial). Vertical saccades, however, are implemented by the superior colliculus inputs to the rostral interstitial nucleus of Cajal, and are intact. The Ocular Motor Examination the examination of the ocular motor system in awake, alert subjects involves testing both voluntary and reflex eye movements. In patients with stupor or coma, testing of reflex eyelid and ocular movements must suffice. The eyelids at rest in coma, as in sleep, are maintained in a closed position by tonic contraction of the orbicularis oculi muscles. The eyelids of a comatose patient close smoothly and gradually, a movement that cannot be duplicated by an awake individual simulating unconsciousness. Absence of tone or failure to close either eyelid can indicate facial motor weakness. Blepharospasm, or strong resistance to eyelid opening and then rapid closure, is usually voluntary, suggesting that the patient is not truly comatose. However, lethargic patients with either metabolic or structural lesions may resist eye opening, as do some patients with a nondominant parietal lobe infarct. In patients with unilateral forebrain infarcts, the ptosis is often ipsilateral to hemiparesis. Spontaneous blinking usually is lost in coma as a function of the depressed level of consciousness and concomitant eye closure. However, in persistent vegetative state, it may return during cycles of eye opening (Chapter 9). Blinking in response to a loud sound or a bright light implies that the afferent sensory pathways are intact to the brainstem, but does not necessarily mean that they are active at a forebrain level. Even patients with complete destruction of the visual cortex may recover reflex blink responses to light,107 but not to threat. The corneal reflex can be performed by approaching the eye from the side with a wisp of cotton that is then gently applied to the sclera and pulled across it to touch the corneal surface. Corneal trauma can be completely avoided by testing the corneal reflex with sterile saline. Two to three drops of sterile saline are dropped on the cornea from a height of 4 to 6 inches. However, some patients who wear contact lenses may have permanent suppression of the corneal reflex. A small flashlight or bright ophthalmoscope held about 50 cm from the face and shined toward the eyes of the patient should reflect off the same point in the cornea of each eye if the gaze is conjugate. If it is possible to obtain a history, ask about eye movements, as a congenital strabismus may be misinterpreted as dysconjugate eye movements due to a brainstem lesion. Slowly roving eye movements are typical of metabolic encephalopathy, and if conjugate, they imply an intact ocular motor system. The head is rotated first in a lateral direction to either side while holding the eyelids open. This can be done by grasping the head on either side with both hands and using the thumbs to reach across to the eyelids and hold them open. The head movements should be brisk, and when the head position is held at each extreme for a few seconds, the eyes should gradually come back to midposition. The head is then rotated in a vertical plane (as in head nodding) and the eyes are observed for vertical conjugate movement. In an awake patient, the voluntary control of gaze overcomes this reflex response. However, in patients with impaired consciousness, the oculocephalic reflex should predominate. There may also be a small contribution from proprioceptive afferents from the neck,112 which also travel through the medial longitudinal fasciculus. Because these pathways overlap extensively with the ascending arousal system (see Figure 28), it is quite unusual for patients with structural causes of coma to have a normal oculocephalic examination. In contrast, patients with metabolic encephalopathy, particularly due to hepatic failure, may have exaggerated or very brisk oculocephalic responses. Eye movements in patients who are deeply comatose may respond sluggishly or not at all to oculocephalic stimulation. In such cases, more intense vestibular stimulation may be obtained by testing caloric vestibulo-ocular responses. With appropriate equipment, vestibulo-ocular monitoring can be done using galvanic stimulation and video-oculography. The ear canal is first examined and, if necessary, cerumen is removed to allow clear visualization that the tympanic membrane is intact. The head of the bed is then raised to about 30 degrees to bring the horizontal semicircular canal into a vertical position so that the response is maximal. If the patient is merely sleepy, the canal may be irrigated with cool water (158C to 208C); this usually induces a brisk response and may occasionally cause nausea and vomiting. Fortunately, in practice, it is rarely necessary to use caloric stimulation in such patients. If the patient is deeply comatose, a maximal stimulus is obtained by using ice water. An emesis basin can be placed below the ear, seated on an absorbent pad, to catch the effluent. The ice water is infused at a rate of about 10 mL/minute for 5 minutes, or until a response is obtained. After a response is obtained, it is necessary to wait at least 5 minutes for the response to dissipate before testing the opposite ear. To test vertical eye movements, both external auditory canals are irrigated simultaneously with cold water (causing the eyes to deviate downward) or warm water (causing upward deviation). The cold water induces a downward convection current, away from the ampulla, in the endolymph within the horizontal semicircular canal. The effect of the current upon the hair cells in the ampulla is to reduce tonic discharge of the vestibular neurons. The left-hand side shows the responses to oculocephalic maneuvers (which should only be done after the possibility of cervical spine injury has been eliminated). The right-hand side shows responses to caloric stimulation with cold or warm water (see text for explanation). Normal brainstem reflexes in a patient with metabolic encephalopathy are illustrated in row (A). The patient shown in row (B) has a lesion of the right side of the pons (see Figure 28), causing a paralysis of gaze to that side with either eye. Row (E) illustrates a patient with a midbrain infarction eliminating both the oculomotor and trochlear responses, leaving only bilateral abduction responses. Hearing was intact, as were facial, oropharyngeal, and tongue motor and sensory responses. Motor and sensory examination was also normal, tendon reflexes were symmetric, and toes were downgoing. At that point, the pupils were pinpoint and the patient was unresponsive with flaccid limbs. The sudden onset of bilateral impairment of eye movements on the background of clear consciousness is rare, and raised the possibility of a brainstem injury even without unconsciousness. Any activation of the anterior canal (which activates the ipsilateral superior rectus and the contralateral inferior oblique muscles) and the posterior canal (which activates the ipsilateral superior oblique and contralateral inferior rectus muscles) by caloric stimulation cancel each other out. When caloric stimulation is done in an awake patient who is trying to maintain fixation. This mnemonic can be confusing for inexperienced examiners, as the responses seen in a comatose patient with an intact brainstem are the opposite: cold water induces only tonic deviation (there is no little or no corrective nystagmus), so the eyes deviate toward the ear that is irrigated. The presence of typical vestibular nystagmus in a patient who is unresponsive indicates a psychogenic cause of unresponsiveness. The absence of a response to caloric stimulation does not always imply brainstem dysfunction. Bilateral vestibular failure occurs with phenytoin or tricyclic antidepressant toxicity. Aminoglycoside vestibular toxicity may obliterate the vestibular response, but oculocephalic responses may persist, the neck muscles supplying the afferent information. Finally, if there has been head trauma, one or more eye muscles may become trapped by a blowout fracture of the orbit. It is important to distinguish this cause of abnormal eye movements from damage to neural structures, either peripherally or centrally. This is generally done by an ophthalmologist, who applies topical anesthetics to the globe and uses a fine, toothed forceps to tug on the sclera to attempt to move the globe (forced duction). Inability to move the globe through a full range of movements may indicate a trapped muscle and requires evaluation for orbital fracture. Patient 21 A 56-year-old man with a 20-year history of poorly controlled hypertension came to the emergency department with a complaint of sudden onset of severe dizziness. On examination, he was fully Interpretation of Abnormal Ocular Movements A wide range of eye movements may be seen, both at rest and during vestibular stimulation. Each presents clues about the nature of the insult that is causing the impairment of consciousness. Table 23 lists some of the spontaneous eye movements that may be observed in unconscious patients. Most individuals have a mild degree of exophoria when drowsy and not maintaining active fixation. However, other individuals have varying types of strabismus, which may worsen as they become less responsive and no longer attempt to maintain conjugate gaze. Hence, it is very difficult to determine the meaning of dysconjugate gaze in a stuporous or comatose patient if nothing is known about the presence of baseline strabismus. On the other hand, certain types of dysconjugate eye movements raise suspicion of brainstem injury that may require further examination for confirmation. For example, injury to the oculomotor nucleus or nerve produces exodeviation of the involved eye. In skew deviation,114 in which one eye is deviated upward and the other downward, there typically is an injury to the brainstem (see below). A destructive lesion involving the frontal eye fields causes the eyes to deviate toward the side of the lesion (away from the side of the associated hemiparesis). An irritative lesion may cause deviation of the eyes away from the side of the lesion. These eye movements represent seizure activity, and often there is some evidence of quick, nystagmoid jerks toward the side of eye deviation indicative of continuing seizure activity. Hemorrhage into the thalamus may also produce ``wrong-way eyes,' which deviate away from the side of the lesion. Damage to the lateral pons, on the other hand, may cause loss of eye movements toward that side (gaze palsy, Figure 29). The lateral gaze deviation in such patients cannot be overcome by vestibular stimulation, whereas vigorous oculocephalic or caloric stimulation usually overcomes lateral gaze deviation due to a cortical gaze paresis. Absence of abduction of a single eye suggests injury to the abducens nerve either within the brainstem or along its course to the orbit. However, either increased intracranial pressure or decreased pressure, as occurs with cerebral spinal fluid leaks,121 can cause either a unilateral or bilateral abducens palsy, so the presence of an isolated abducens palsy may be misleading. Isolated loss of adduction of the eye contralateral to the head movement implies an injury to the medial longitudinal fasciculus. Bilateral lesions of the medial longitudinal fasciculus impair adduction of both eyes as well as vertical oculocephalic and vestibulo-ocular eye movements, a condition that is distinguished from bilateral oculomotor nucleus or nerve injury in the comatose patient by preservation of the pupil- lary light responses. Typically, there may also be severe ptosis on that side (so that if the patient is awake, he or she may not be aware of diplopia). In rare cases with a lesion of the oculomotor nucleus, the weakness of the superior rectus will be on the side opposite the other third nerve muscles (as these fibers are crossed) and ptosis will be bilateral (but not very severe). This occurs most often when the paresis is due to ischemia of the oculomotor nerve (the smaller pupilloconstrictor fibers are more resistant to ischemia), such as in diabetic occlusion of the vasa nervorum. Such patients are also typically awake and alert, whereas third nerve paresis due to brainstem injury or compression of the oculomotor nerve by uncal herniation results in impairment of consciousness and early pupillodilation. Trochlear nerve impairment causes a hyperopia of the involved eye, often with some exodeviation. If awake, the patient typically attempts to compensate by tilting the head toward that shoulder. Because the trochlear nerve is crossed, a trochlear palsy in a comatose patient suggests damage to the trochlear nucleus on the opposite side of the brainstem. In some cases, the eye that is elevated may alternate from side to side depending on whether the patient is looking to the left or the right. As in sleeping individuals who typically have some degree of exophoria, the eye positions may not be quite conjugate, but the ocular Examination of the Comatose Patient 71 excursions should be conjugate. Most roving eye movements are predominantly horizontal, although some vertical movements may also occur. Most patients with roving eye movements have a metabolic encephalopathy, and oculocephalic and caloric vestibulo-ocular responses are typically preserved or even hyperactive. The roving eye movements may disappear as the coma deepens, although they may persist in quite severe hepatic coma. Roving eye movements cannot be duplicated by patients who are awake, and hence their presence indicates that unresponsiveness is not psychogenic.
Generic trihexyphenidyl 2 mg with visa. What Are The Alternatives To Opioids In Treating Chronic Pain - 24/7 Helpline Call 1(800) 615-1067.
Syndromes
Effects of Sodium Intake on Blood Pressure: Evidence from MetaAnalyses of Intervention Studies myofascial pain treatment vancouver cheap 2mg trihexyphenidyl mastercard. Several meta-analyses of clinical trials have been conducted to assess the effects of sodium intake on blood pressure (Table 6-15) period pain treatment uk order 2 mg trihexyphenidyl. Typically pain medication for shingles treatment buy trihexyphenidyl 2 mg on line, these studies estimate the ratio of the average change in blood pressure to observed average change in sodium intake pain medication for dogs ibuprofen generic 2mg trihexyphenidyl visa. However pain treatment mayo clinic purchase trihexyphenidyl 2 mg on-line, such ratios cannot be used to assess dose response unless the relationship is linear back pain after treatment for uti safe 2 mg trihexyphenidyl. The earliest meta-analyses aggregated data across a wide range of study designs, from very brief feeding studies lasting a few days to long-term behavioral intervention studies lasting a year or more. These meta-analyses have provided consistent evidence that a reduced sodium intake lowers systolic and diastolic blood pressure in hypertensive individuals. However, the extent of blood pressure reduction in nonhypertensive individuals is less consistent. The corresponding reductions in systolic/diastolic blood pressures in nonhypertensive persons were 2. One meta-analysis focused on trials conducted in older-aged persons (mean age close to 60 years) (Alam and Johnson, 1999). In this meta-analysis, which included both nonhypertensive and hypertensive persons, sodium reduction significantly lowered systolic and diastolic blood pressure by 5. The effect was more pronounced in trials that exclusively enrolled individuals older than age 60. A meta-analysis was conducted to assess the effect of modest sodium reduction to levels that would be relevant to public health decision-making (He and MacGregor, 2002). Trials of brief duration and those with extremely low sodium intakes were excluded. All of the included trials lasted 4 or more weeks, and many were controlled feedings studies. Another meta-analysis assessed the long-term effects of advice to reduce sodium intake (Hooper et al. Most included trials used intensive behavioral interventions in freeliving individuals. Net reduction in urinary sodium excretion as the result of the behavioral interventions was 35. This meta-analysis documents the difficulties of sustaining a reduced sodium intake in free-living persons over the long-term. Because of the limited net reduction in sodium intake as evidenced by attained urinary sodium excretion, the efficacy of sodium reduction as a means to lower blood pressure cannot be assessed from this analysis. In Canada, approximately 27 percent of adults 35 to 64 years old have hypertension (Wolf-Maier et al. It has been estimated that almost one-third of blood pressure-related deaths from coronary heart disease are estimated to occur in individuals with blood pressure in this range (Stamler et al. The prevalence of hypertension rises progressively with age, such that more than half of all Americans 60 years of age or older have hypertension (Hajjar and Kotchen, 2003). Among nonhypertensive adults, the estimated lifetime risk of developing hypertension is 0. The rise in blood pressure with age, while commonplace in Western countries, is not universal, as there are non-Western populations, as well as some Western populations. In ecologic observational studies, a reduced intake of sodium and an increased intake of potassium have been associated with a blunted age-related rise in blood pressure (Rose et al. Hypertension can be prevented by complementary application of strategies aimed at achieving a downward shift in the distribution of blood pressure in the general population (population-based strategy) and more intensive targeted strategies aimed at achieving a greater reduction in blood pressure in individuals and groups at greater risk for high blood pressure (intensive targeted strategy) (Whelton et al. Because the health benefits of a population strategy are applied to large numbers, even small downward shifts in the distribution of blood pressure can be expected to result in a substantial reduction in the burden of illness in the population being targeted (Rose, 1985; Whelton et al. For example, a downward shift in the population distribution of systolic blood pressure by 2 mm Hg would be expected to result in an annual reduction of 6 percent in mortality from stroke and 4 percent from coronary heart disease (Stamler, 1991). The corresponding estimates would be 8 and 5 percent for a 3-mm Hg downward shift in the population distribution of systolic blood pressure, and 14 and 9 percent for a 5 mm Hg shift (Stamler, 1991). Sodium reduction is one of several nutritional therapies that have been proposed as a means to reduce blood pressure and thereby affect a downward shift of blood pressure in the population (Chobanian et al. Each study was a controlled trial in which there was a behavioral intervention that focused exclusively on reducing sodium intake. As shown in Table 6-16, net reductions in urinary sodium excretion on the sodium reduction arm were modest in the three studies, ranging from 13 to 57 mmol/day, at the end of follow-up. In this setting, the relative risk of incident hypertension associated with a reduced sodium intervention that did not include any other lifestyle change ranged from 0. At 6 months, the height of intervention adherence, the incidence of hypertension was lowest in the combined group (2. By the end of follow-up, the incidence of hypertension was 18 to 22 percent less in each behavioral intervention group (p < 0. Results of this trial indicate that behavioral interventions can prevent hypertension over the long-term. Also, the pattern of incident hypertension at 6 and 18 months suggests that the effects of weight loss and reduced sodium intake, under optimal conditions of adherence, may be additive. It is important to note that a major barrier to the achievement of greater reductions in blood pressure and reductions in the associated cardiovascular disease complications is reliance on behavioral interventions to reduce dietary intake of sodium. Given the current market availability of lowersodium food products, careful selection is necessary to lower sodium intake. Stroke and Coronary Heart Disease A strong positive association between salt intake and cardiovascular disease, especially stroke, has been documented in a variety of animal models (Chen et al. In Japan, a public health campaign to reduce average dietary sodium intake was associated with a significant reduction in the prevalence of hypertension and hemorrhagic stroke, a major cause of death in this population before sodium intake decreased (Yamori and Horie, 1994). Increased sodium intake has also been associated with increased left ventricular mass, a subclinical form of cardiovascular disease (Liebson et al. Results of prospective studies have been less consistent, primarily because of methodological limitations. Early reports did not find a significant relationship between dietary sodium intake and risk of stroke (Kagan et al. To a large extent, inadequate power reflects the imprecision associated with most approaches to the measurement of habitual sodium intake. In particular, a high ratio of intraindividual to interindividual variation in sodium intake, which is commonplace in westernized populations (Liu et al. Two epidemiological studies published by Alderman and coworkers (1995, 1998b) have been interpreted as providing evidence that low sodium diets have an adverse effect on human health. In the first of these studies, Alderman and colleagues (1995) reported the presence of a significant inverse association between urinary sodium excretion and incident myocardial infarction in a prospective cohort study conducted in 2,937 treated hypertensive patients. As indicated in an accompanying editorial and in subsequent communications, however, the assessment of sodium intake and imprecision in the measurement of potentially confounding variables might have contributed to the occurrence of this unexpected finding (Cook et al. Urinary sodium excretion as obtained and reported in this study did not represent habitual dietary sodium intake. First, participants were advised to reduce their sodium intake prior to the collection of urine. The relationship between urinary sodium excretion and myocardial infarction was inverse in men, but direct in women. Plasma renin concentrations did not increase proportionately to the reduction in sodium excretion as might be anticipated. Also, the study was conducted in hypertensive patients who were enrolled in a work-site treatment program, making it difficult to know whether the findings would have general application. While the authors have responded to these concerns (Alderman and Laragh, 1996), interpretation of the findings from this study remains difficult. They identified an inverse relationship between sodium intake and mortality from cardiovascular diseases (p = 0. In addition to the inconsistency between the direction of the association with the two methods of estimating sodium intake (directly, or as adjusted based on estimated energy intake), several methodological concerns make it difficult to interpret the findings. Participants with a baseline history of cardiovascular diseases were included in the main analysis, albeit such participants might be expected to have changed their dietary intake of sodium prior to dietary assessment. Acute rheumatic fever, chronic rheumatic heart disease, and diseases of the pulmonary circulation were included as cardiovascular mortality outcomes, although the biological basis for a relationship between sodium intake and these diseases is not obvious. As in the prior report by Alderman and colleagues, there is again evidence of differential completeness of dietary data. Of greatest concern is the fact that the highly correlated variables of sodium intake, caloric intake, and sodium:calorie ratio were simultaneously included in the same multivariate model. Several epidemiological and clinical studies have suggested that overweight persons may be more sensitive to the effects of sodium on blood pressure (Altschul et al. In this setting, two prospective studies examined the effects of sodium intake on cardiovascular outcomes in analyses stratified by overweight status (He et al. In contrast to previous analyses using the same database reported by Alderman and colleagues (1998b), He and colleagues (1999) excluded those individuals with a history of cardiovascular disease or its treatment and those who intentionally consumed a low-salt diet. As estimated from a single 24-hour dietary recall that did not include discretionary salt use, baseline median sodium intake in the quintiles (based on the sodium-energy ratio) ranged from 1. In the overweight stratum, there were consistent and highly significant positive relationships between baseline dietary intake of sodium and risk of stroke, cardiovascular disease, and total mortality. Dietary sodium intake was not significantly associated with nonfatal coronary heart disease in overweight participants or with risk of cardiovascular disease in participants with normal weight. In a prospective study conducted in 1,173 Finnish men and 1,263 women aged 25 to 64 years, the adjusted hazard ratios for coronary heart disease, cardiovascular disease, and all-cause mortality, associated with a 100 mmol (2. Overall, observational studies, particularly ecological studies, suggest that higher levels of sodium intake increase the risk of cardiovascular disease, especially stroke. Of the available prospective observational studies, those with the most rigorous methods have likewise documented a positive relationship, which was evident in overweight individuals. Still, conclusive evidence of a causal relationship typically depends on results of appropriately designed clinical trials that test the effects of sodium reduction on clinical cardiovascular outcomes. While some persons have advocated such a trial, the feasibility of such an endeavor is uncertain, especially in view of the well-documented difficulties in establishing and maintaining a large contrast in sodium intake over the long-term (Table 6-16). Left Ventricular Mass Increased left ventricular mass or wall thickness (left ventricular hypertrophy) is a subclinical form of cardiovascular disease that is a powerful predictor of cardiovascular morbidity and mortality, including myocardial infarction, stroke, congestive heart failure, and sudden death (Bikkina et al. Echocardiography is a sensitive diagnostic technique that is used to estimate left ventricular mass. The 5-year mortality for electrocardiographic left ventricular hypertrophy was 33 percent for men and 21 percent for women (Kannel, 1991). Increased left ventricular mass is thought to be, in part, a structural adaptation of the heart as a compensatory mechanism for increased blood pressure and wall stress. Increased blood pressure is one of the strongest correlates of left ventricular mass (Liebson et al. Not surprisingly, factors associated with elevated blood pressure are also associated with increased left ventricular mass, including obesity (de Simone et al. Several cross-sectional studies have examined the relationship between sodium intake, typically as measured by urinary sodium excretion, and left ventricular mass or hypertrophy, as measured by echocardiography. Other cross-sectional studies have documented associations between sodium intake and cardiac function, such as impaired diastolic filling (Langenfeld et al. Most reports used correlation or regression analyses and did not report left ventricular mass by level of urinary sodium excretion. Available studies predominantly enrolled hypertensive adults, but some enrolled nonhypertensive individuals (du Cailar et al. With the exception of the study by Alderman and colleagues, which assessed left ventricular hypertrophy by electrocardiography and did not detect an association, each study documented a statistically significant, positive relationship between urinary sodium excretion and left ventricular mass (Daniels et al. Figure 6-6 displays results from the report of Schmieder and coworkers (1988), who were the first to report an association between sodium intake and left ventricular hypertrophy. The only two studies that reported left ventricular mass by level of dietary sodium are included in Table 6-18. In most studies, the association between urinary sodium excretion and left ventricular mass persisted after adjustment for other determinants of left ventricular mass, including blood pressure (du Cailar et al. Potential mechanistic pathways by which sodium might exert a direct effect on left ventricular mass include the renin-angiotensin system, the sympathetic nervous system, and fluid-volume homeostasis (Beil et al. Four clinical trials assessed the effects of a reduced sodium intake on left ventricular mass in hypertensive individuals. In three trials, the comparison group received antihypertensive drug therapy (Fagerberg et al. In two of these trials, the nonpharmacological intervention included weight loss, as well as sodium reduction (Fagerberg et al. In each of the three trials with an active drug treatment comparison group, reductions in left ventricular mass were similar in the pharmacological and nonpharmacological intervention groups. In view of the well-documented effects of antihypertensive drug therapy on left ventricular mass in controlled trials (Klingbeil et al. However, because two of the trials included weight loss in the nonpharmacological interventions, one cannot attribute the effects to a reduced sodium intake. Only one trial tested a reduced sodium intervention and compared its effects with that of a nonintervention control group (Jula and Karanko, 1994). In this randomized trial that enrolled 76 hypertensive individuals, mean urinary sodium excretion decreased from 195 mmol (4. In summary, available data from cross-sectional studies in hypertensive individuals are consistent in documenting a progressive, direct, and independent relationship between sodium intake and left ventricular mass. Furthermore, sodium may have a direct effect apart from an indirect effect mediated through blood pressure. While one controlled trial suggests that the association between sodium intake and left ventricular mass is causal, additional trials are needed. Calcium Excretion, Bone Mineral Density, and Kidney Stones Numerous intervention studies have demonstrated that increased sodium chloride intake induces a substantial increase in the urinary excretion of calcium (Table 6-19). Sodium chloride-induced hypercalciuria also appears to be accompanied by an increased intestinal calcium absorption (Breslau et al.